Introduction
Chronic ulcer skin refers to a long-lasting open sore or wound on the skin that fails to heal within a reasonable time frame. It can be caused by various underlying conditions and can significantly impact a person’s quality of life[1]. The aim of this guide is to provide healthcare professionals with a comprehensive approach to diagnosing and managing chronic ulcer skin.
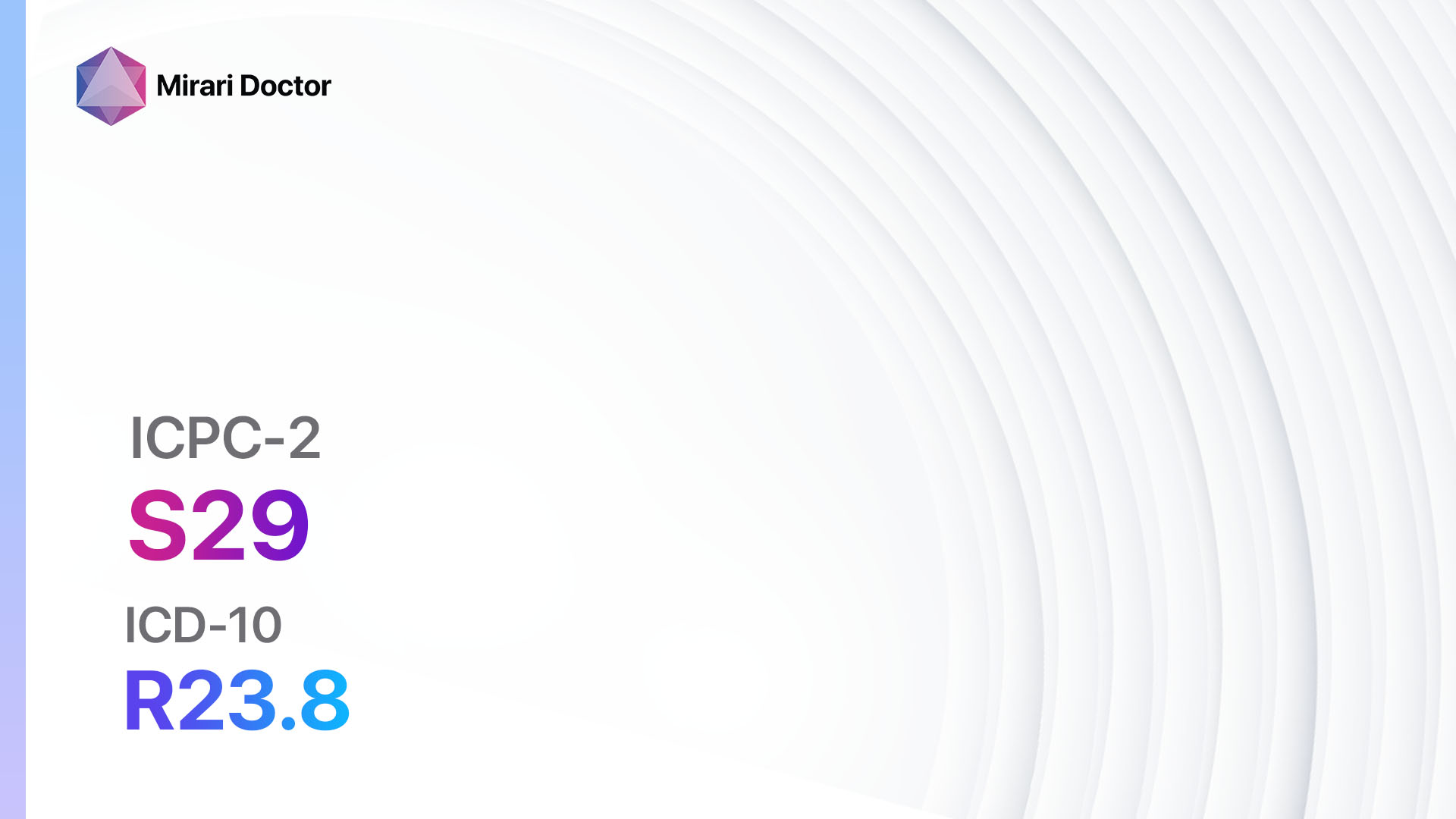
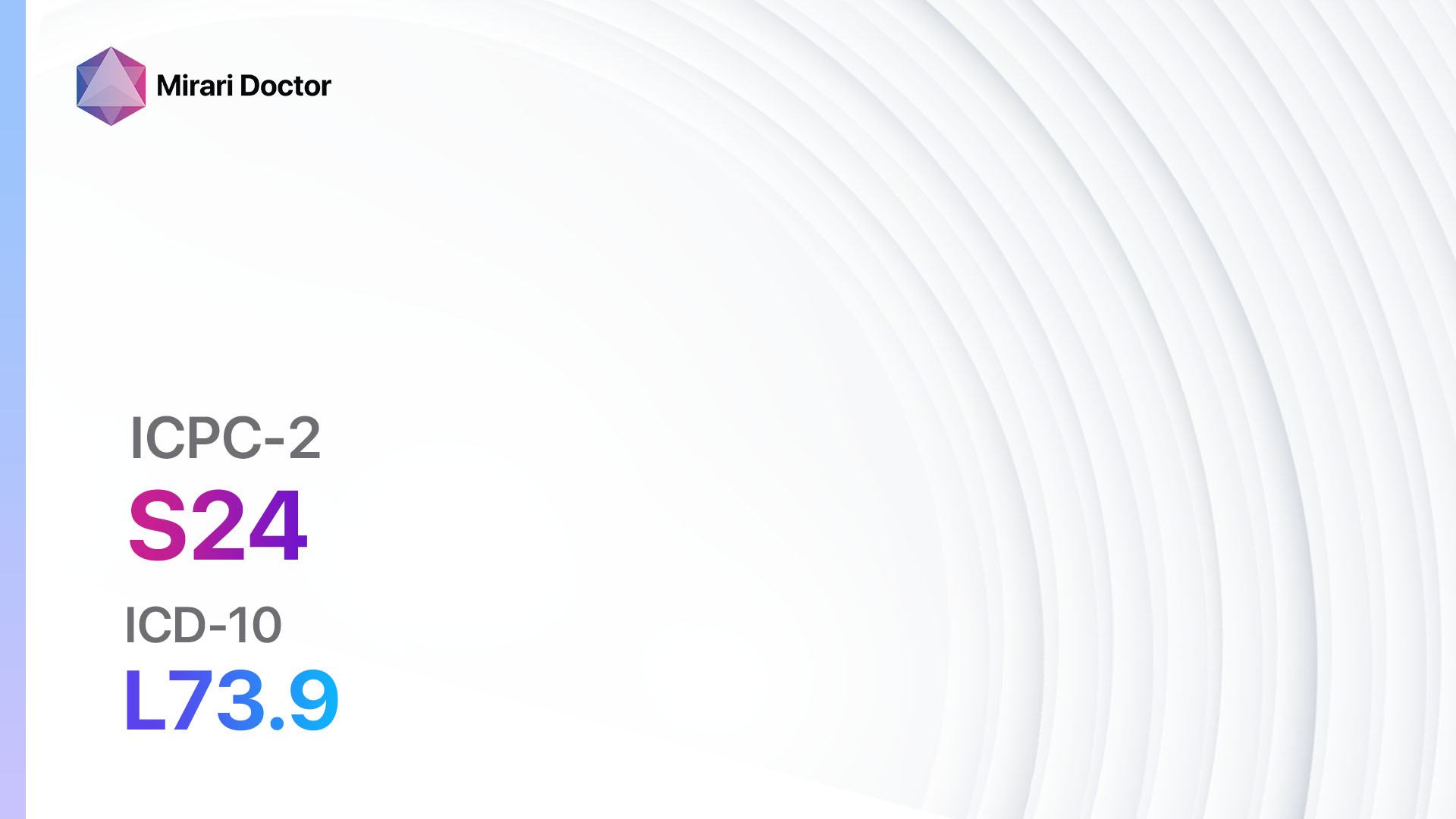
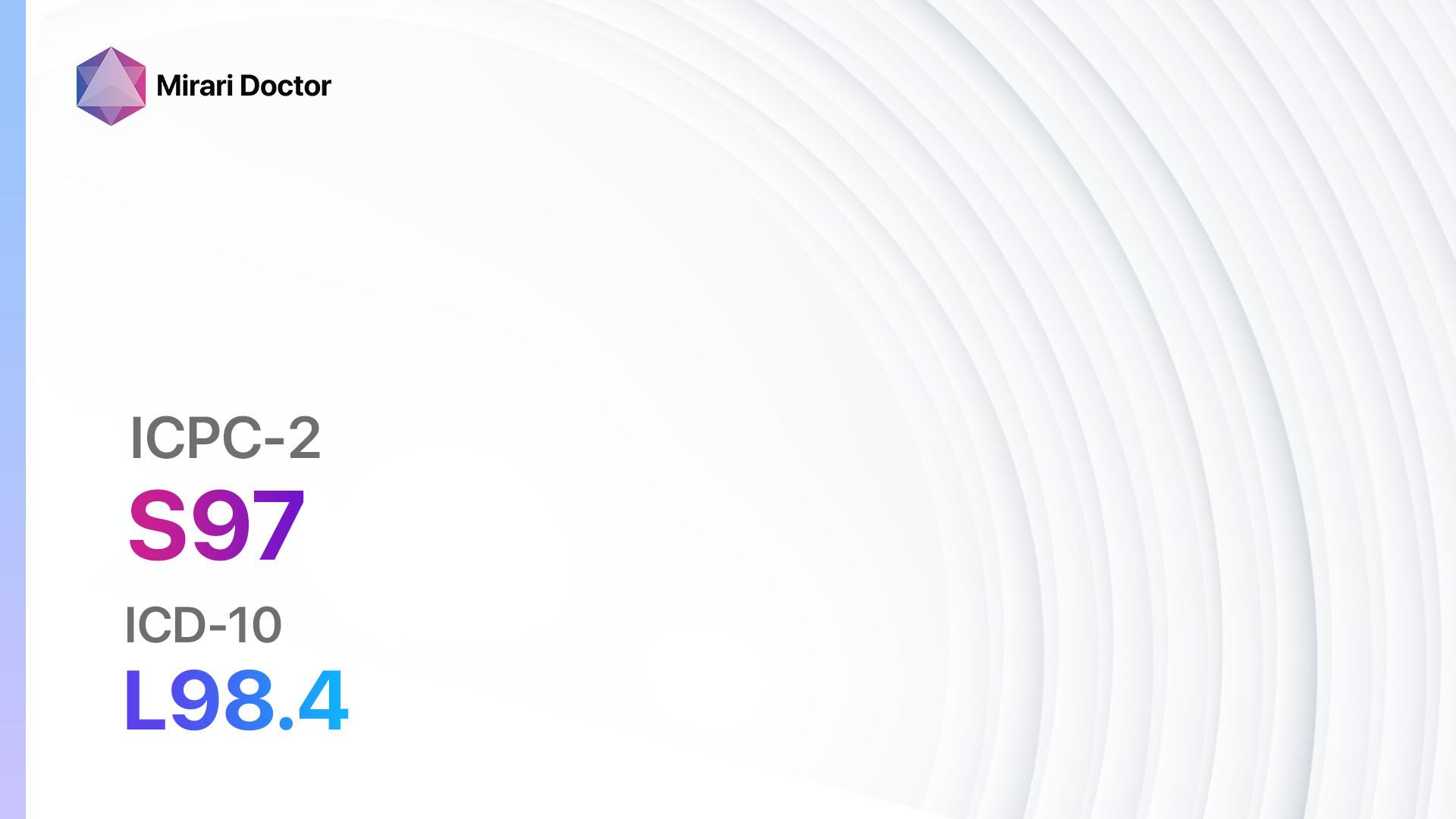
Codes
- ICPC-2 Code: S97 Chronic ulcer skin
- ICD-10 Code: L98.4 Chronic ulcer of skin, not elsewhere classified
Symptoms
- Persistent open sore or wound on the skin
- Slow or non-healing wound
- Pain or discomfort at the site of the ulcer
- Redness and inflammation around the ulcer
- Drainage or pus from the ulcer
- Foul odor from the ulcer
- Swelling or edema in the surrounding area[2]
Causes
- Venous insufficiency: Inadequate blood flow in the veins, leading to poor circulation and ulcers, commonly seen in the lower legs.
- Arterial insufficiency: Reduced blood flow in the arteries, resulting in tissue damage and ulcers, often seen in the feet and lower legs.
- Diabetic neuropathy: Nerve damage caused by diabetes, leading to loss of sensation and increased risk of ulcers.
- Pressure ulcers: Prolonged pressure on a specific area of the skin, commonly seen in bedridden or immobile individuals.
- Infection: Bacterial, fungal, or viral infections can impair wound healing and contribute to the development of chronic ulcers.
- Trauma: Physical injury or trauma to the skin can result in non-healing wounds and chronic ulcers.
- Autoimmune diseases: Conditions such as vasculitis or systemic lupus erythematosus can cause chronic ulcers[3].
Diagnostic Steps
Medical History
- Obtain a detailed medical history, including information about the duration and progression of the ulcer, previous treatments, and any underlying medical conditions.
- Identify risk factors such as diabetes, peripheral vascular disease, obesity, smoking, and immobility[4].
- Assess the patient’s overall health status, including any medications or allergies.
Physical Examination
- Inspect the ulcer for size, depth, and location.
- Assess the surrounding skin for signs of infection, inflammation, or edema.
- Palpate the ulcer to determine the presence of any underlying structures, such as bone or tendon.
- Evaluate peripheral pulses and assess for signs of arterial or venous insufficiency.
- Perform a sensory examination to assess for neuropathy[5].
Determine Severity
- Classify the ulcer based on severity and depth, using a standardized classification system such as the Wagner or the University of Texas Diabetic Wound Classification.
- Grade the ulcer based on the presence of infection, ischemia, and depth of tissue involvement.
- Classify the ulcer as mild, moderate, or severe based on the extent of tissue damage and the presence of complications[6].
Laboratory Tests
- Complete blood count (CBC): Assess for signs of infection or anemia.
- Blood glucose levels: Evaluate for diabetes or uncontrolled blood sugar levels.
- Wound culture: Collect a sample from the ulcer to identify the presence of bacteria or other microorganisms.
- Doppler ultrasound: Assess blood flow in the affected area to determine the presence of arterial or venous insufficiency.
- Biopsy: In some cases, a tissue sample may be taken for further analysis to rule out underlying malignancy or autoimmune diseases[7].
Diagnostic Imaging
- Doppler ultrasound: Assess blood flow in the affected area to determine the presence of arterial or venous insufficiency.
- X-ray: Evaluate for underlying bone involvement or osteomyelitis.
- Magnetic resonance imaging (MRI): Provide detailed images of soft tissues and help identify any deep-seated infections or abscesses[8].
Other Tests
- Ankle-brachial index (ABI): Measure the blood pressure in the ankle and compare it to the blood pressure in the arm to assess for arterial insufficiency.
- Venous duplex ultrasound: Assess the venous system for signs of venous insufficiency or deep vein thrombosis.
- Skin biopsy: Collect a sample of the affected skin for further analysis, especially in cases of suspected autoimmune diseases or malignancy[9].
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the progress of the ulcer and adjust the treatment plan as necessary.
- Educate the patient about proper wound care, including cleaning, dressing changes, and offloading techniques.
- Provide guidance on lifestyle modifications, such as smoking cessation, weight management, and regular exercise.
- Emphasize the importance of glycemic control in patients with diabetes.
- Discuss the signs and symptoms of infection or worsening of the ulcer that require immediate medical attention[10].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Chronic Ulcer Skin:
- Topical antibiotics (e.g., Mupirocin, Silver sulfadiazine):
- Cost: $10-$50 per tube.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Local skin irritation or allergic reactions.
- Severe side effects: Rare, but may include systemic allergic reactions.
- Drug interactions: Limited systemic absorption, minimal drug interactions.
- Warning: Avoid use in deep or infected wounds.
- Topical growth factors (e.g., Becaplermin):
- Cost: $300-$500 per tube.
- Contraindications: Hypersensitivity to the medication, malignancy at the application site.
- Side effects: Local skin irritation, pain, or burning sensation.
- Severe side effects: Rare, but may include systemic allergic reactions.
- Drug interactions: Limited systemic absorption, minimal drug interactions.
- Warning: Use with caution in patients with a history of malignancy.
- Systemic antibiotics (e.g., Cephalexin, Clindamycin):
- Cost: $10-$50 per course of treatment.
- Contraindications: Hypersensitivity to the medication, history of severe antibiotic-associated diarrhea or colitis.
- Side effects: Gastrointestinal upset, allergic reactions.
- Severe side effects: Rare, but may include severe allergic reactions or Clostridium difficile infection.
- Drug interactions: Potential interactions with other medications, especially those metabolized by the liver.
- Warning: Use with caution in patients with renal impairment.
- Analgesics (e.g., Acetaminophen, Nonsteroidal anti-inflammatory drugs):
- Cost: Varies depending on the specific medication.
- Contraindications: Hypersensitivity to the medication, active gastrointestinal bleeding or peptic ulcer disease.
- Side effects: Gastrointestinal upset, liver toxicity (with acetaminophen), increased risk of bleeding (with nonsteroidal anti-inflammatory drugs).
- Severe side effects: Rare, but may include severe liver toxicity or gastrointestinal bleeding.
- Drug interactions: Potential interactions with other medications, especially those metabolized by the liver.
- Warning: Use with caution in patients with renal impairment or liver disease.
- Compression therapy (e.g., Compression stockings, Unna boots):
- Cost: $20-$100 per pair of compression stockings, $10-$50 per Unna boot.
- Contraindications: Severe peripheral arterial disease, uncontrolled congestive heart failure, acute deep vein thrombosis.
- Side effects: Skin irritation, discomfort, or pressure sores.
- Severe side effects: Rare, but may include skin necrosis or worsening of arterial insufficiency.
- Drug interactions: N/A
- Warning: Use with caution in patients with compromised arterial circulation.
Surgical Procedures:
- Debridement: Removal of dead or infected tissue to promote wound healing. Cost: $500-$2,000 per procedure.
- Skin grafting: Transplantation of healthy skin to cover the ulcer and promote healing. Cost: $5,000-$15,000 per procedure.
- Negative pressure wound therapy: Application of a vacuum dressing to promote wound healing. Cost: $500-$2,000 per week of treatment.
Alternative Interventions
- Hyperbaric oxygen therapy: Involves breathing pure oxygen in a pressurized chamber to increase oxygen delivery to tissues. Cost: $200-$300 per session.
- Platelet-rich plasma therapy: Injection of concentrated platelets from the patient’s own blood to promote wound healing. Cost: $500-$1,500 per treatment.
- Electrical stimulation: Application of electrical currents to the wound to promote healing. Cost: $100-$500 per session.
- Low-level laser therapy: Use of low-energy lasers to stimulate tissue repair and reduce inflammation. Cost: $100-$300 per session.
- Topical honey: Application of medical-grade honey to the wound to promote healing. Cost: $20-$50 per jar.
Lifestyle Interventions
- Wound care: Proper cleaning, dressing changes, and offloading techniques. Cost: Varies depending on the specific wound care products.
- Smoking cessation: Quitting smoking can improve blood flow and promote wound healing. Cost: Varies depending on the smoking cessation program or aids used.
- Weight management: Achieving and maintaining a healthy weight can reduce pressure on the ulcer and improve healing. Cost: Varies depending on the weight loss program or interventions used.
- Regular exercise: Physical activity can improve circulation and promote overall health. Cost: Varies depending on the type of exercise or fitness program chosen.
- Nutritional support: A balanced diet rich in vitamins, minerals, and protein can support wound healing. Cost: Varies depending on the specific dietary requirements or supplements.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – S97 Chronic ulcer skin (ICD-10:L98.4)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD | Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD |
 |
|
Use the Mirari Cold Plasma device to treat Chronic ulcer skin effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Chronic ulcer skin. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Panuncialman, J., & Falanga, V. (2010). Unusual causes of cutaneous ulceration. Surgical Clinics of North America, 90(6), 1161-1180.
- Frykberg, R. G., & Banks, J. (2015). Challenges in the treatment of chronic wounds. Advances in wound care, 4(9), 560-582.
- Shanmugam, V. K., Angra, D., Rahimi, H., & McNish, S. (2017). Vasculitic and autoimmune wounds. Journal of vascular surgery. Venous and lymphatic disorders, 5(2), 280-292.
- Guo, S., & DiPietro, L. A. (2010). Factors affecting wound healing. Journal of dental research, 89(3), 219-229.
- Alavi, A., Sibbald, R. G., Mayer, D., Goodman, L., Botros, M., Armstrong, D. G., … & Kirsner, R. S. (2014). Diabetic foot ulcers: Part I. Pathophysiology and prevention. Journal of the American Academy of Dermatology, 70(1), 1-e1.
- Lavery, L. A., Armstrong, D. G., & Harkless, L. B. (1996). Classification of diabetic foot wounds. Journal of Foot and Ankle Surgery, 35(6), 528-531.
- Dissemond, J., Körber, A., & Grabbe, S. (2006). Differential diagnosis of leg ulcers. JDDG: Journal der Deutschen Dermatologischen Gesellschaft, 4(8), 627-634.
- Lipsky, B. A., Berendt, A. R., Cornia, P. B., Pile, J. C., Peters, E. J., Armstrong, D. G., … & Senneville, E. (2012). 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clinical infectious diseases, 54(12), e132-e173.
- Dabiri, G., Falanga, V. (2013). Connective tissue ulcers. Journal of tissue viability, 22(4), 92-102.
- Frykberg, R. G., Zgonis, T., Armstrong, D. G., Driver, V. R., Giurini, J. M., Kravitz, S. R., … & Vanore, J. V. (2006). Diabetic foot disorders: a clinical practice guideline (2006 revision). The journal of foot and ankle surgery, 45(5), S1-S66.
Related articles
Made in USA