Introduction
Pityriasis rosea is a common skin condition characterized by a rash that usually begins with a single, large, scaly patch known as the herald patch. It is believed to be caused by a viral infection, although the exact cause is unknown.[1] The aim of this guide is to provide a comprehensive overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for Pityriasis rosea.
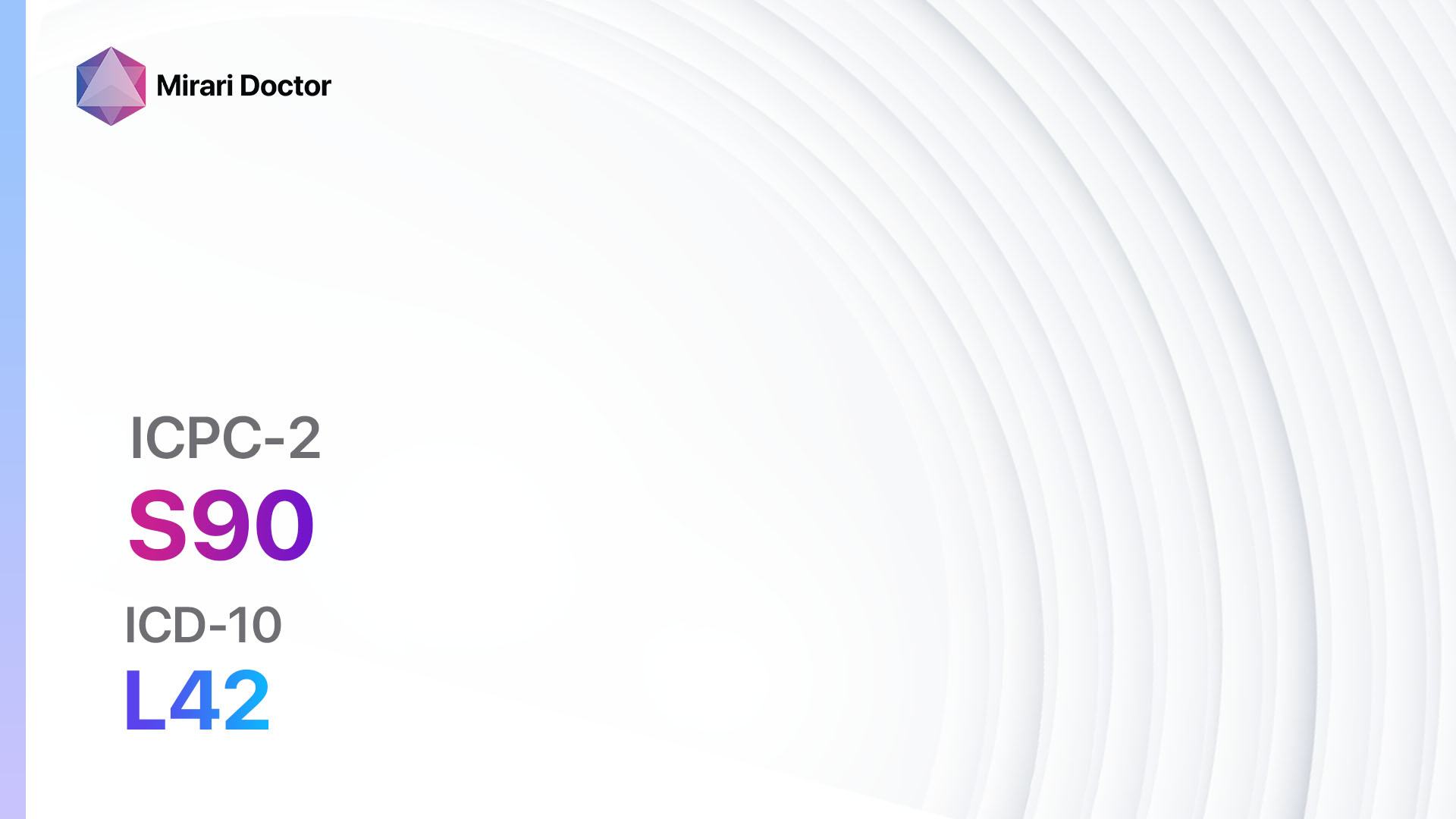
Codes
Symptoms
- Herald patch: A single, large, scaly patch that typically appears on the trunk or upper arms and is usually followed by smaller, similar patches.[2]
- Smaller patches: These smaller patches, known as secondary patches, may develop on the trunk, arms, legs, or neck. They are usually oval or round in shape and may be pink, red, or brown in color.[3]
- Itching: The rash may be accompanied by mild to moderate itching, which can be relieved with over-the-counter antihistamines or topical corticosteroids.[4]
- Flu-like symptoms: Some individuals may experience flu-like symptoms, such as fatigue, headache, sore throat, or fever, before or during the appearance of the rash.[5]
Causes
- Viral infection: Pityriasis rosea is believed to be caused by a viral infection, although the specific virus is unknown.[6]
- Immune response: It is thought that the rash is a result of an immune response to the viral infection.[7]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the appearance of the herald patch and any subsequent patches.
- Ask about any flu-like symptoms that may have preceded the rash.
- Inquire about any recent illnesses or infections.
- Determine if the patient has any known allergies or sensitivities to medications or substances.
Physical Examination
- Examine the patient’s skin for the presence of the herald patch and any secondary patches.
- Assess the size, shape, and color of the patches.
- Note any itching or discomfort reported by the patient.
- Check for any other signs or symptoms that may be present.
Determine Severity
- Pityriasis rosea is typically classified as mild, moderate, or severe based on the extent and severity of the rash.[8]
- Mild: Fewer than 10 secondary patches, minimal itching or discomfort.
- Moderate: 10-50 secondary patches, moderate itching or discomfort.
- Severe: More than 50 secondary patches, severe itching or discomfort, involvement of the face or genitals.
Laboratory Tests
- Pityriasis rosea is usually diagnosed based on the characteristic appearance of the rash and the patient’s symptoms.
- In some cases, a skin biopsy may be performed to rule out other skin conditions[9].
- Blood tests are generally not necessary for the diagnosis of pityriasis rosea.
Diagnostic Imaging
- Diagnostic imaging is not typically necessary for the diagnosis of pityriasis rosea.
Other Tests
- No other diagnostic tests are typically necessary for the diagnosis of pityriasis rosea.
Follow-up and Patient Education
- Advise the patient to monitor the progression of the rash and report any worsening symptoms or new symptoms.
- Provide information on self-care measures, such as avoiding excessive heat or sweating, using mild soaps and moisturizers, and avoiding harsh or irritating fabrics[10].
- Educate the patient about the self-limiting nature of the condition and the expected timeline for resolution of the rash.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Pityriasis rosea:
- Topical corticosteroids (e.g., hydrocortisone cream):
- Cost: $5-$20 per tube.
- Contraindications: Hypersensitivity to corticosteroids, skin infections.
- Side effects: Skin thinning, skin discoloration.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Prolonged use may lead to skin atrophy.
- Antihistamines (e.g., cetirizine, loratadine):
- Cost: $5-$15 per box.
- Contraindications: Hypersensitivity to antihistamines, narrow-angle glaucoma.
- Side effects: Drowsiness, dry mouth.
- Severe side effects: None reported.
- Drug interactions: Sedatives, alcohol.
- Warning: May cause drowsiness, avoid driving or operating heavy machinery.
- Topical calamine lotion:
- Cost: $5-$10 per bottle.
- Contraindications: Hypersensitivity to calamine lotion.
- Side effects: None reported.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: For external use only, avoid contact with eyes or mucous membranes.
- Oral corticosteroids (e.g., prednisone):
- Cost: $10-$50 per bottle.
- Contraindications: Hypersensitivity to corticosteroids, systemic fungal infections.
- Side effects: Increased appetite, weight gain.
- Severe side effects: Adrenal suppression, osteoporosis.
- Drug interactions: NSAIDs, anticoagulants.
- Warning: Prolonged use may require gradual tapering to avoid adrenal insufficiency.
- Antiviral medications (e.g., acyclovir):
- Cost: $10-$50 per bottle.
- Contraindications: Hypersensitivity to antiviral medications.
- Side effects: Nausea, vomiting.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: May cause gastrointestinal upset, take with food to minimize side effects.
Alternative Drugs:
- Topical zinc oxide cream: May help soothe itching and promote healing.
- Oral antihistamines: Can provide relief from itching and promote better sleep.
- Moisturizing creams: Help hydrate the skin and reduce dryness and itching.
- Topical antifungal creams: Used if there is a suspicion of a fungal infection.
Alternative Interventions
- Oatmeal baths: Soaking in a warm bath with colloidal oatmeal can help soothe itching and reduce inflammation. Cost: $5-$15 per box of oatmeal bath packets.
- Cold compresses: Applying cold compresses to the affected areas can provide temporary relief from itching. Cost: Free.
- Aloe vera gel: Applying aloe vera gel to the rash can help soothe itching and promote healing. Cost: $5-$15 per bottle of aloe vera gel.
- Tea tree oil: Diluted tea tree oil can be applied topically to the rash to help reduce inflammation and itching. Cost: $5-$15 per bottle of tea tree oil.
- Probiotics: Taking probiotic supplements or consuming probiotic-rich foods may help support the immune system and promote healing. Cost: $10-$30 per bottle of probiotic supplements.
Lifestyle Interventions
- Avoiding hot showers or baths: Hot water can exacerbate itching and dry out the skin. Cost: Free.
- Using mild, fragrance-free soaps: Harsh soaps and detergents can irritate the skin. Cost: $5-$10 per bottle of mild soap.
- Wearing loose-fitting, breathable clothing: Tight clothing can rub against the rash and worsen itching. Cost: Varies.
- Applying moisturizers: Regularly applying moisturizers can help hydrate the skin and reduce dryness and itching. Cost: $5-$20 per bottle of moisturizer.
- Avoiding excessive sweating: Sweating can worsen itching and irritation. Cost: Free.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – S90 Pityriasis rosea (ICD-10:L42)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting:3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD | Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD |
 |
|
Use the Mirari Cold Plasma device to treat Pityriasis rosea effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Pityriasis rosea. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Drago F, Broccolo F, Rebora A. Pityriasis rosea: an update with a critical appraisal of its possible herpesviral etiology. J Am Acad Dermatol. 2009;61(2):303-318.
- Mahajan K, Relhan V, Relhan AK, Garg VK. Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects. Indian J Dermatol. 2016;61(4):375-384.
- Urbina F, Das A, Sudy E. Clinical variants of pityriasis rosea. World J Clin Cases. 2017;5(6):203-211.
- Chuh A, Zawar V, Lee A. Atypical presentations of pityriasis rosea: case presentations. J Eur Acad Dermatol Venereol. 2005;19(1):120-126.
- Drago F, Ciccarese G, Rebora A, Broccolo F, Parodi A. Pityriasis Rosea: A Comprehensive Classification. Dermatology. 2016;232(4):431-437.
- Watanabe T, Kawamura T, Jacob SE, et al. Pityriasis rosea is associated with systemic active infection with both human herpesvirus-7 and human herpesvirus-6. J Invest Dermatol. 2002;119(4):793-797.
- Broccolo F, Drago F, Careddu AM, et al. Additional evidence that pityriasis rosea is associated with reactivation of human herpesvirus-6 and -7. J Invest Dermatol. 2005;124(6):1234-1240.
- Chuh AA. Diagnostic criteria for pityriasis rosea: a prospective case control study for assessment of validity. J Eur Acad Dermatol Venereol. 2003;17(1):101-103.
- Stulberg DL, Wolfrey J. Pityriasis rosea. Am Fam Physician. 2004;69(1):87-91.
- González LM, Allen R, Janniger CK, Schwartz RA. Pityriasis rosea: an important papulosquamous disorder. Int J Dermatol. 2005;44(9):757-764.
Related articles
Made in USA