Introduction
Sinusitis is a common condition characterized by inflammation of the sinuses, which are air-filled cavities in the skull. It can be acute or chronic, with acute sinusitis lasting less than 4 weeks and chronic sinusitis lasting longer than 12 weeks.[1]Sinusitis can cause significant discomfort and affect a person’s quality of life. The aim of this guide is to provide an overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for sinusitis.
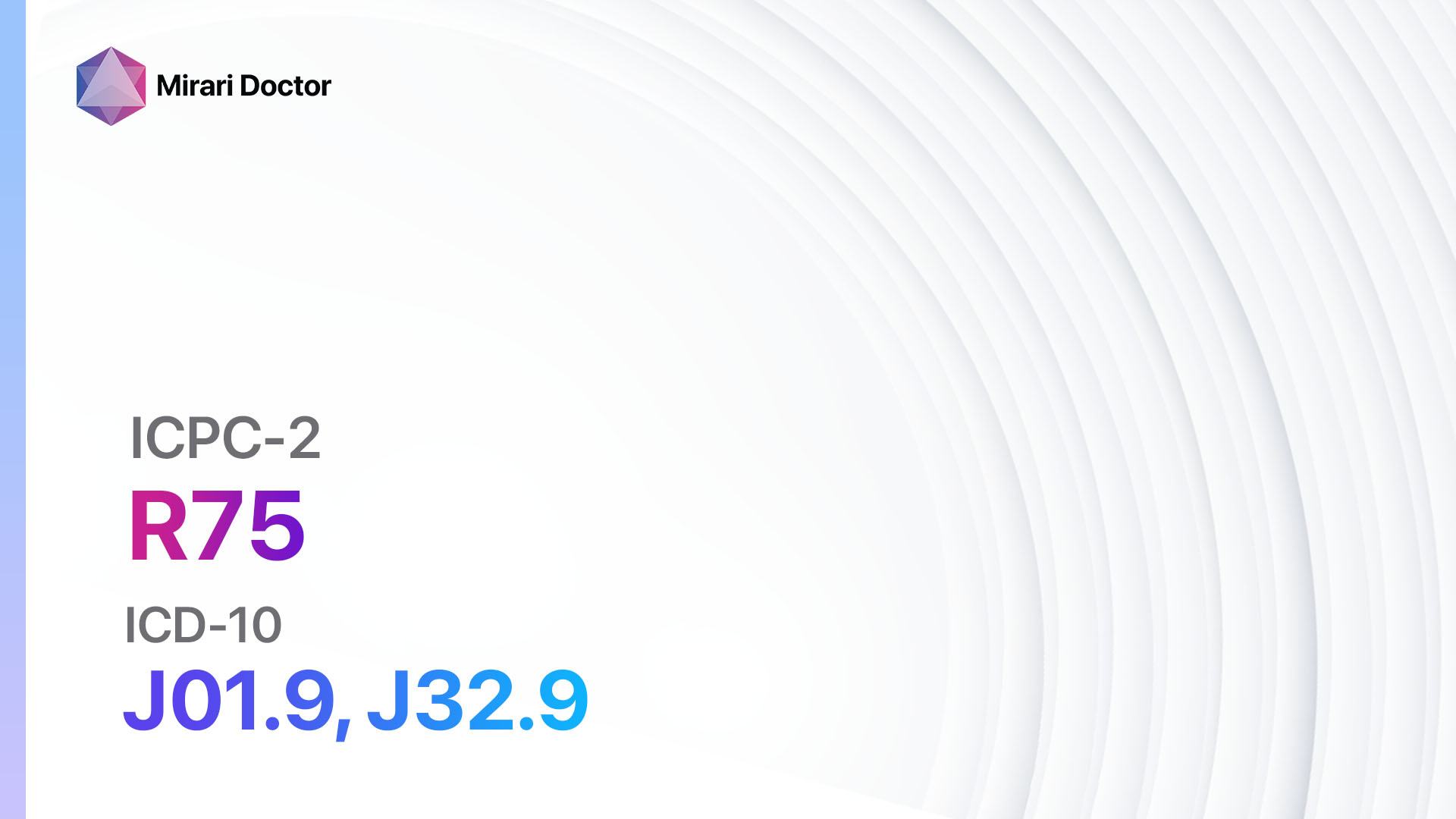
Codes
- ICPC-2 Code: R75 Sinusitis acute/chronic
- ICD-10 Code: J01.9 Acute sinusitis, unspecified, J32.9 Chronic sinusitis, unspecified[2]
Symptoms
- Facial pain or pressure: Patients may experience pain or pressure in the face, particularly around the cheeks, forehead, and eyes.
- Nasal congestion: The nasal passages may feel blocked or congested, making it difficult to breathe through the nose.
- Nasal discharge: Patients may have thick, discolored nasal discharge, which may be yellow or green.
- Loss of smell: Sinusitis can cause a reduced sense of smell or complete loss of smell.
- Headache: Patients may experience headaches, particularly in the forehead or around the eyes.
- Cough: Sinusitis can cause a persistent cough, which may worsen at night.
- Fatigue: Patients may feel tired or fatigued due to the inflammation and congestion in the sinuses.
- Bad breath: Sinusitis can cause bad breath, also known as halitosis.
- Tooth pain: In some cases, sinusitis can cause pain in the upper teeth.[3][4]
Causes
- Viral infection: The most common cause of acute sinusitis is a viral infection, such as the common cold or influenza.
- Bacterial infection: In some cases, acute sinusitis may be caused by a bacterial infection, typically following a viral infection.
- Allergies: Chronic sinusitis can be caused by allergies, such as hay fever or allergic rhinitis.
- Nasal polyps: Nasal polyps are growths that can develop in the nasal passages and contribute to chronic sinusitis.
- Deviated septum: A deviated septum, which is a shift in the nasal septum, can obstruct the sinuses and lead to chronic sinusitis.
- Immune system disorders: Certain immune system disorders, such as HIV/AIDS or cystic fibrosis, can increase the risk of sinusitis.[5][6]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration, severity, and progression of symptoms.
- Ask about any previous episodes of sinusitis or other respiratory conditions.
- Inquire about any known risk factors, such as allergies or immune system disorders.
- Assess the impact of sinusitis on the patient’s daily activities and quality of life.[7]
Physical Examination
- Inspect the nasal passages for signs of inflammation, such as redness or swelling.
- Palpate the sinuses to check for tenderness or pain.
- Evaluate the patient’s sense of smell.
- Examine the throat and ears for any signs of infection or inflammation.[8]
Laboratory Tests
- Nasal swab: A swab of the nasal discharge may be taken to identify the presence of bacteria or viruses.
- Blood tests: Blood tests can help determine if there is an underlying immune system disorder or other systemic condition contributing to sinusitis.[9]
Diagnostic Imaging
- X-ray: X-rays can provide a basic view of the sinuses and help identify any blockages or abnormalities.
- CT scan: CT scans provide a more detailed view of the sinuses and can help identify the extent of inflammation or any structural abnormalities.
- MRI: MRI scans may be used in certain cases to evaluate the sinuses and surrounding structures in more detail.[10]
Other Tests
- Allergy testing: Allergy testing may be recommended if allergies are suspected as a cause of chronic sinusitis.
- Nasal endoscopy: A thin, flexible tube with a light and camera may be inserted into the nasal passages to visualize the sinuses and identify any abnormalities or polyps.
Follow-up and Patient Education
- Schedule a follow-up appointment to assess the patient’s response to treatment and make any necessary adjustments.
- Provide education on sinusitis management, including proper nasal hygiene, the use of saline nasal rinses, and the importance of completing the full course of prescribed medications.
- Discuss strategies for preventing future episodes of sinusitis, such as avoiding known triggers and managing allergies effectively.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Sinusitis acute/chronic:
- Antibiotics (e.g., Amoxicillin, Augmentin, Azithromycin):
- Cost: Generic versions can be $3-$50/month.
- Contraindications: Allergy to penicillin or macrolide antibiotics.
- Side effects: Nausea, diarrhea, rash.
- Severe side effects: Severe allergic reactions, liver damage.
- Drug interactions: Warfarin, oral contraceptives.
- Warning: Complete the full course of antibiotics as prescribed.
- Nasal corticosteroids (e.g., Fluticasone, Budesonide):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: None.
- Side effects: Nasal irritation, nosebleeds.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Regular use is necessary for optimal effectiveness.
- Decongestants (e.g., Pseudoephedrine, Phenylephrine):
- Cost: Generic versions can be $5-$20/month.
- Contraindications: Uncontrolled high blood pressure, heart disease.
- Side effects: Increased heart rate, elevated blood pressure.
- Severe side effects: None reported.
- Drug interactions: MAO inhibitors, beta-blockers.
- Warning: Limit use to short-term relief (3-7 days).
- Antihistamines (e.g., Loratadine, Cetirizine):
- Cost: Generic versions can be $5-$20/month.
- Contraindications: Glaucoma, urinary retention.
- Side effects: Drowsiness, dry mouth.
- Severe side effects: None reported.
- Drug interactions: Sedatives, alcohol.
- Warning: Non-drowsy formulations are available.
- Saline nasal rinses:
- Cost: Over-the-counter kits can range from $5-$20.
- Contraindications: None.
- Side effects: Nasal irritation, discomfort.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Follow proper technique for safe and effective use.
Alternative Drugs:
- Mucolytics (e.g., Guaifenesin): Can help thin and loosen mucus in the sinuses.
- Oral corticosteroids (e.g., Prednisone): May be prescribed for severe or chronic sinusitis.
- Antifungal medications (e.g., Fluconazole): Used in cases of fungal sinusitis.
- Leukotriene modifiers (e.g., Montelukast): Can help reduce inflammation in the sinuses.
Surgical Procedures:
- Functional endoscopic sinus surgery (FESS): A minimally invasive procedure to remove blockages or polyps in the sinuses. Cost: $5,000 to $15,000.
- Balloon sinuplasty: A procedure that uses a small balloon to open up blocked sinuses. Cost: $3,000 to $7,000.
Alternative Interventions
- Acupuncture: May help reduce sinus inflammation and improve symptoms. Cost: $60-$120 per session.
- Nasal irrigation: Using a neti pot or nasal irrigation bottle to rinse the sinuses with saline solution. Cost: $10-$20 for a neti pot or irrigation bottle.
- Steam inhalation: Inhaling steam from a bowl of hot water or using a steam inhaler to help relieve congestion. Cost: $20-$50 for a steam inhaler.
- Herbal supplements: Certain herbs, such as Echinacea or goldenseal, may have potential benefits for sinusitis. Cost: Varies depending on the specific supplement.
- Probiotics: Some studies suggest that certain strains of probiotics may help reduce the frequency and severity of sinusitis. Cost: Varies depending on the specific probiotic supplement.
Lifestyle Interventions
- Nasal hygiene: Regularly cleaning the nasal passages with saline solution or nasal sprays to help reduce congestion and prevent infection. Cost: $5-$15 for saline nasal sprays.
- Humidification: Using a humidifier or steam vaporizer to add moisture to the air and help relieve sinus congestion. Cost: $20-$100 for a humidifier.
- Avoiding triggers: Identifying and avoiding triggers that worsen sinusitis symptoms, such as allergens or irritants.
- Quitting smoking: Smoking can worsen sinusitis symptoms and delay healing. Cost: Varies depending on the method used for smoking cessation.
- Maintaining a healthy diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can support overall immune health. Cost: Varies depending on individual food choices.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. It is recommended to consult with a healthcare professional for personalized treatment recommendations and cost estimates.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment:Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies:Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort:Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection:Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R75 Sinusitis acute/chronic (ICD-10:J01.9, J32.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Modesetting:7 (Immunotherapy) Location:4(Heart,Bile& Pancreas) Morning:15minutes, Evening:15minutes | Modesetting:7 (Immunotherapy) Location:4(Heart,Bile& Pancreas) Morning:30minutes, Lunch:30minutes, Evening:30minutes | Modesetting:7 (Immunotherapy) Location:4(Heart,Bile& Pancreas) Morning:30minutes, Lunch:30minutes, Evening:30minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD | Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD | Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD | Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD |
 |
|
Use the Mirari Cold Plasma device to treat Sinusitis acute/chronic effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Sinusitis acute/chronic. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Rosenfeld RM, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 Suppl):S1-S39.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). 2019.
- Aring AM, Chan MM. Acute Rhinosinusitis in Adults. Am Fam Physician. 2011;83(9):1057-1063.
- Fokkens WJ, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology. 2020;58(Suppl S29):1-464.
- Hamilos DL. Chronic rhinosinusitis: Epidemiology and medical management. J Allergy Clin Immunol. 2011;128(4):693-707.
- Orlandi RR, et al. International Consensus Statement on Allergy and Rhinology: Rhinosinusitis. Int Forum Allergy Rhinol. 2016;6 Suppl 1:S22-S209.
- Bhattacharyya N. Clinical and symptom criteria for the accurate diagnosis of chronic rhinosinusitis. Laryngoscope. 2006;116(7 Pt 2 Suppl 110):1-22.
- Benninger MS, et al. Adult chronic rhinosinusitis: Definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg. 2003;129(3 Suppl):S1-32.
- Desrosiers M, et al. Canadian clinical practice guidelines for acute and chronic rhinosinusitis. J Otolaryngol Head Neck Surg. 2011;40 Suppl 2:S99-193.
- Lund VJ, Mackay IS. Staging in rhinosinusitus. Rhinology. 1993;31(4):183-184.
Related articles
Made in USA