Introduction
Pneumonia is a respiratory infection that affects the lungs, causing inflammation and fluid buildup. It can be caused by various pathogens, including bacteria, viruses, and fungi. Pneumonia can range from mild to severe and can be life-threatening, especially in vulnerable populations such as the elderly and those with weakened immune systems.[1] The aim of this guide is to provide a comprehensive overview of the symptoms, causes, diagnostic steps, possible interventions, and patient education for pneumonia.
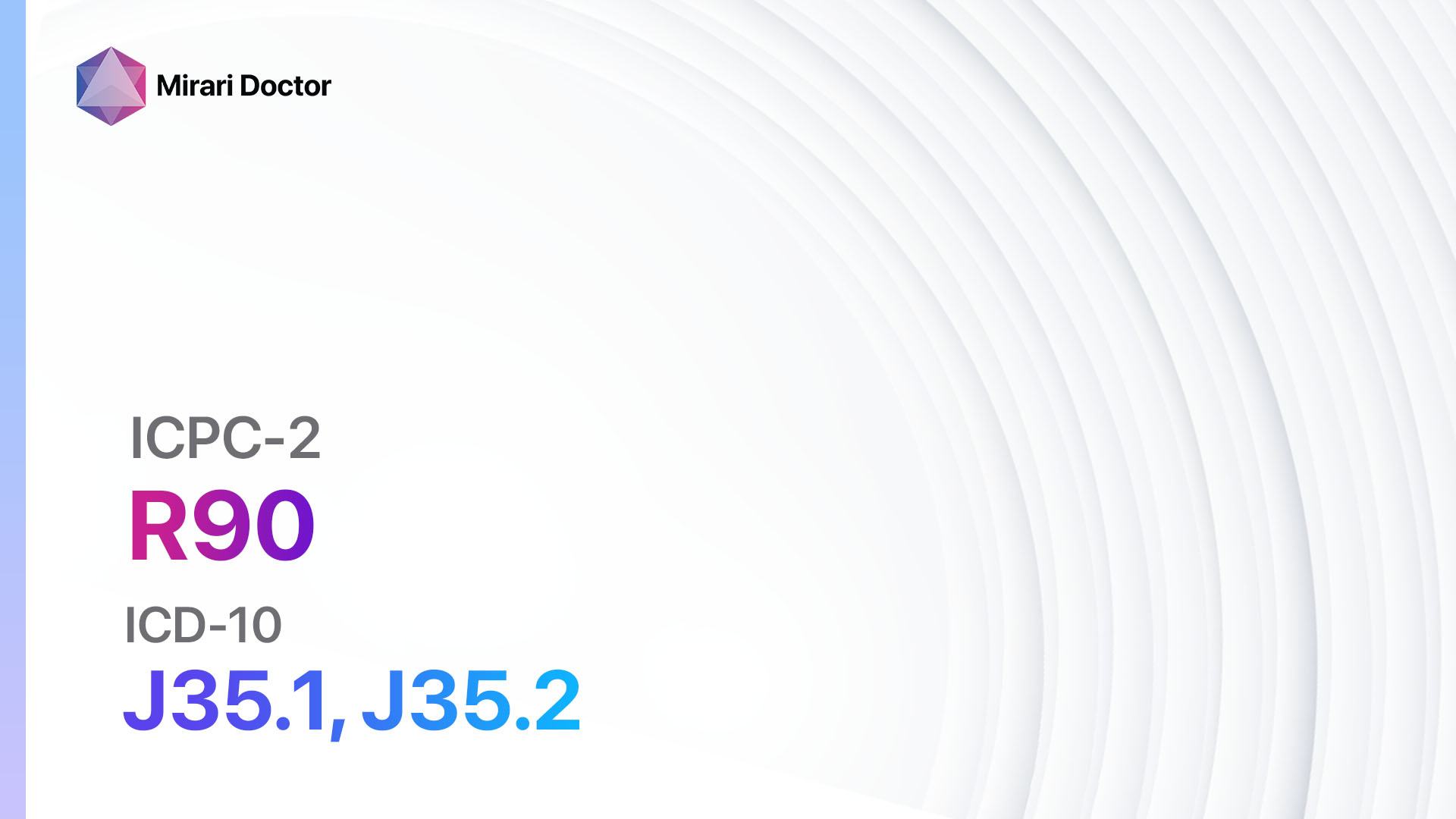
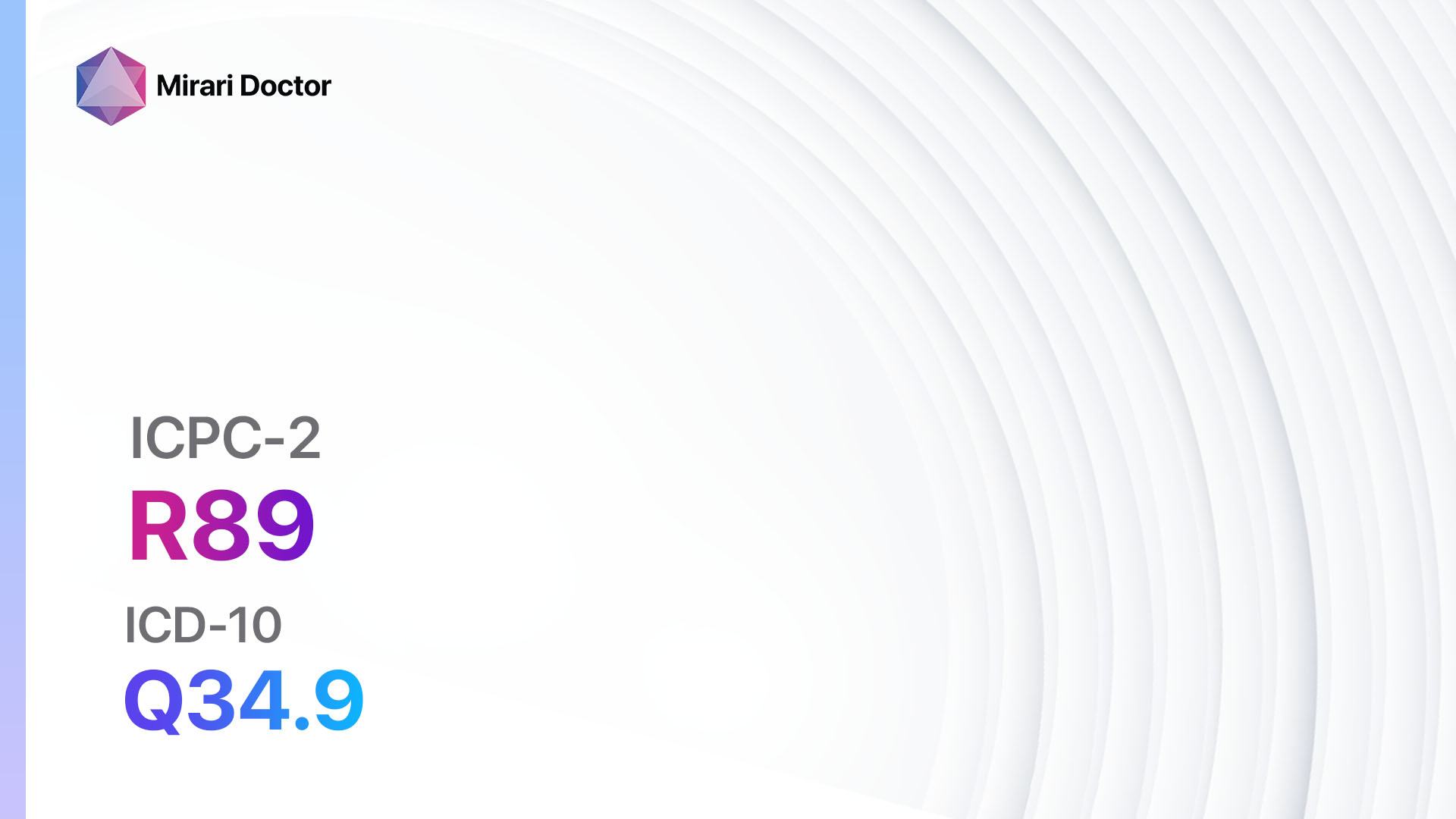
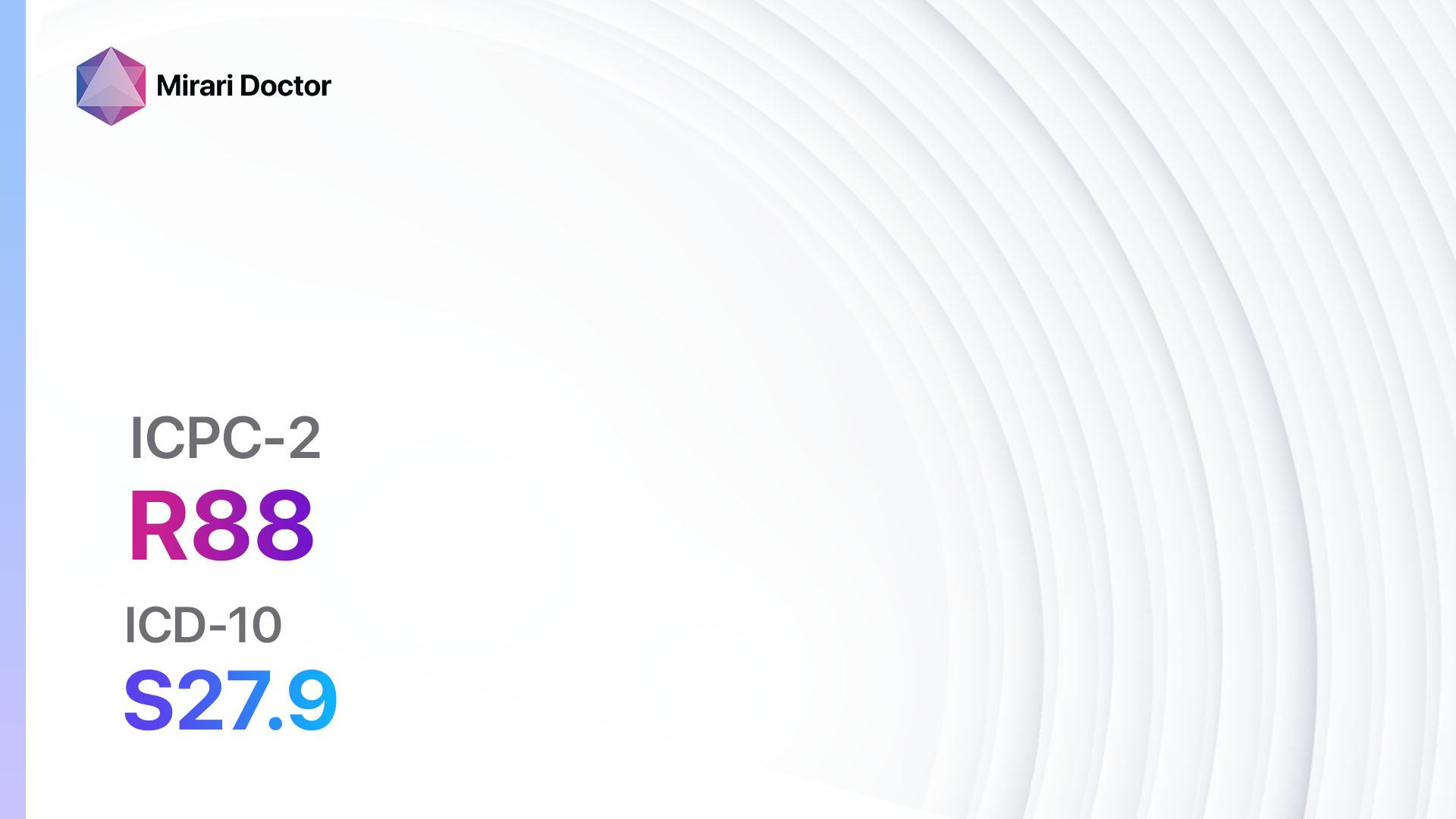
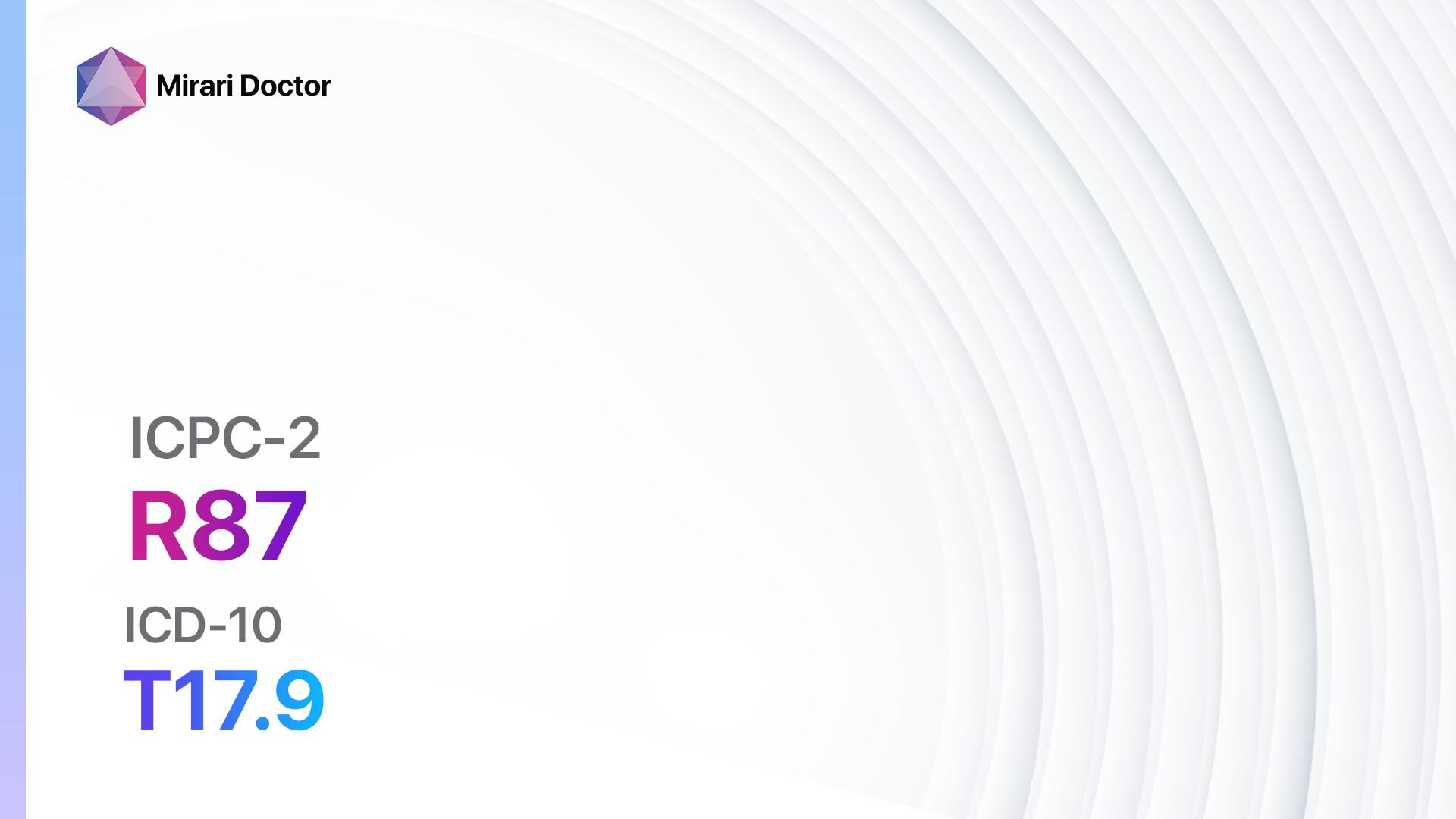
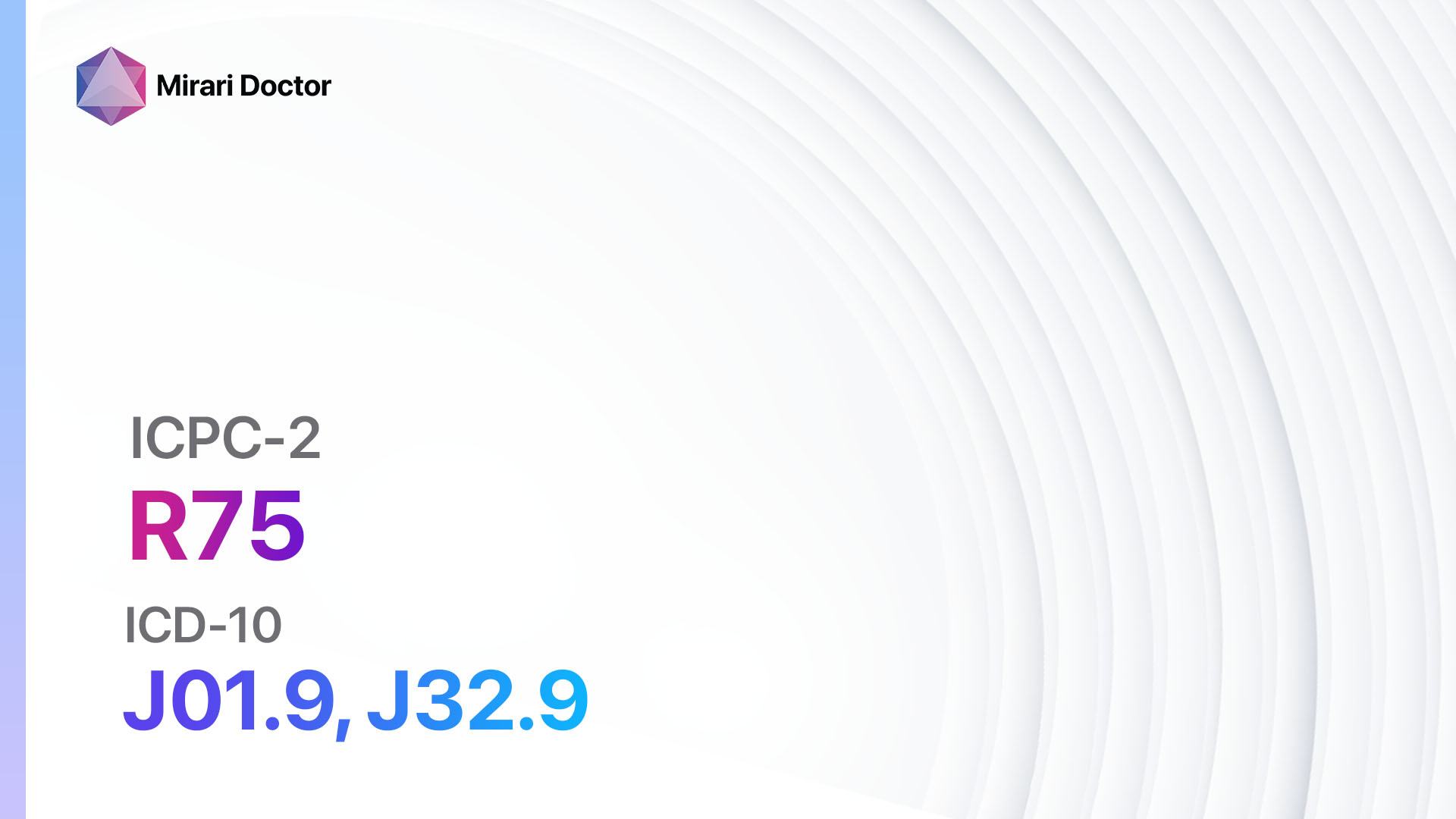
Codes
Symptoms
- Cough: A persistent cough that may produce phlegm or mucus.
- Fever: Elevated body temperature, often accompanied by chills.
- Shortness of breath: Difficulty breathing or rapid breathing.
- Chest pain: Sharp or stabbing pain in the chest, worsened by deep breaths or coughing.
- Fatigue: Feeling tired or weak.
- Sweating: Excessive sweating, especially during sleep.
- Confusion: Mental confusion or disorientation, particularly in older adults.
- Bluish lips or nails: A sign of low oxygen levels in the blood.[3]
Causes
- Bacterial infection: The most common cause of pneumonia, with Streptococcus pneumoniae being the most prevalent bacteria.
- Viral infection: Viruses such as influenza, respiratory syncytial virus (RSV), and rhinovirus can cause viral pneumonia.
- Fungal infection: Fungi such as Pneumocystis jirovecii can cause pneumonia, especially in individuals with weakened immune systems.
- Aspiration: Inhaling food, drink, or saliva into the lungs can lead to aspiration pneumonia.
- Hospital-acquired pneumonia: Pneumonia acquired during a hospital stay, often caused by drug-resistant bacteria.[4]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration and severity.
- Identify any risk factors, such as recent travel, exposure to sick individuals, or underlying medical conditions.
- Determine if the patient has received any recent vaccinations, such as the pneumococcal vaccine.[5]
Physical Examination
- Listen to the patient’s lungs using a stethoscope to detect abnormal breath sounds, such as crackles or wheezing.
- Check for signs of respiratory distress, such as increased respiratory rate or use of accessory muscles.
- Assess the patient’s vital signs, including temperature, heart rate, and oxygen saturation.[6]
Laboratory Tests
- Complete blood count (CBC): To check for elevated white blood cell count, which may indicate an infection.
- Blood cultures: To identify the specific pathogen causing the pneumonia.
- Sputum culture: To determine the presence of bacteria or fungi in the respiratory secretions.
- Pulse oximetry: To measure the oxygen saturation levels in the blood.
- Arterial blood gas (ABG) analysis: To assess the patient’s respiratory function and acid-base balance.[7]
Diagnostic Imaging
- Chest X-ray: To visualize the lungs and identify areas of consolidation or fluid buildup.
- Computed tomography (CT) scan: To obtain detailed images of the lungs, especially in cases of complicated pneumonia or suspected lung abscess.
- Lung ultrasound: To assess lung function and detect pleural effusion or other abnormalities.[8]
Other Tests
- Bronchoscopy: A procedure in which a flexible tube with a camera is inserted into the airways to collect samples or remove obstructions.
- Pleural fluid analysis: To examine the fluid collected from the pleural space for infection or other abnormalities.
- Lung biopsy: In rare cases, a small sample of lung tissue may be obtained for further analysis.[9]
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the patient’s progress and ensure appropriate treatment.
- Educate the patient about the importance of completing the full course of antibiotics or antiviral medications.
- Provide information on preventive measures, such as hand hygiene, vaccination, and avoiding exposure to sick individuals.
- Advise the patient to seek medical attention if symptoms worsen or new symptoms develop.[10]
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Pneumonia:
- Antibiotics (e.g., Amoxicillin, Azithromycin, Levofloxacin):
- Cost: Generic versions can range from $5 to $50 for a course of treatment.
- Contraindications: Allergy to the specific antibiotic, history of severe adverse reactions.
- Side effects: Nausea, diarrhea, rash.
- Severe side effects: Allergic reactions, severe gastrointestinal symptoms.
- Drug interactions: Warfarin, certain antacids.
- Warning: Complete the full course of antibiotics as prescribed.
- Antiviral medications (e.g., Oseltamivir, Zanamivir):
- Cost: Generic versions can range from $50 to $100 for a course of treatment.
- Contraindications: Allergy to the specific antiviral medication.
- Side effects: Nausea, vomiting, headache.
- Severe side effects: Neuropsychiatric events (rare).
- Drug interactions: None significant.
- Warning: Start antiviral treatment within 48 hours of symptom onset for maximum effectiveness.
- Antifungal medications (e.g., Fluconazole, Voriconazole):
- Cost: Generic versions can range from $10 to $100 for a course of treatment.
- Contraindications: Allergy to the specific antifungal medication.
- Side effects: Nausea, abdominal pain, rash.
- Severe side effects: Liver toxicity, severe skin reactions.
- Drug interactions: Certain anticoagulants, statins.
- Warning: Monitor liver function during treatment.
- Bronchodilators (e.g., Albuterol, Ipratropium):
- Cost: Generic versions can range from $10 to $50 for an inhaler.
- Contraindications: Allergy to the specific bronchodilator.
- Side effects: Tremor, increased heart rate.
- Severe side effects: Chest pain, arrhythmias (rare).
- Drug interactions: Beta-blockers, certain antidepressants.
- Warning: Use as directed for symptom relief.
- Corticosteroids (e.g., Prednisone, Methylprednisolone):
- Cost: Generic versions can range from $5 to $20 for a course of treatment.
- Contraindications: Allergy to the specific corticosteroid, active infection.
- Side effects: Increased appetite, weight gain, mood changes.
- Severe side effects: Increased risk of infection, adrenal suppression.
- Drug interactions: Certain anticoagulants, antidiabetic medications.
- Warning: Use corticosteroids cautiously and under medical supervision.
Alternative Drugs:
- Immunomodulators (e.g., Interferon gamma): Used in severe or complicated cases of pneumonia to boost the immune response.
- Mucolytics (e.g., Acetylcysteine): May help thin and loosen mucus, making it easier to cough up.
- Probiotics: Some evidence suggests that certain strains of probiotics may help prevent respiratory infections.
Surgical Procedures:
- In rare cases, surgical intervention may be necessary for complications such as lung abscess or empyema. The specific procedure will depend on the individual case and should be discussed with a surgeon.
Alternative Interventions
- Acupuncture: May help alleviate symptoms and improve overall well-being. Cost: $60-$120 per session.
- Herbal remedies: Certain herbs, such as echinacea and elderberry, may have immune-boosting properties. Cost: Varies depending on the specific herb and preparation.
- Steam inhalation: Inhaling steam from hot water or herbal infusions may help relieve congestion and soothe the respiratory tract. Cost: Minimal.
- Proper hydration: Drinking plenty of fluids, especially warm liquids, can help thin mucus and promote coughing. Cost: Minimal.
- Rest and self-care: Getting adequate rest, maintaining good hygiene, and avoiding exposure to irritants can support the body’s natural healing process. Cost: Minimal.
Lifestyle Interventions
- Smoking cessation: Quitting smoking can improve lung health and reduce the risk of respiratory infections. Cost: Varies depending on the chosen method (e.g., nicotine replacement therapy, counseling).
- Healthy diet: Consuming a balanced diet rich in fruits, vegetables, and whole grains can support immune function. Cost: Varies depending on food choices.
- Regular exercise: Engaging in moderate physical activity can strengthen the immune system and improve overall health. Cost: Varies depending on the chosen activity (e.g., gym membership, home workout equipment).
- Adequate sleep: Getting enough sleep is essential for immune function and overall well-being. Cost: Minimal.
- Stress management: Practicing stress-reducing techniques, such as meditation or yoga, can support immune function. Cost: Varies depending on the chosen method (e.g., classes, online resources).
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R81 Pneumonia (ICD-10:J18.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Pneumonia effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Pneumonia. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Centers for Disease Control and Prevention. (2022). Pneumonia. Retrieved from https://www.cdc.gov/pneumonia/index.html
- World Health Organization. (2019). International Statistical Classification of Diseases and Related Health Problems (ICD-10).
- Mayo Clinic. (2021). Pneumonia – Symptoms and causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/syc-20354204
- American Lung Association. (2022). Learn About Pneumonia. Retrieved from https://www.lung.org/lung-health-diseases/lung-disease-lookup/pneumonia
- Metlay, J. P., Waterer, G. W., Long, A. C., Anzueto, A., Brozek, J., Crothers, K., … & Whitney, C. G. (2019). Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. American Journal of Respiratory and Critical Care Medicine, 200(7), e45-e67.
- Mandell, L. A., Wunderink, R. G., Anzueto, A., Bartlett, J. G., Campbell, G. D., Dean, N. C., … & Whitney, C. G. (2007). Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clinical Infectious Diseases, 44(Supplement_2), S27-S72.
- Lim, W. S., Baudouin, S. V., George, R. C., Hill, A. T., Jamieson, C., Le Jeune, I., … & Woodhead, M. A. (2009). BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax, 64(Suppl 3), iii1-iii55.
- Reissig, A., Copetti, R., Mathis, G., Mempel, C., Schuler, A., Zechner, P., … & Hoyer, H. (2012). Lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia: a prospective, multicenter, diagnostic accuracy study. Chest, 142(4), 965-972.
- Musher, D. M., & Thorner, A. R. (2014). Community-acquired pneumonia. New England Journal of Medicine, 371(17), 1619-1628.
- File, T. M. (2003). Community-acquired pneumonia. The Lancet, 362(9400), 1991-2001.
Related articles
Made in USA