Introduction
Breathing problems can be caused by various factors and can significantly impact a person’s quality of life. This guide aims to provide an overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle changes that can help manage breathing problems.
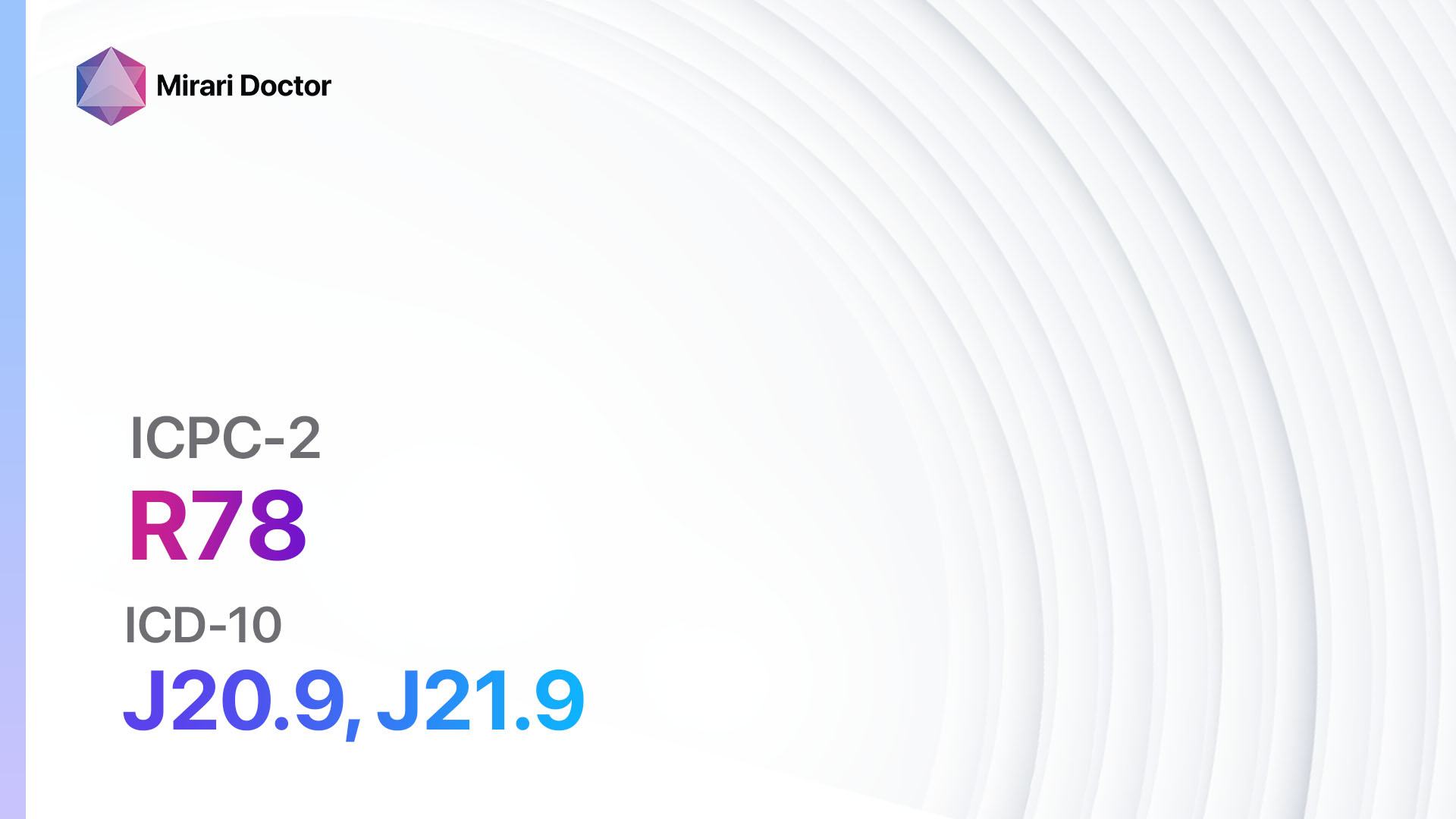
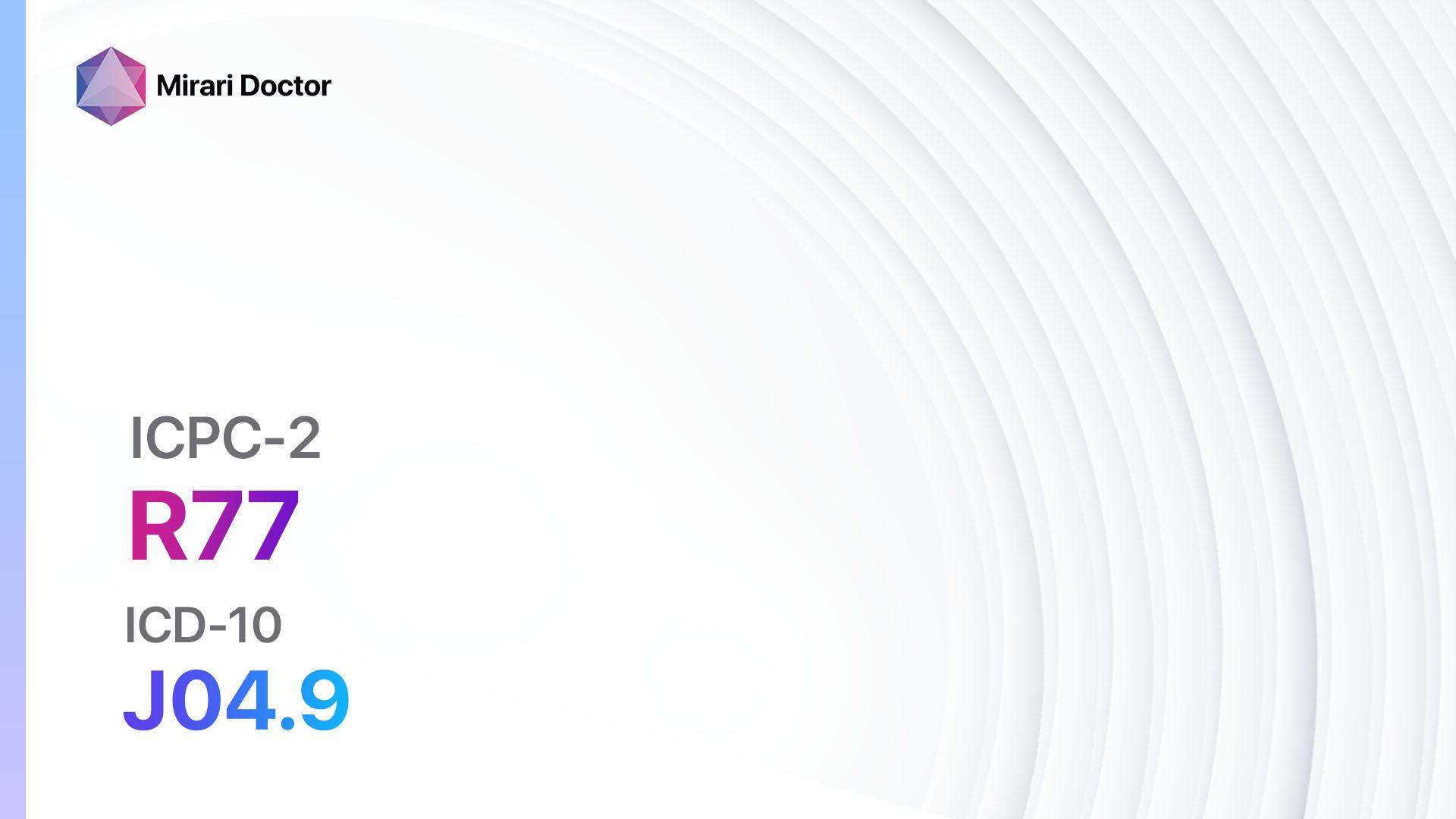
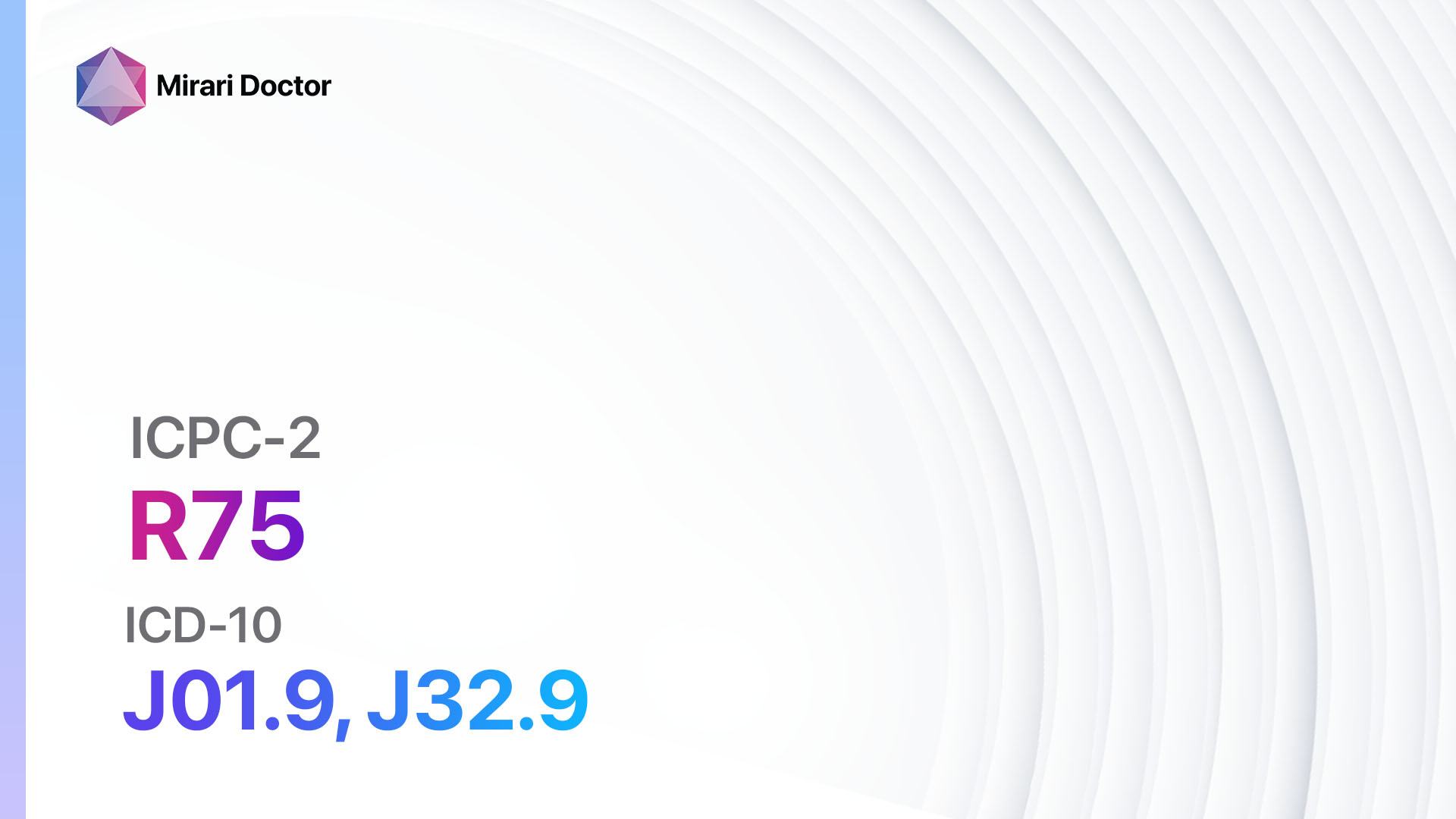
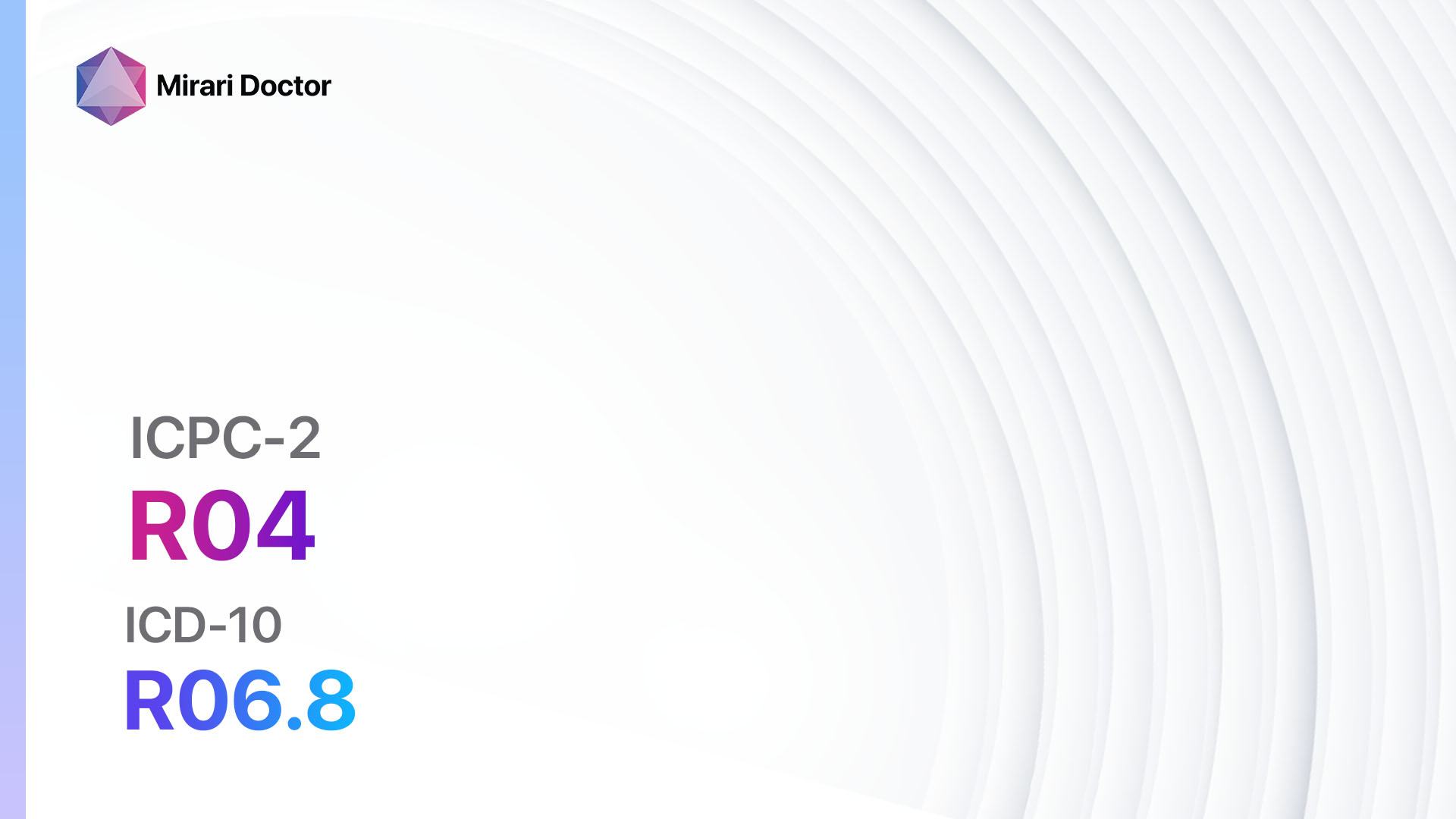
Codes
- ICPC-2 Code: R04 Breathing problem, other
- ICD-10 Code: R06.8 Other and unspecified abnormalities of breathing
Symptoms
- Shortness of breath: Difficulty breathing or a feeling of not getting enough air.[1]
- Wheezing: A high-pitched whistling sound when breathing out.[2]
- Chest tightness: A sensation of pressure or constriction in the chest.[3]
- Coughing: Persistent coughing, especially during physical activity or at night.[4]
- Rapid breathing: Breathing at a faster rate than normal.[5]
- Fatigue: Feeling tired or exhausted due to the increased effort required to breathe.[6]
Causes
- Asthma: A chronic condition characterized by inflammation and narrowing of the airways.[7]
- Chronic obstructive pulmonary disease (COPD): A group of lung diseases, including chronic bronchitis and emphysema, that cause airflow obstruction.[8]
- Allergies: An immune response to certain substances, such as pollen, dust mites, or pet dander.[9]
- Respiratory infections: Infections of the respiratory tract, such as the common cold or pneumonia.[10]
- Obesity: Excess weight can put pressure on the lungs and make breathing more difficult.
- Smoking: Tobacco smoke can irritate the airways and lead to chronic respiratory problems.
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration, frequency, and severity.
- Identify any risk factors, such as a family history of respiratory conditions or exposure to environmental pollutants.
- Ask about any medical conditions or medications that may contribute to breathing problems.
Physical Examination
- Listen to the patient’s lungs using a stethoscope to detect abnormal breath sounds, such as wheezing or crackles.
- Assess the patient’s respiratory rate and effort.
- Check for signs of cyanosis (bluish discoloration of the skin) or clubbing of the fingers, which may indicate chronic respiratory conditions.
Laboratory Tests
- Complete blood count (CBC): To check for signs of infection or anemia.
- Pulmonary function tests (PFTs): Measure lung capacity and airflow to assess lung function.
- Allergy testing: To identify specific allergens that may be triggering breathing problems.
- Arterial blood gas (ABG) analysis: Measures oxygen and carbon dioxide levels in the blood to evaluate respiratory function.
Diagnostic Imaging
- Chest X-ray: To assess the structure of the lungs and detect any abnormalities, such as pneumonia or lung tumors.
- Computed tomography (CT) scan: Provides detailed images of the lungs and can help diagnose conditions like pulmonary embolism or lung cancer.
- Pulmonary angiography: Invasive procedure to visualize the blood vessels in the lungs and detect any blockages.
Other Tests
- Electrocardiogram (ECG): To evaluate heart function and rule out cardiac causes of breathing problems.
- Sleep study (polysomnography): To assess breathing patterns during sleep and diagnose conditions like sleep apnea.
- Bronchoscopy: Invasive procedure to examine the airways and collect samples for further analysis.
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the patient’s progress and adjust treatment if necessary.
- Provide education on proper inhaler technique, breathing exercises, and lifestyle modifications to manage breathing problems effectively.
- Encourage patients to quit smoking and avoid exposure to environmental triggers, such as allergens or pollutants.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Breathing problems:
- Bronchodilators (e.g., Albuterol, Salbutamol):
- Cost: Generic versions can range from $10 to $50 per inhaler.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Tremors, increased heart rate.
- Severe side effects: Chest pain, irregular heartbeat.
- Drug interactions: Beta-blockers, diuretics.
- Warning: Overuse may lead to decreased effectiveness.
- Corticosteroids (e.g., Fluticasone, Budesonide):
- Cost: Generic versions can range from $20 to $100 per inhaler.
- Contraindications: Active fungal or bacterial infections.
- Side effects: Thrush (oral candidiasis), hoarseness.
- Severe side effects: Adrenal suppression, osteoporosis.
- Drug interactions: HIV protease inhibitors, ketoconazole.
- Warning: Rinse mouth after use to prevent thrush.
- Leukotriene modifiers (e.g., Montelukast, Zafirlukast):
- Cost: Generic versions can range from $20 to $100 per month.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Headache, gastrointestinal upset.
- Severe side effects: Neuropsychiatric events (rare).
- Drug interactions: Phenobarbital, rifampin.
- Warning: Monitor for changes in mood or behavior.
- Mast cell stabilizers (e.g., Cromolyn sodium, Nedocromil):
- Cost: Generic versions can range from $10 to $50 per inhaler.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Throat irritation, cough.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Requires regular use for optimal effectiveness.
- Anticholinergics (e.g., Ipratropium bromide, Tiotropium):
- Cost: Generic versions can range from $20 to $100 per inhaler.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Dry mouth, constipation.
- Severe side effects: None reported.
- Drug interactions: Other anticholinergic medications.
- Warning: Use with caution in patients with narrow-angle glaucoma.
Surgical Procedures:
- Lung volume reduction surgery: Removes damaged lung tissue to improve lung function. Cost: $50,000 to $100,000.
- Lung transplantation: Replaces a diseased lung with a healthy lung from a donor. Cost: $100,000 to $1,000,000.
Alternative Interventions
- Acupuncture: May help improve breathing and reduce anxiety. Cost: $60 to $120 per session.
- Yoga and breathing exercises: Can improve lung capacity and promote relaxation. Cost: Varies depending on the class or instructor.
- Herbal remedies: Certain herbs, such as ginger or eucalyptus, may help alleviate respiratory symptoms. Cost: Varies depending on the specific herb or supplement.
- Salt therapy (halotherapy): Inhaling salt particles may help reduce inflammation in the airways. Cost: $25 to $50 per session.
- Breathing retraining: Techniques to improve breathing patterns and reduce hyperventilation. Cost: Varies depending on the therapist or program.
Lifestyle Interventions
- Smoking cessation: Quitting smoking is crucial for improving lung health. Cost: Varies depending on the method used (e.g., nicotine replacement therapy, medications, counseling).
- Regular exercise: Physical activity can strengthen the respiratory muscles and improve lung function. Cost: Varies depending on the chosen activity (e.g., gym membership, equipment).
- Healthy diet: A balanced diet rich in fruits, vegetables, and lean proteins can support overall respiratory health. Cost: Varies depending on food choices and dietary preferences.
- Environmental modifications: Avoiding exposure to allergens, pollutants, and irritants can help reduce breathing problems. Cost: Varies depending on the necessary modifications (e.g., air purifiers, allergen-proof bedding).
- Stress management: Techniques such as meditation, mindfulness, or therapy can help reduce anxiety and improve breathing. Cost: Varies depending on the chosen method or therapist.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. It is recommended to consult with healthcare professionals for personalized treatment options and cost estimates.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R04 Breathing problem, other (ICD-10:R06.8)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Breathing problem, other effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Breathing problem, other. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Parshall, M. B., Schwartzstein, R. M., Adams, L., Banzett, R. B., Manning, H. L., Bourbeau, J., … & American Thoracic Society Committee on Dyspnea. (2012). An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. American journal of respiratory and critical care medicine, 185(4), 435-452.
- Loudon, R. G., & Murphy Jr, R. L. (1984). Lung sounds. American Review of Respiratory Disease, 130(4), 663-673.
- Lehrer, P., Feldman, J., Giardino, N., Song, H. S., & Schmaling, K. (2002). Psychological aspects of asthma. Journal of consulting and clinical psychology, 70(3), 691.
- Irwin, R. S., French, C. L., Chang, A. B., Altman, K. W., & CHEST Expert Cough Panel*. (2018). Classification of cough as a symptom in adults and management algorithms: CHEST guideline and expert panel report. Chest, 153(1), 196-209.
- Tobin, M. J., Chadha, T. S., Jenouri, G., Birch, S. J., Gazeroglu, H. B., & Sackner, M. A. (1983). Breathing patterns: 1. Normal subjects. Chest, 84(2), 202-205.
- Gruet, M. (2018). Fatigue in chronic respiratory diseases: theoretical framework and implications for real-life performance and rehabilitation. Frontiers in physiology, 9, 1285.
- Holgate, S. T. (2008). Pathogenesis of asthma. Clinical & Experimental Allergy, 38(6), 872-897.
- Vogelmeier, C. F., Criner, G. J., Martinez, F. J., Anzueto, A., Barnes, P. J., Bourbeau, J., … & Agustí, A. (2017). Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. American journal of respiratory and critical care medicine, 195(5), 557-582.
- Galli, S. J., Tsai, M., & Piliponsky, A. M. (2008). The development of allergic inflammation. Nature, 454(7203), 445-454.
- Ferkol, T., & Schraufnagel, D. (2014). The global burden of respiratory disease. Annals of the American Thoracic Society, 11(3), 404-406.
Related articles
Made in USA