Introduction
Respiratory infections are common and can be caused by various pathogens, including viruses, bacteria, and fungi. Respiratory infection other (ICPC-2: R83) refers to respiratory infections that do not fall into specific categories such as upper respiratory tract infections or pneumonia.[1]This guide aims to provide healthcare professionals with a comprehensive approach to diagnosing and managing respiratory infection other.
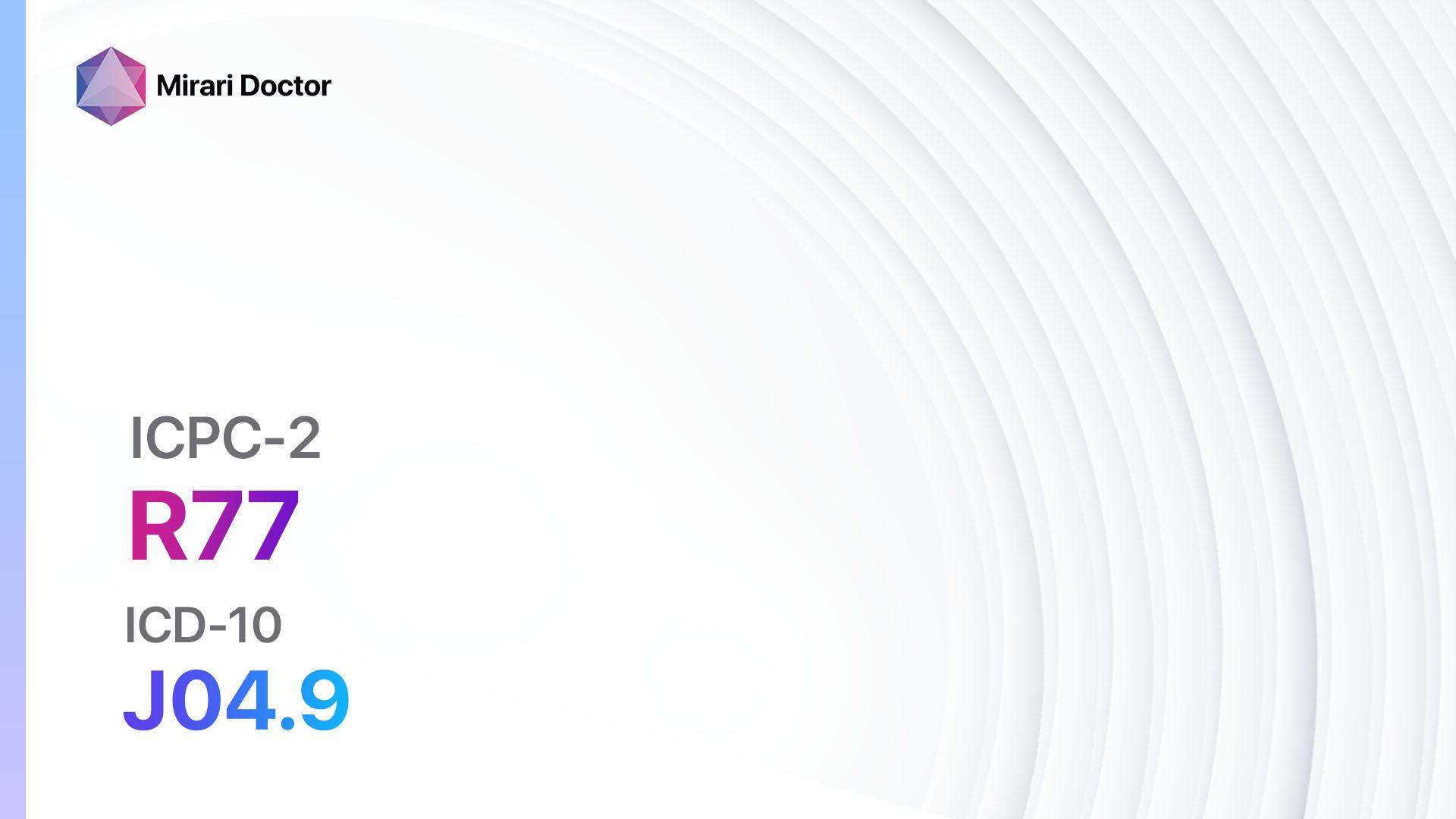
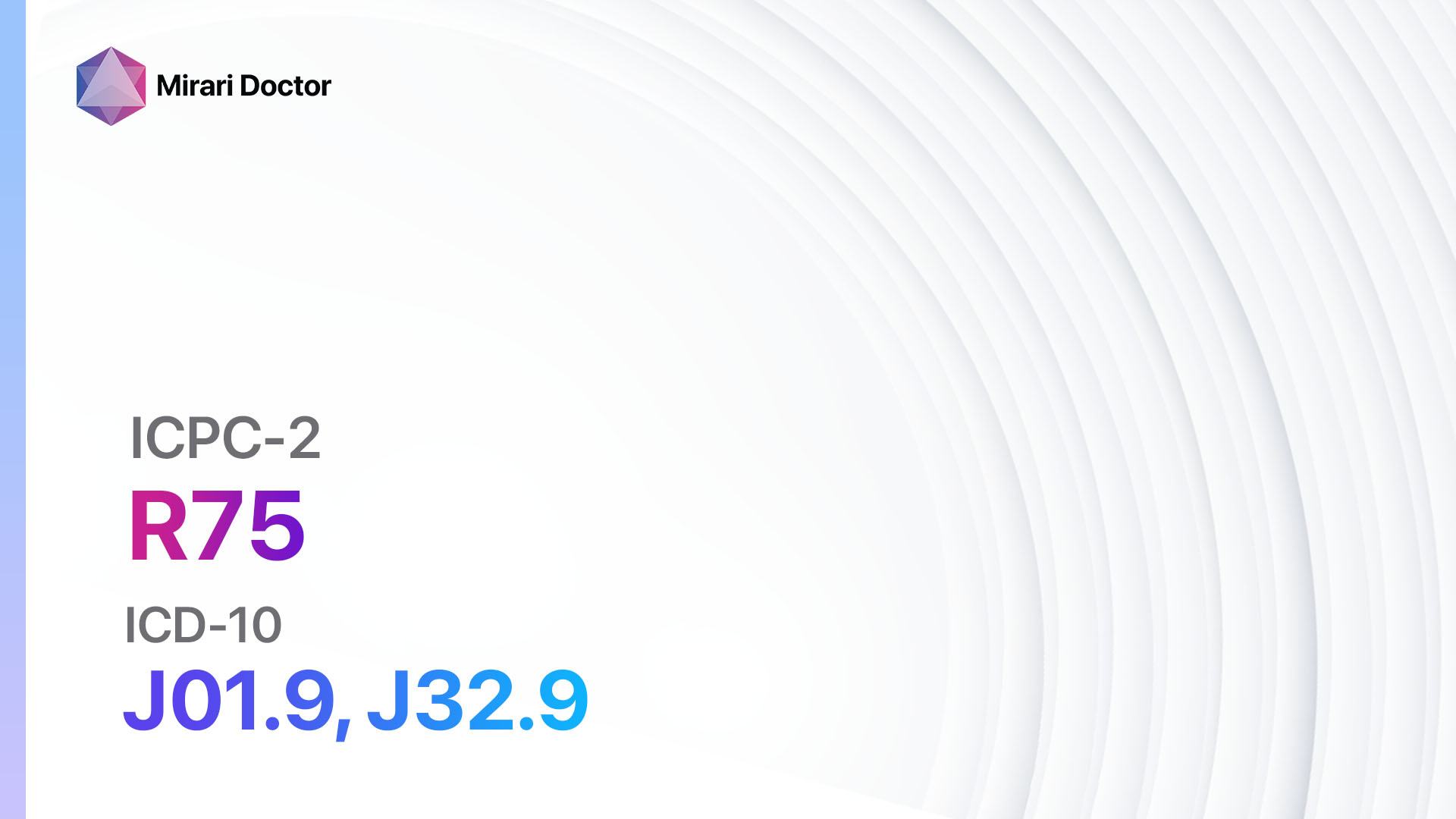
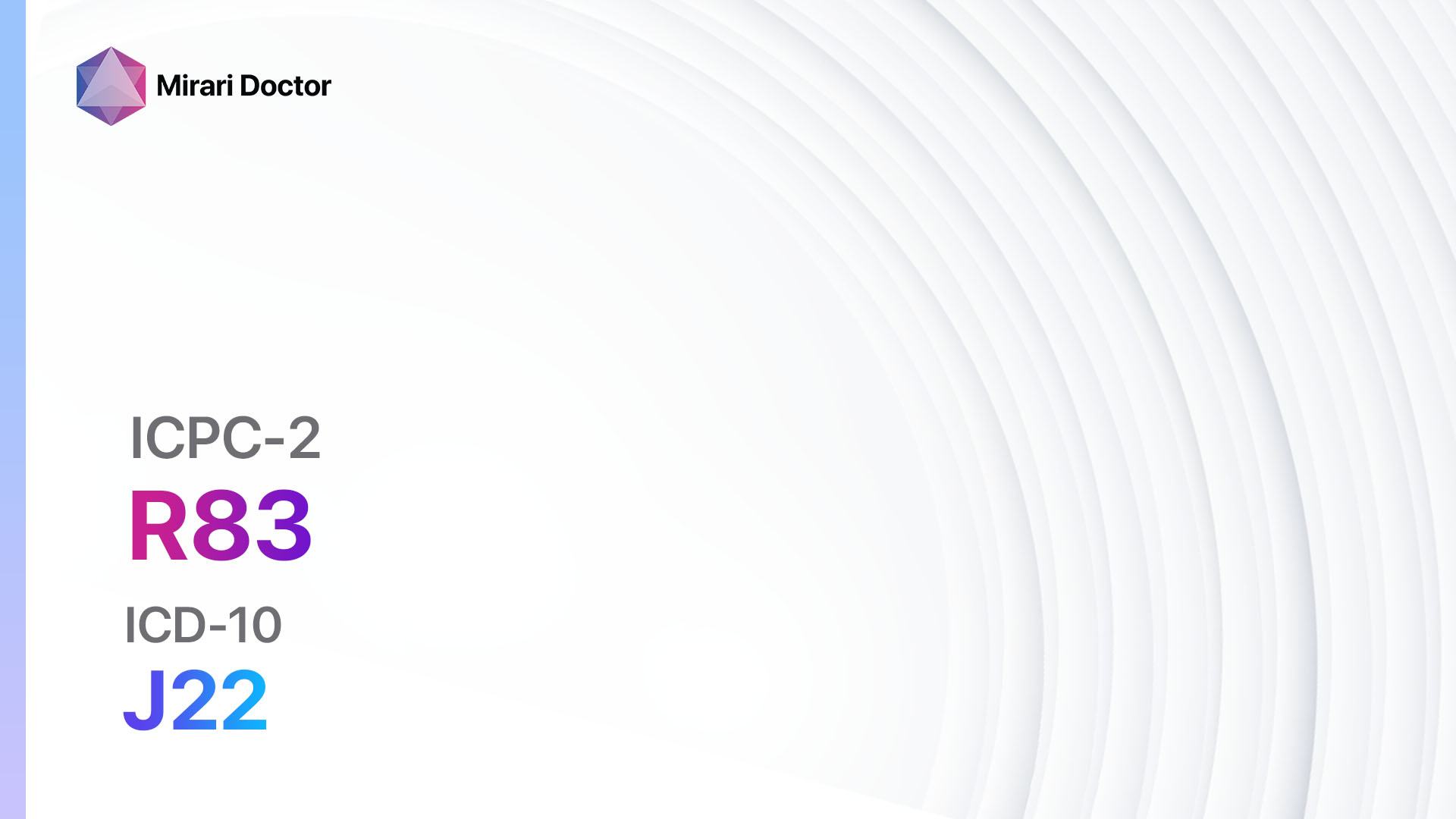
Codes
- ICPC-2 Code: R83 Respiratory infection other
- ICD-10 Code: J22 Unspecified acute lower respiratory infection[2]
Symptoms
- Cough: Persistent cough that may be dry or productive.
- Sore throat: Pain or discomfort in the throat.
- Nasal congestion: Blockage or stuffiness in the nasal passages.
- Sneezing: Frequent and uncontrollable sneezing.
- Fatigue: Feeling tired or exhausted.
- Headache: Aching or pain in the head.
- Fever: Elevated body temperature above 100.4°F (38°C).
- Shortness of breath: Difficulty breathing or breathlessness.[3]
Causes
- Viral infections: Respiratory infections can be caused by various viruses, including rhinovirus, influenza virus, respiratory syncytial virus (RSV), and coronavirus.
- Bacterial infections: Certain bacteria, such as Streptococcus pneumoniae and Haemophilus influenzae, can cause respiratory infections.
- Fungal infections: In rare cases, fungal infections like Aspergillus or Candida can lead to respiratory infections.
- Environmental factors: Exposure to pollutants, allergens, or irritants can contribute to respiratory infections.[4]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration and severity.
- Ask about any recent travel or exposure to individuals with respiratory infections.
- Inquire about any underlying medical conditions, such as asthma or chronic obstructive pulmonary disease (COPD).
- Assess the patient’s immunization status, particularly for influenza and pneumococcal vaccines.[5]
Physical Examination
- Evaluate vital signs, including temperature, heart rate, and respiratory rate.
- Examine the patient’s throat, lungs, and nasal passages for signs of inflammation or infection.
- Listen to lung sounds using a stethoscope to detect any abnormal breath sounds.
- Check for enlarged lymph nodes in the neck or other areas.[6]
Laboratory Tests
- Complete blood count (CBC): Assess for elevated white blood cell count, which may indicate an infection.
- Nasal swab or throat culture: Collect samples to test for specific pathogens, such as influenza or Streptococcus.
- Chest X-ray: Evaluate the lungs for signs of pneumonia or other abnormalities.
- Pulse oximetry: Measure oxygen saturation levels to assess respiratory function.[7]
Diagnostic Imaging
- Chest X-ray: Provides a detailed image of the lungs to identify any abnormalities, such as pneumonia or lung masses.
- Computed tomography (CT) scan: Offers a more detailed view of the lungs and surrounding structures, useful for detecting lung abscesses or evaluating the extent of infection.[8]
Other Tests
- Sputum culture: Collect a sample of sputum to identify the specific bacteria causing the infection.
- Allergy testing: Determine if the respiratory infection is triggered by allergies.
- Pulmonary function tests: Assess lung function and identify any underlying respiratory conditions, such as asthma or COPD.[9]
Follow-up and Patient Education
- Schedule a follow-up appointment to monitor the patient’s progress and ensure appropriate treatment.
- Educate the patient about the importance of rest, hydration, and good respiratory hygiene (covering mouth and nose when coughing or sneezing).
- Advise the patient to seek medical attention if symptoms worsen or persist for an extended period.[10]
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Respiratory infection other:
- Antibiotics (e.g., Amoxicillin, Azithromycin):
- Cost: Generic versions can range from $3 to $50.
- Contraindications: Allergy to antibiotics, severe liver disease.
- Side effects: Nausea, diarrhea, rash.
- Severe side effects: Severe allergic reactions, Clostridium difficile infection.
- Drug interactions: Warfarin, oral contraceptives.
- Warning: Complete the full course of antibiotics as prescribed.
- Antiviral medications (e.g., Oseltamivir, Zanamivir):
- Cost: Generic versions can range from $50 to $150.
- Contraindications: Severe renal impairment, allergy to antiviral medications.
- Side effects: Nausea, vomiting, headache.
- Severe side effects: Neuropsychiatric events, severe allergic reactions.
- Drug interactions: None significant.
- Warning: Start antiviral treatment within 48 hours of symptom onset for optimal efficacy.
- Bronchodilators (e.g., Albuterol, Ipratropium):
- Cost: Generic versions can range from $10 to $50.
- Contraindications: Allergy to bronchodilators, severe cardiac disease.
- Side effects: Tremor, tachycardia, dry mouth.
- Severe side effects: Cardiac arrhythmias, paradoxical bronchospasm.
- Drug interactions: Beta-blockers, diuretics.
- Warning: Use with caution in patients with a history of seizures or hyperthyroidism.
- Corticosteroids (e.g., Prednisone, Dexamethasone):
- Cost: Generic versions can range from $5 to $30.
- Contraindications: Active infections, systemic fungal infections.
- Side effects: Increased appetite, weight gain, mood changes.
- Severe side effects: Adrenal suppression, osteoporosis.
- Drug interactions: Nonsteroidal anti-inflammatory drugs (NSAIDs), anticoagulants.
- Warning: Use the lowest effective dose for the shortest duration possible.
- Antipyretics (e.g., Acetaminophen, Ibuprofen):
- Cost: Generic versions can range from $3 to $10.
- Contraindications: Severe liver disease, allergy to antipyretics.
- Side effects: Nausea, stomach pain, rash.
- Severe side effects: Severe allergic reactions, liver toxicity.
- Drug interactions: Warfarin, alcohol.
- Warning: Follow the recommended dosage and avoid exceeding the maximum daily dose.
Alternative Drugs:
- Antifungal medications (e.g., Fluconazole): Used for respiratory infections caused by fungi.
- Antihistamines (e.g., Loratadine, Cetirizine): May help relieve symptoms such as nasal congestion and sneezing.
- Mucolytics (e.g., Guaifenesin): Aid in thinning and loosening mucus, making it easier to cough up.
- Nasal decongestants (e.g., Oxymetazoline): Provide temporary relief from nasal congestion.
Surgical Procedures:
- Invasive procedures are generally not required for respiratory infection other. However, in rare cases, surgical intervention may be necessary to drain abscesses or remove obstructions.
Alternative Interventions
- Steam inhalation: Breathing in warm, moist air can help soothe the respiratory tract and alleviate congestion. Cost: Free.
- Herbal remedies: Certain herbs, such as Echinacea and elderberry, are believed to have immune-boosting properties. Cost: Varies depending on the specific herb and preparation.
- Nasal irrigation: Flushing the nasal passages with a saline solution can help clear mucus and reduce nasal congestion. Cost: $10-$20 for a nasal irrigation kit.
- Probiotics: Some studies suggest that probiotics may help strengthen the immune system and reduce the severity of respiratory infections. Cost: Varies depending on the specific probiotic supplement.
Lifestyle Interventions
- Rest and hydration: Getting plenty of rest and staying hydrated can support the body’s immune response and aid in recovery. Cost: Free.
- Good respiratory hygiene: Encourage the patient to cover their mouth and nose when coughing or sneezing to prevent the spread of infection. Cost: Free.
- Avoiding triggers: If the respiratory infection is triggered by allergens or irritants, the patient should try to minimize exposure to these substances. Cost: Varies depending on the specific triggers.
- Quitting smoking: Smoking can worsen respiratory infections and delay healing. Encourage patients to quit smoking to improve their respiratory health. Cost: Varies depending on the method used for smoking cessation.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment:Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies:Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort:Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection:Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R83 Respiratory infection other (ICD-10:J22)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting:7 (Immunotherapy) Location:4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes | Mode setting:7 (Immunotherapy) Location:4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting:7 (Immunotherapy) Location:4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning:60minutesapprox.$10USD, Evening:60minutesapprox.$10USD | Total Morning:120minutesapprox.$20USD, Lunch:120minutesapprox. $20 USD, Evening:120minutesapprox. $20 USD, | Total Morning:120minutesapprox.$20USD, Lunch:120minutesapprox. $20 USD, Evening:120minutesapprox. $20 USD, |
| Usualtreatmentfor7-60daysapprox.$140USD–$1200USD | Usualtreatmentfor6-8weeksapprox.$2,520USD–$3,360USD | Usualtreatmentfor3-6monthsapprox.$5,400USD–$10,800USD |
 |
|
Use the Mirari Cold Plasma device to treat Respiratory infection other effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Respiratory infection other. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- World Organization of Family Doctors (WONCA). International Classification of Primary Care, 2nd edition (ICPC-2). Oxford University Press; 1998.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Geneva: WHO; 2019.
- Eccles R. Understanding the symptoms of the common cold and influenza. Lancet Infect Dis. 2005;5(11):718-725.
- Dasaraju PV, Liu C. Infections of the Respiratory System. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996.
- Schaffner W, Rehm SJ, Elasy TA. Influenza vaccination: an unmet need in patients with diabetes. Clin Diabetes. 2007;25(4):145-149.
- Bickley LS, Szilagyi PG. Bates’ Guide to Physical Examination and History Taking. 12th edition. Philadelphia: Wolters Kluwer; 2017.
- Metlay JP, Waterer GW, Long AC, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-e67.
- Franquet T. Imaging of pulmonary viral pneumonia. Radiology. 2011;260(1):18-39.
- Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948-968.
- Fashner J, Ericson K, Werner S. Treatment of the common cold in children and adults. Am Fam Physician. 2012;86(2):153-159.
Related articles
Made in USA