Introduction
Throat symptoms or complaints refer to any discomfort, pain, or abnormal sensations experienced in the throat. These symptoms can be caused by various factors, including infections, allergies, acid reflux, or structural abnormalities.[1] This guide aims to provide an overview of the symptoms, causes, diagnostic steps, possible interventions, and patient education related to throat symptoms.
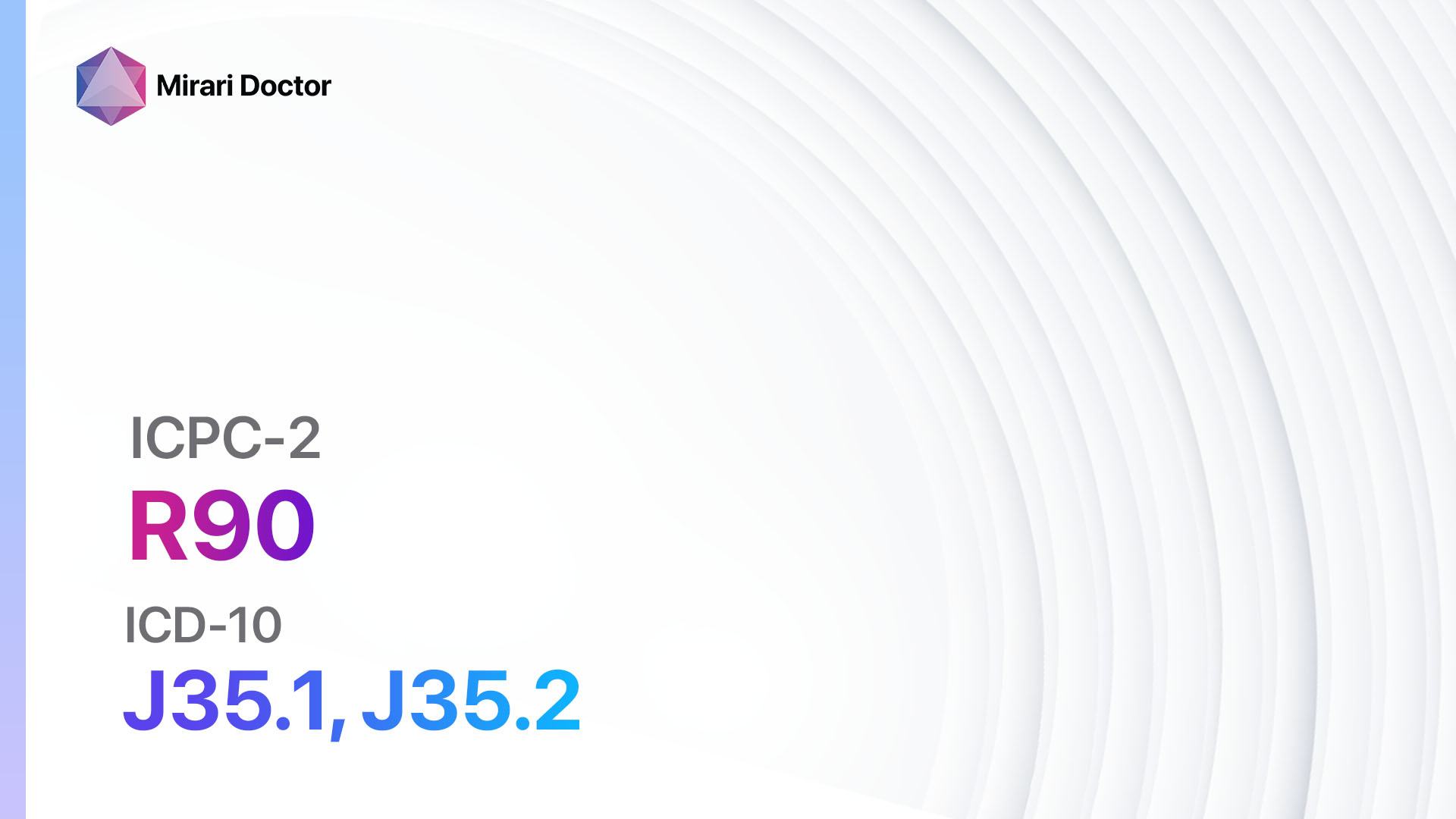
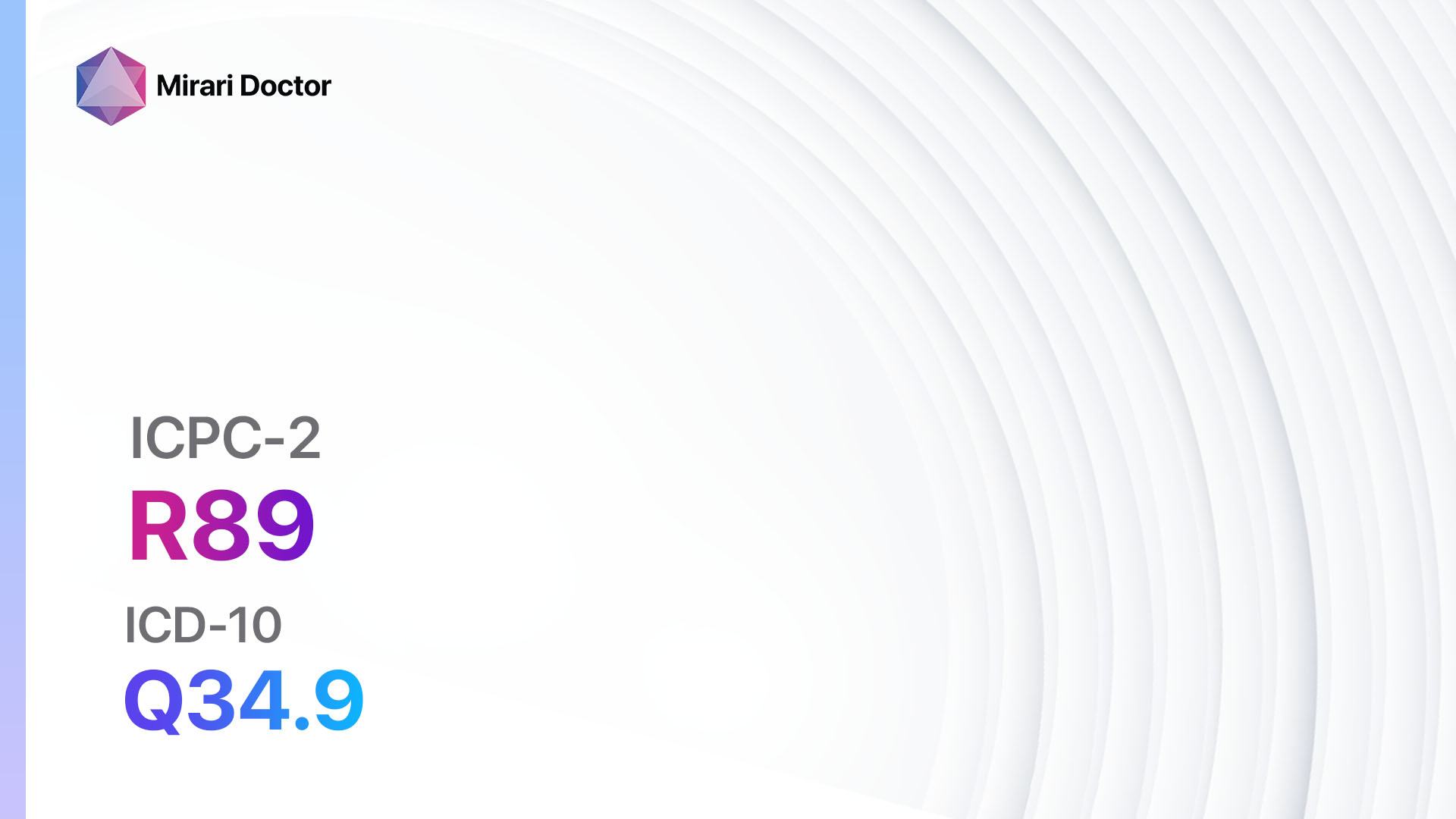
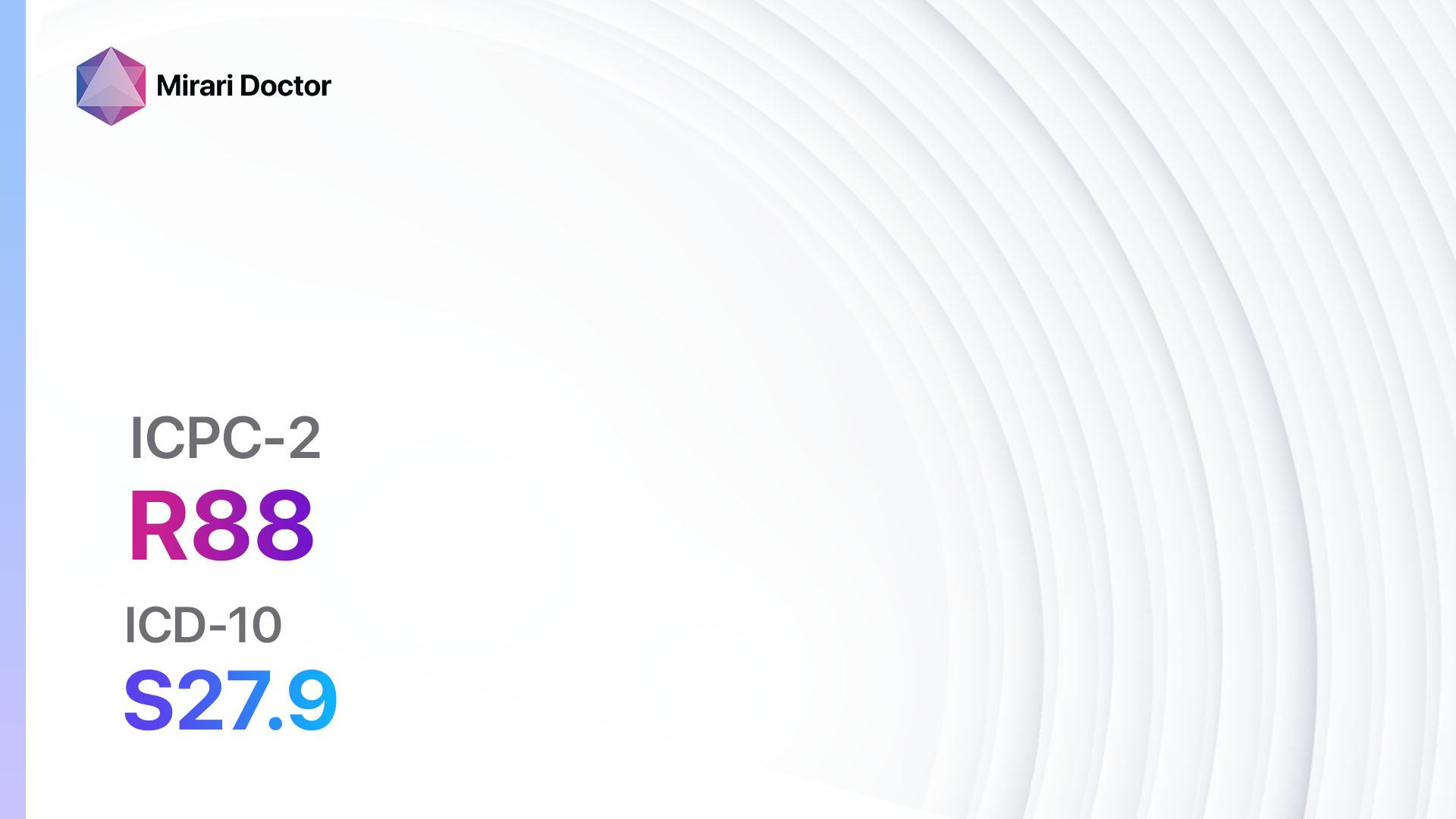
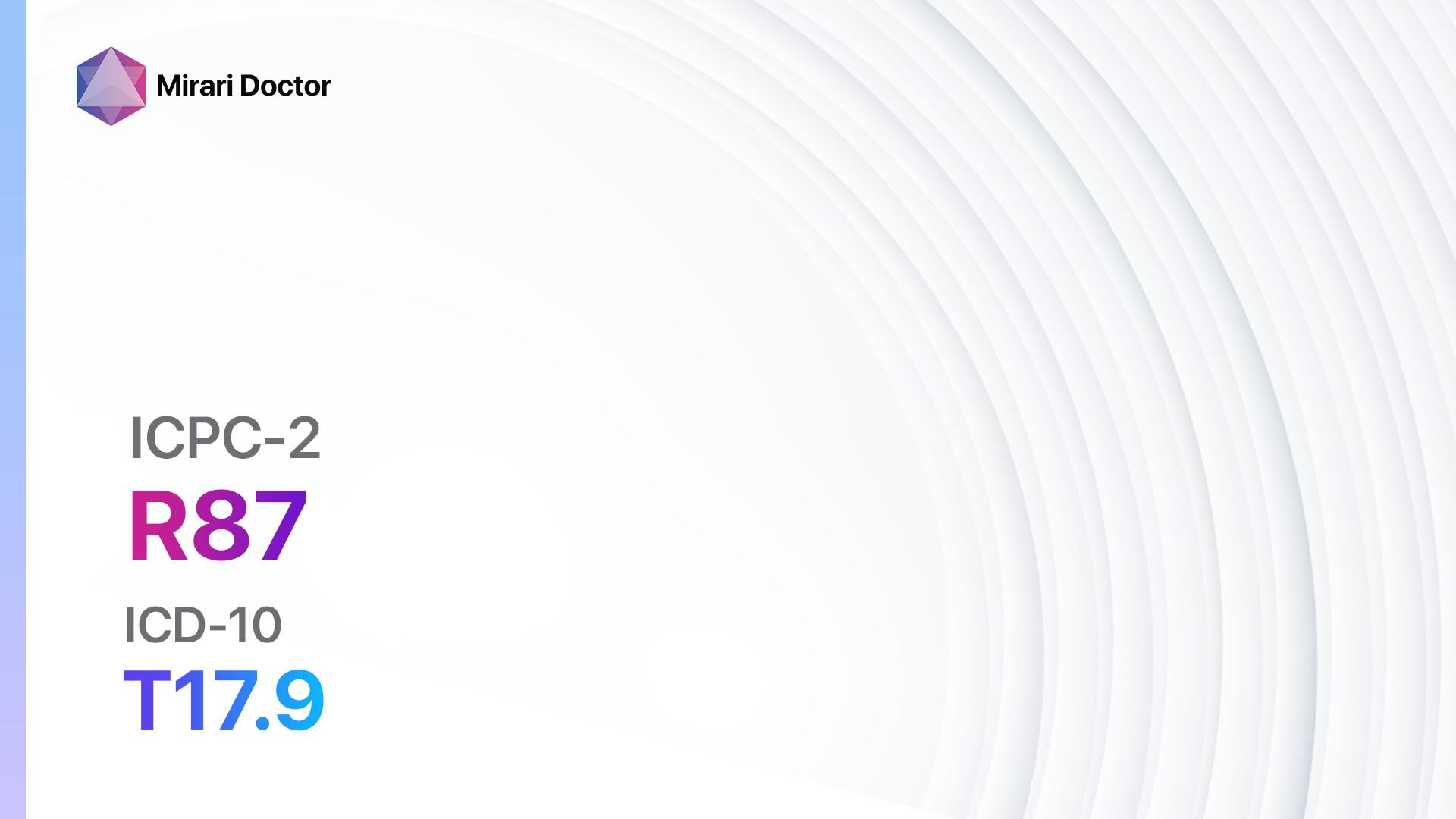
Codes
Symptoms
- Sore throat: Pain or discomfort in the throat, especially when swallowing.[2]
- Hoarseness: Changes in the voice, such as a raspy or strained voice.[3]
- Difficulty swallowing: Feeling of obstruction or discomfort when swallowing.
- Throat irritation: Persistent itching or tickling sensation in the throat.
- Swollen tonsils: Enlarged tonsils that may be accompanied by pain or difficulty breathing.[4]
- Cough: Persistent cough that may be dry or accompanied by phlegm.
- Bad breath: Unpleasant odor coming from the mouth or throat.
- Throat congestion: Feeling of mucus or phlegm in the throat.
- Throat pain: Sharp or dull pain in the throat, especially when swallowing or talking.
- Redness or inflammation: Visible redness or swelling in the throat.[5]
Causes
- Viral infections: Common cold, flu, or mononucleosis.[6]
- Bacterial infections: Streptococcal infection (strep throat), tonsillitis, or diphtheria.
- Allergies: Allergic rhinitis or postnasal drip.
- Gastroesophageal reflux disease (GERD): Acid reflux from the stomach into the throat.[7]
- Environmental irritants: Smoking, pollution, or dry air.
- Structural abnormalities: Enlarged tonsils, deviated septum, or nasal polyps.
- Voice strain: Excessive use of the voice or shouting.
- Foreign body: Presence of a foreign object in the throat.
- Cancer: Throat cancer or laryngeal cancer.[8]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration, severity, and any associated factors.
- Ask about any previous medical conditions, allergies, or surgeries.
- Inquire about lifestyle factors, such as smoking or exposure to environmental irritants.
- Assess the patient’s risk factors for infections or cancer, such as recent travel or family history.[9]
Physical Examination
- Inspect the throat for redness, swelling, or visible abnormalities.
- Palpate the neck to check for swollen lymph nodes.
- Use a tongue depressor to examine the tonsils and back of the throat.
- Evaluate the patient’s voice quality and assess for hoarseness.[10]
Laboratory Tests
- Rapid strep test: A throat swab to test for streptococcal infection.
- Complete blood count (CBC): To check for signs of infection or inflammation.
- Monospot test: To diagnose mononucleosis.
- Throat culture: To identify the presence of bacteria or fungi.
- Allergy testing: To determine if allergies are contributing to throat symptoms.
Diagnostic Imaging
- X-ray: To assess for structural abnormalities or foreign bodies in the throat.
- CT scan: Provides detailed images of the throat and surrounding structures.
- MRI: Useful for evaluating soft tissue abnormalities or tumors in the throat.
Other Tests
- Esophagoscopy: A flexible tube with a camera is inserted through the mouth to examine the throat and esophagus.
- Laryngoscopy: A thin tube with a camera is inserted through the nose or mouth to visualize the larynx.
- Biopsy: Removal of a small tissue sample for laboratory analysis to diagnose cancer or other abnormalities.
Follow-up and Patient Education
- Provide the patient with a clear explanation of the diagnosis and treatment plan.
- Discuss the importance of completing any prescribed medications or interventions.
- Educate the patient about lifestyle modifications to prevent recurrence or worsening of symptoms.
- Schedule follow-up appointments to monitor the patient’s progress and adjust treatment if necessary.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for throat symptoms:
- Antibiotics (e.g., Amoxicillin, Azithromycin):
- Cost: Generic versions can be $3-$50/month.
- Contraindications: Allergy to antibiotics, liver disease.
- Side effects: Upset stomach, diarrhea, rash.
- Severe side effects: Severe allergic reactions, liver damage.
- Drug interactions: Warfarin, oral contraceptives.
- Warning: Complete the full course of antibiotics as prescribed.
- Pain relievers (e.g., Acetaminophen, Ibuprofen):
- Cost: Over-the-counter options are inexpensive. Prescription-strength may range from $10-$50/month.
- Contraindications: Allergy to pain relievers, history of stomach ulcers.
- Side effects: Upset stomach, dizziness, rash.
- Severe side effects: Severe allergic reactions, liver or kidney damage.
- Drug interactions: Blood thinners, other pain relievers.
- Warning: Follow the recommended dosage and avoid exceeding the maximum daily limit.
- Antihistamines (e.g., Loratadine, Cetirizine):
- Cost: Generic versions can be $5-$20/month.
- Contraindications: Allergy to antihistamines, narrow-angle glaucoma.
- Side effects: Drowsiness, dry mouth, blurred vision.
- Severe side effects: Irregular heartbeat, difficulty urinating.
- Drug interactions: Sedatives, alcohol.
- Warning: Some antihistamines may cause drowsiness, so avoid driving or operating machinery if affected.
- Proton pump inhibitors (e.g., Omeprazole, Esomeprazole):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Allergy to proton pump inhibitors, liver disease.
- Side effects: Headache, diarrhea, abdominal pain.
- Severe side effects: Severe allergic reactions, kidney damage.
- Drug interactions: Warfarin, clopidogrel.
- Warning: Take the medication as directed, usually before meals.
- Corticosteroids (e.g., Prednisone, Dexamethasone):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Allergy to corticosteroids, active infections.
- Side effects: Increased appetite, weight gain, mood changes.
- Severe side effects: Adrenal suppression, osteoporosis.
- Drug interactions: NSAIDs, anticoagulants.
- Warning: Follow the prescribed dosage and duration, as abrupt discontinuation can cause withdrawal symptoms.
Surgical Procedures:
- Tonsillectomy: Surgical removal of the tonsils. Cost: $3,000 to $6,000.
- Adenoidectomy: Surgical removal of the adenoids. Cost: $3,000 to $6,000.
- Vocal cord surgery: Surgical procedures to correct voice disorders. Cost: $5,000 to $10,000.
Alternative Interventions
- Herbal remedies: Throat lozenges or teas containing ingredients like honey, ginger, or slippery elm. Cost: Varies depending on the specific product.
- Saltwater gargles: Mix 1/4 to 1/2 teaspoon of salt in 8 ounces of warm water and gargle several times a day. Cost: Minimal, as salt is readily available.
- Steam inhalation: Inhaling steam from a bowl of hot water or using a humidifier to soothe the throat. Cost: Minimal, as hot water is readily available.
- Honey and lemon: Mix honey and lemon juice in warm water and drink to soothe the throat. Cost: Minimal, as honey and lemon are readily available.
- Throat sprays or numbing lozenges: Over-the-counter products that provide temporary relief of throat pain. Cost: Varies depending on the specific product.
Lifestyle Interventions
- Stay hydrated: Drink plenty of fluids to keep the throat moist. Cost: Minimal, as water is readily available.
- Avoid irritants: Limit exposure to smoke, pollution, and other environmental irritants. Cost: Minimal, as it involves avoiding certain environments.
- Rest the voice: Avoid excessive talking or shouting to allow the throat to heal. Cost: Minimal, as it involves modifying behavior.
- Use a humidifier: Add moisture to the air to prevent dryness in the throat. Cost: $20-$100 for a basic humidifier.
- Practice good oral hygiene: Brushing teeth and tongue regularly to reduce bacteria in the mouth and throat. Cost: Minimal, as it involves maintaining regular oral hygiene practices.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R21 Throat symptom/complaint (ICD-10:R07.0)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Throat symptom/complaint effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Throat symptom/complaint. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Renner B, Mueller CA, Shephard A. Environmental and non-infectious factors in the aetiology of pharyngitis (sore throat). Inflamm Res. 2012;61(10):1041-1052.
- Stead W. Patient education: Sore throat in adults (Beyond the Basics). UpToDate. 2021.
- Schwartz SR, Cohen SM, Dailey SH, et al. Clinical practice guideline: hoarseness (dysphonia). Otolaryngol Head Neck Surg. 2009;141(3 Suppl 2):S1-S31.
- Bathala S, Eccles R. A review on the mechanism of sore throat in tonsillitis. J Laryngol Otol. 2013;127(3):227-232.
- Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55(10):1279-1282.
- Wessels MR. Clinical practice. Streptococcal pharyngitis. N Engl J Med. 2011;364(7):648-655.
- Kahrilas PJ, Smith JA, Dicpinigaitis PV. A causal relationship between cough and gastroesophageal reflux disease (GERD) has been established: a pro/con debate. Lung. 2014;192(1):39-46.
- Marur S, Forastiere AA. Head and Neck Squamous Cell Carcinoma: Update on Epidemiology, Diagnosis, and Treatment. Mayo Clin Proc. 2016;91(3):386-396.
- Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):e72-e112.
- Couch ME, Zanation AM. Diseases of the oral cavity, pharynx, and esophagus. In: Flint PW, Haughey BH, Lund VJ, et al., eds. Cummings Otolaryngology: Head and Neck Surgery. 6th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 69.
Related articles
Made in USA