Introduction
Chronic bronchitis is a long-term inflammation of the bronchial tubes, which carry air to and from the lungs. It is a type of chronic obstructive pulmonary disease (COPD) and is characterized by a persistent cough that produces mucus.[1]This guide aims to provide an overview of chronic bronchitis, including its symptoms, causes, diagnostic steps, possible interventions, and lifestyle modifications.
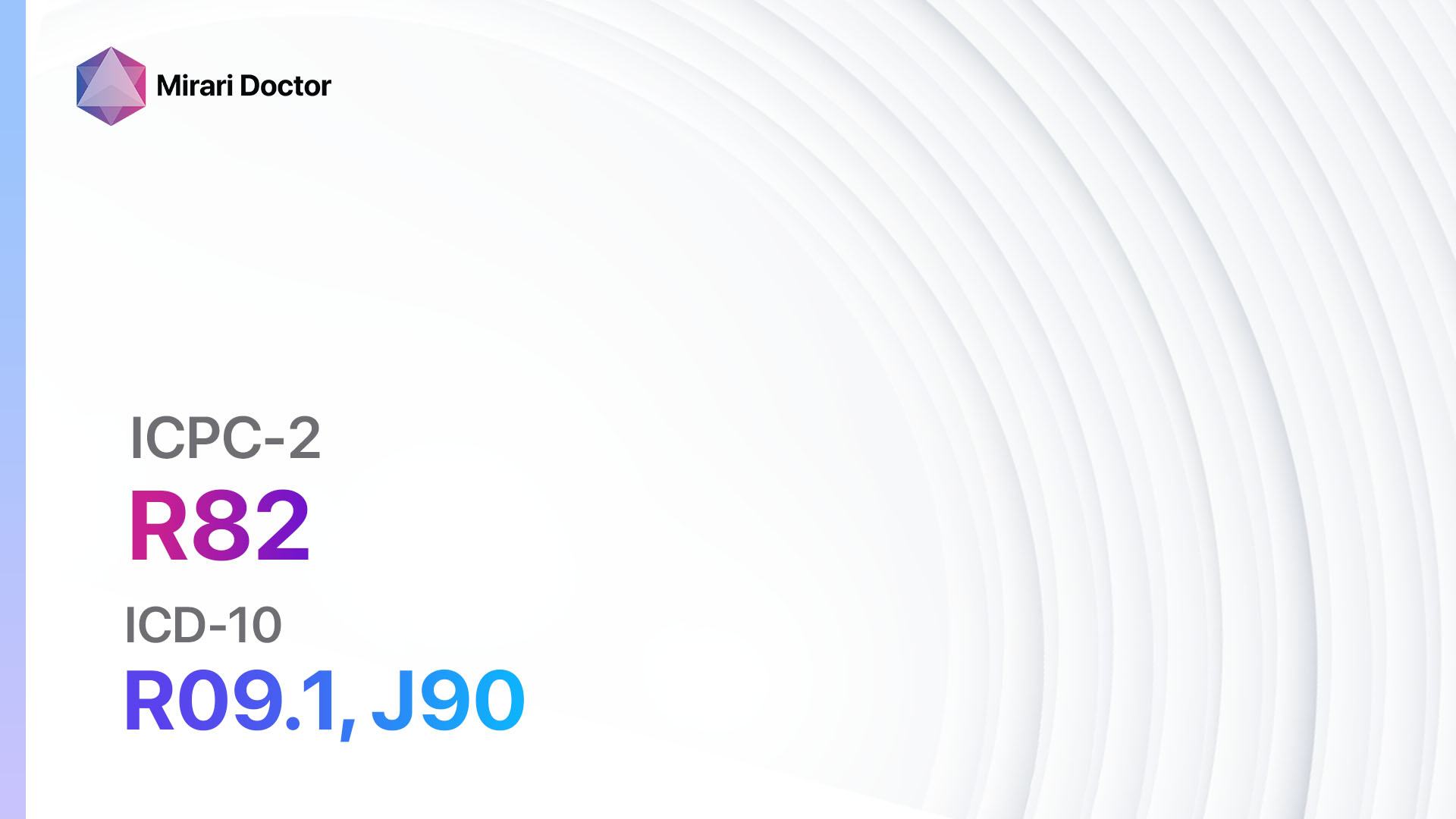
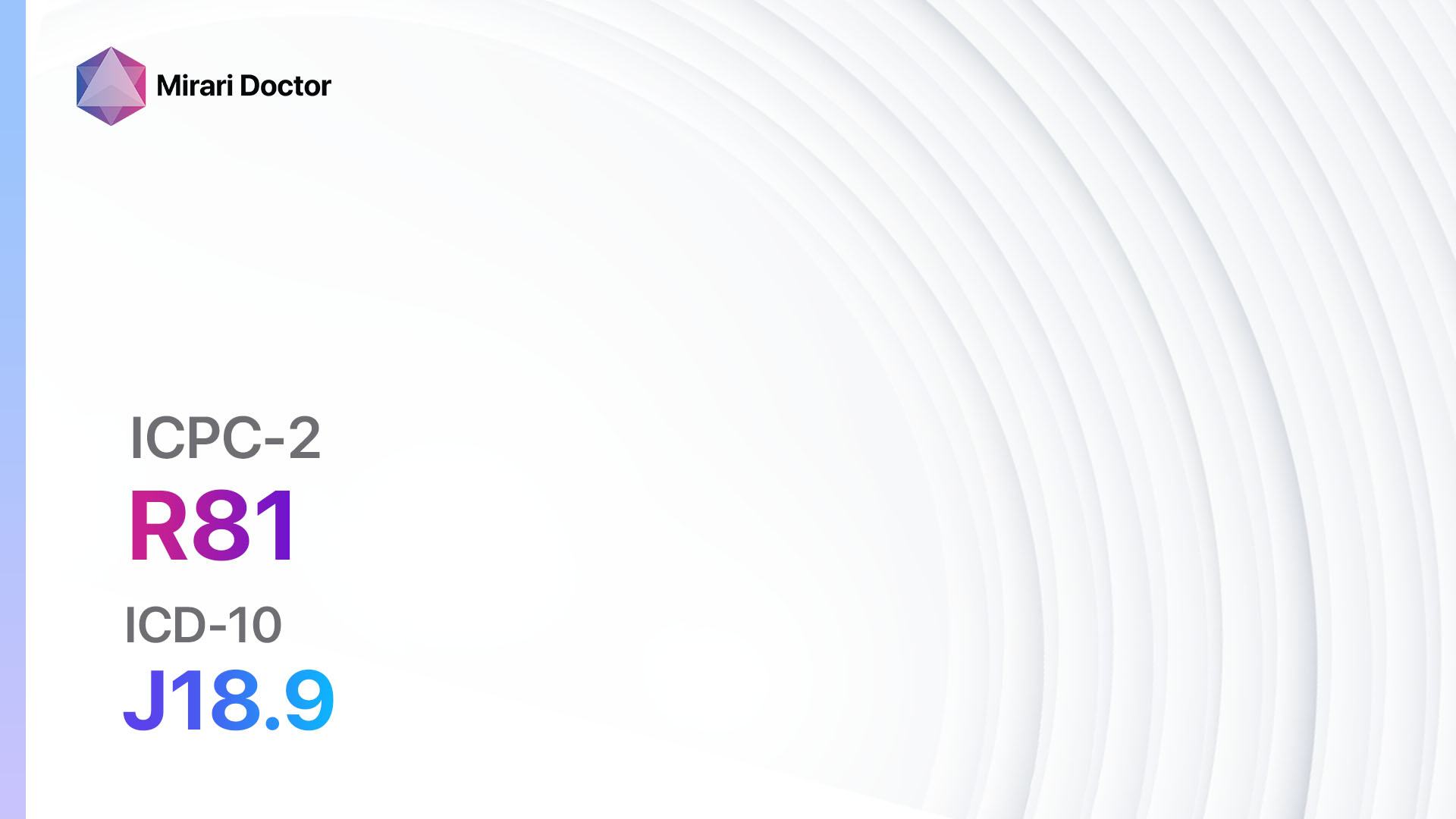
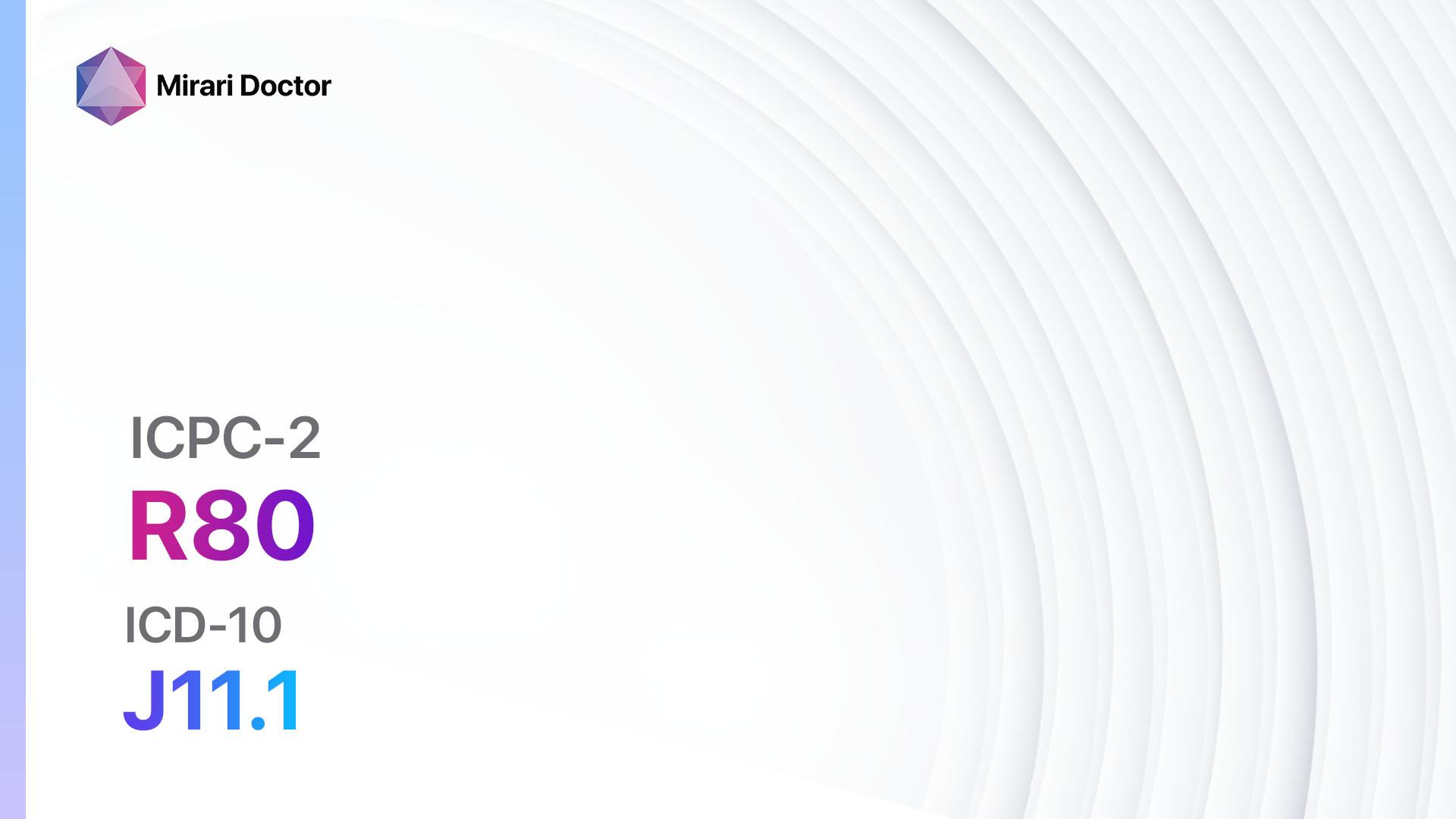
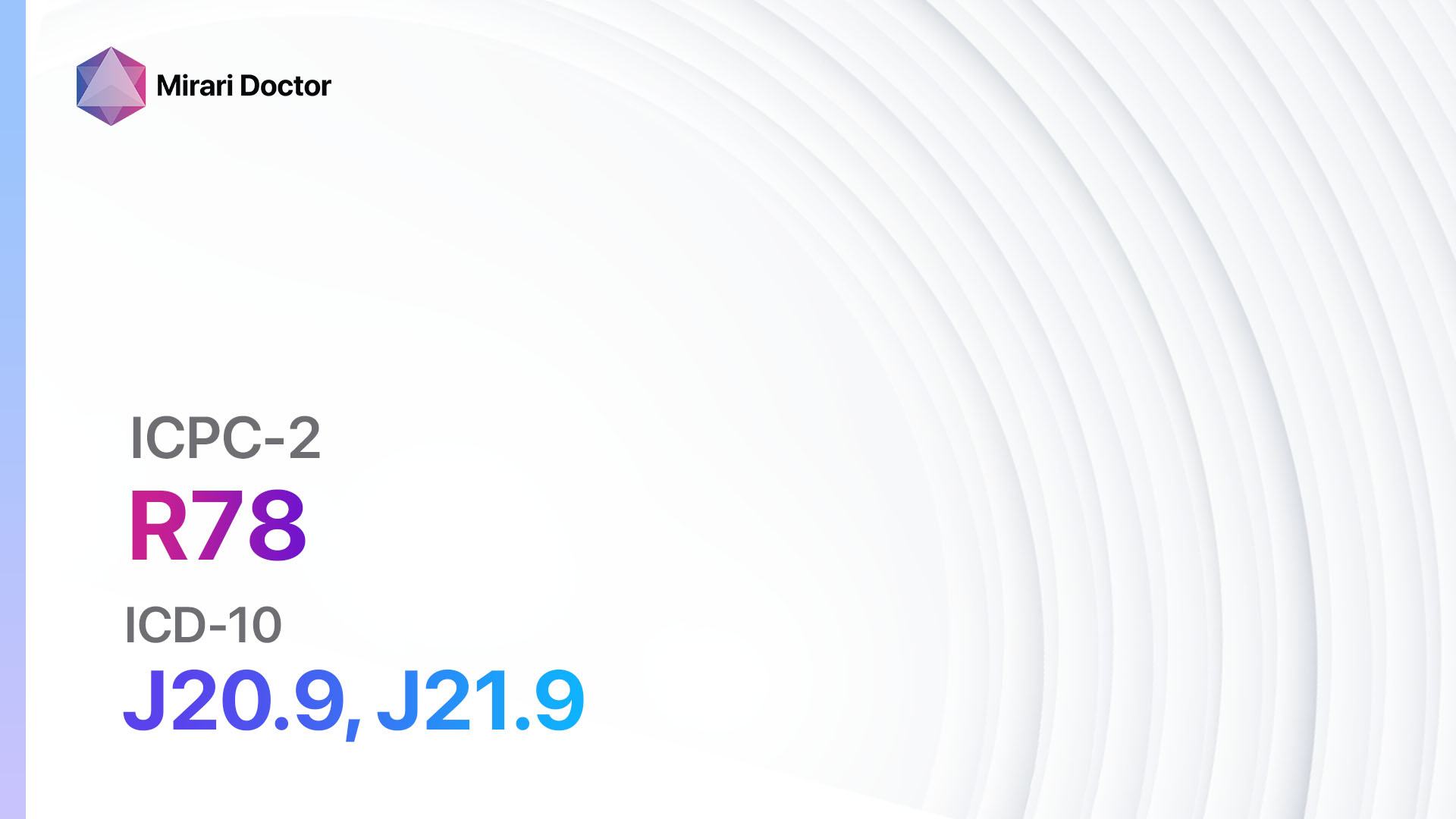
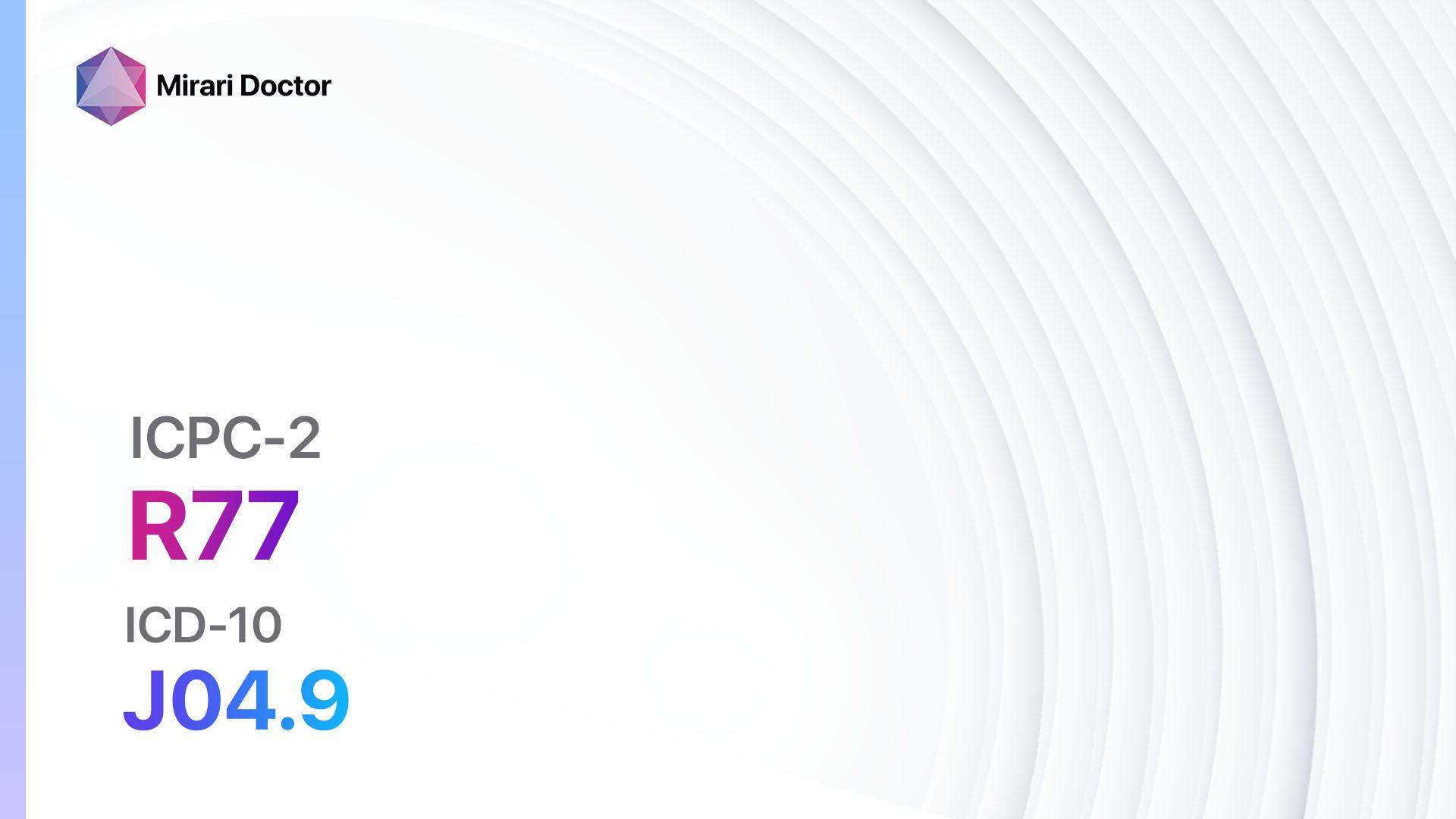
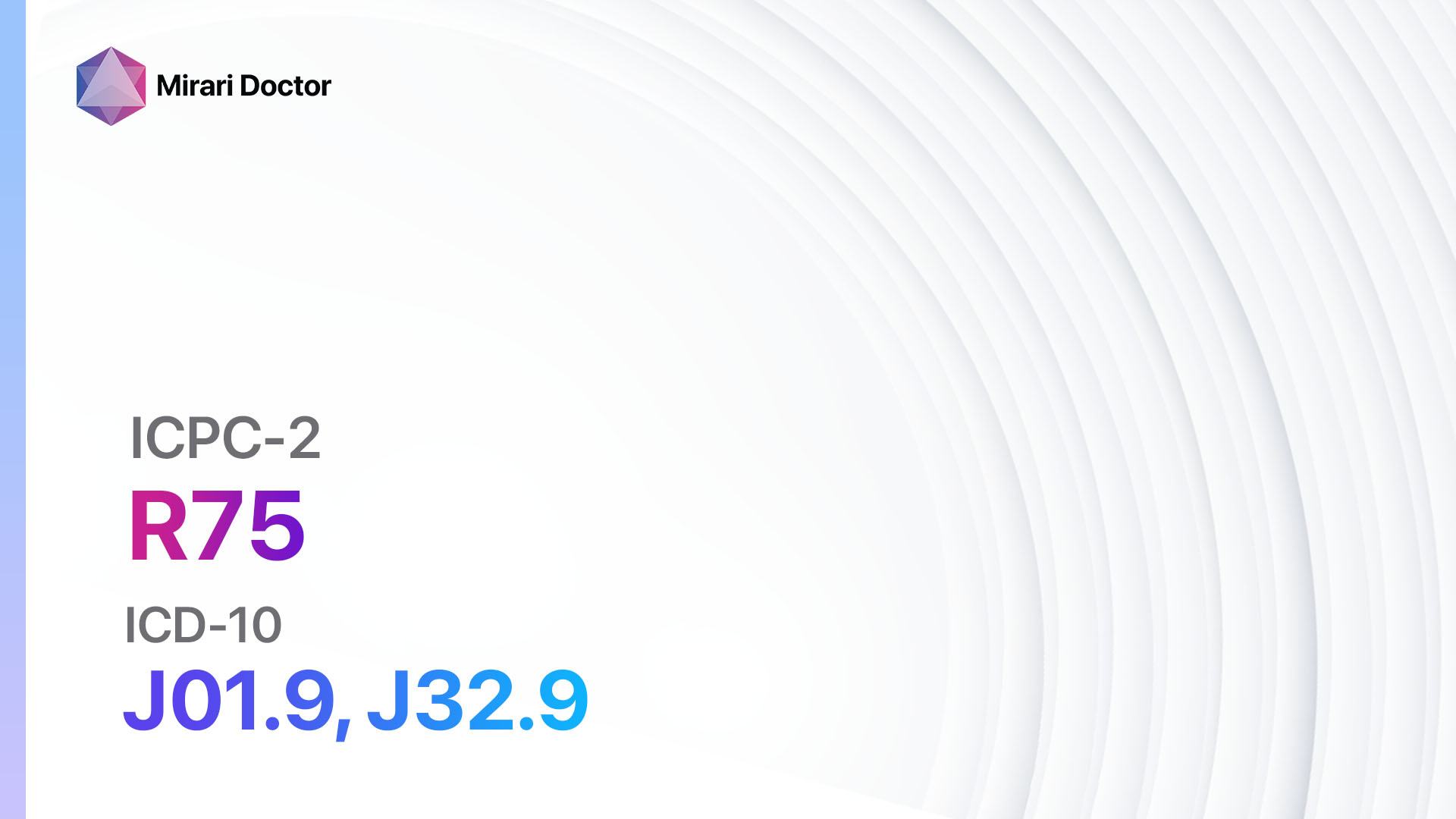
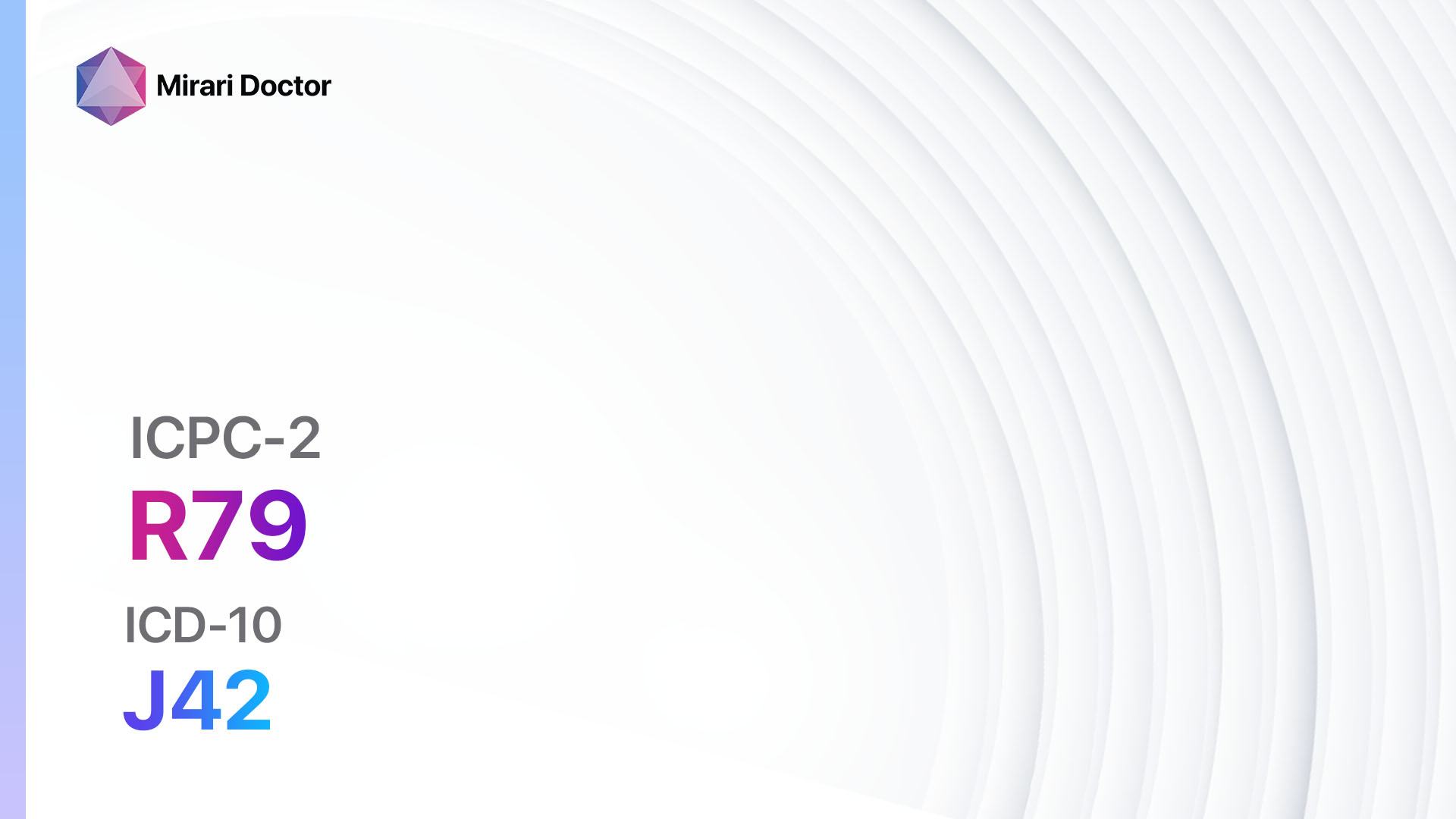
Codes
Symptoms
- Persistent cough: A cough that lasts for at least three months and occurs most days of the month for at least two consecutive years.
- Excessive mucus production: The cough is often accompanied by the production of thick, sticky mucus.
- Shortness of breath: Difficulty breathing, especially during physical activity.
- Wheezing: A whistling or squeaky sound when breathing.
- Chest discomfort: A feeling of tightness or heaviness in the chest.[3]
Causes
- Smoking: The most common cause of chronic bronchitis is long-term cigarette smoking.
- Environmental factors: Exposure to air pollution, dust, or chemical fumes can increase the risk of developing chronic bronchitis.
- Genetics: Certain genetic factors may make some individuals more susceptible to chronic bronchitis.
- Respiratory infections: Repeated respiratory infections, especially during childhood, can contribute to the development of chronic bronchitis.[4]
Diagnostic Steps
Medical History
- Gather information about the patient’s smoking history, including the number of years smoked and the average number of cigarettes smoked per day.
- Ask about exposure to environmental factors such as air pollution, dust, or chemical fumes.
- Inquire about any previous respiratory infections or lung diseases.
- Assess the patient’s symptoms, including the duration and severity of cough, mucus production, shortness of breath, and wheezing.[5]
Physical Examination
- Auscultate the lungs using a stethoscope to listen for abnormal breath sounds, such as wheezing or crackles.
- Assess the patient’s respiratory rate and effort.
- Look for signs of cyanosis (bluish discoloration of the lips or fingertips) indicating low oxygen levels.
- Examine the patient’s chest for any abnormalities or deformities.[6]
Laboratory Tests
- Complete blood count (CBC): To assess for signs of infection or anemia.
- Arterial blood gas (ABG) analysis: To measure oxygen and carbon dioxide levels in the blood.
- Sputum culture: To identify any bacterial or fungal infections.
- Pulmonary function tests (PFTs): To evaluate lung function and determine the severity of airflow obstruction.
- Alpha-1 antitrypsin deficiency test: To rule out a genetic cause of chronic bronchitis.[7]
Diagnostic Imaging
- Chest X-ray: To assess the structure of the lungs and rule out other lung diseases.
- High-resolution computed tomography (HRCT) scan: To provide detailed images of the lungs and assess the extent of damage or inflammation.
- Pulmonary angiography: To evaluate blood flow in the lungs and rule out other conditions such as pulmonary embolism.[8]
Other Tests
- Bronchoscopy: A thin, flexible tube with a camera is inserted into the airways to visualize the bronchial tubes and collect tissue samples for further analysis.
- Lung biopsy: A small sample of lung tissue is taken for examination under a microscope to confirm the diagnosis and rule out other lung diseases.[9]
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the progression of the disease and adjust treatment as needed.
- Provide education on smoking cessation and the importance of avoiding environmental triggers.
- Teach proper techniques for using inhalers and other respiratory devices.
- Encourage the patient to participate in pulmonary rehabilitation programs to improve lung function and quality of life.[10]
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Chronic bronchitis:
- Bronchodilators (e.g., Albuterol, Salmeterol):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Tremors, increased heart rate.
- Severe side effects: Chest pain, irregular heartbeat.
- Drug interactions: Beta-blockers, diuretics.
- Warning: Overuse may lead to decreased effectiveness.
- Inhaled corticosteroids (e.g., Fluticasone, Budesonide):
- Cost: Generic versions can be $30-$100/month.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Thrush (oral yeast infection), hoarseness.
- Severe side effects: Adrenal suppression, osteoporosis.
- Drug interactions: Strong CYP3A4 inhibitors.
- Warning: Rinse mouth after use to prevent thrush.
- Mucolytics (e.g., Acetylcysteine, Carbocisteine):
- Cost: Generic versions can be $10-$30/month.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Nausea, vomiting.
- Severe side effects: Bronchospasm, anaphylaxis.
- Drug interactions: Nitroglycerin, antitussives.
- Warning: Use with caution in patients with asthma.
- Antibiotics (e.g., Azithromycin, Amoxicillin):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Nausea, diarrhea.
- Severe side effects: Severe allergic reactions, Clostridium difficile infection.
- Drug interactions: Warfarin, oral contraceptives.
- Warning: Use only when bacterial infection is present.
- Oxygen therapy:
- Cost: Varies depending on the type of equipment and insurance coverage.
- Contraindications: None.
- Side effects: Dry or bloody nose, skin irritation.
- Severe side effects: Oxygen toxicity.
- Drug interactions: None.
- Warning: Use as prescribed and avoid smoking near oxygen source.
Surgical Procedures:
- Lung volume reduction surgery: Removes damaged lung tissue to improve lung function. Cost: $50,000 to $100,000.
- Lung transplant: Replaces the diseased lungs with healthy donor lungs. Cost: $700,000 to $1,000,000.
Alternative Interventions
- Acupuncture: May help reduce cough and improve lung function. Cost: $60-$120 per session.
- Herbal supplements: Certain herbs, such as licorice root and ivy leaf, may have expectorant properties. Cost: Varies depending on the specific supplement.
- Breathing exercises: Techniques such as pursed-lip breathing and diaphragmatic breathing can help improve lung function. Cost: Free.
- Chest physiotherapy: Manual techniques to help clear mucus from the lungs. Cost: $50-$100 per session.
- Nutritional supplements: Omega-3 fatty acids and antioxidants may have anti-inflammatory effects. Cost: Varies depending on the specific supplement.
Lifestyle Interventions
- Smoking cessation: Quitting smoking is the most important step in managing chronic bronchitis. Cost: Varies depending on the method used (e.g., nicotine replacement therapy, medications, counseling).
- Avoiding environmental triggers: Minimize exposure to air pollution, dust, and chemical fumes. Cost: Varies depending on the individual’s living and working environment.
- Regular exercise: Engaging in physical activity can improve lung function and overall fitness. Cost: Varies depending on the chosen activity (e.g., gym membership, home exercise equipment).
- Healthy diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can support overall health. Cost: Varies depending on individual food choices.
- Pulmonary rehabilitation: Participating in a structured program that includes exercise, education, and support can improve symptoms and quality of life. Cost: Varies depending on the program and insurance coverage.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment:Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies:Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort:Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection:Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R79 Chronic bronchitis (ICD-10:J42)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Modesetting:7 (Immunotherapy) Location:1 (Sacrum) Morning:15minutes, Evening:15minutes | Modesetting:7 (Immunotherapy) Location:1 (Sacrum) Morning:30minutes, Lunch:30minutes, Evening:30minutes | Modesetting:7 (Immunotherapy) Location:1 (Sacrum) Morning:30minutes, Lunch:30minutes, Evening:30minutes |
| Mode setting:7 (Immunotherapy) Location:4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes | Mode setting:7 (Immunotherapy) Location:4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting:7 (Immunotherapy) Location:4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning:60minutesapprox.$10USD, Evening:60minutesapprox.$10USD | Total Morning:120minutesapprox.$20USD, Lunch:120minutesapprox. $20 USD, Evening:120minutesapprox. $20 USD, | Total Morning:120minutesapprox.$20USD, Lunch:120minutesapprox. $20 USD, Evening:120minutesapprox. $20 USD, |
| Usualtreatmentfor7-60daysapprox.$140USD–$1200USD | Usualtreatmentfor6-8weeksapprox.$2,520USD–$3,360USD | Usualtreatmentfor3-6monthsapprox.$5,400USD–$10,800USD |
 |
|
Use the Mirari Cold Plasma device to treat Chronic bronchitis effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Chronic bronchitis. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2021 Report.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). 2019.
- Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347-365.
- Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765-773.
- Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179-191.
- Celli BR, MacNee W; ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932-946.
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report: GOLD Executive Summary. Eur Respir J. 2017;49(3):1700214.
- Lynch DA, Austin JH, Hogg JC, et al. CT-Definable Subtypes of Chronic Obstructive Pulmonary Disease: A Statement of the Fleischner Society. Radiology. 2015;277(1):192-205.
- Washko GR, Diaz AA, Kim V, et al. Computed tomographic measures of airway morphology in smokers and never-smoking normals. J Appl Physiol (1985). 2014;116(6):668-673.
- Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13-e64.
Related articles
Made in USA