Introduction
Skin infections are a common condition that can affect individuals of all ages. They can be caused by various factors, including bacteria, fungi, and viruses. Skin infections can range from mild to severe and may present with a variety of symptoms[1]. The aim of this guide is to provide healthcare professionals with a comprehensive approach to diagnosing and managing skin infections other than those caused by specific organisms
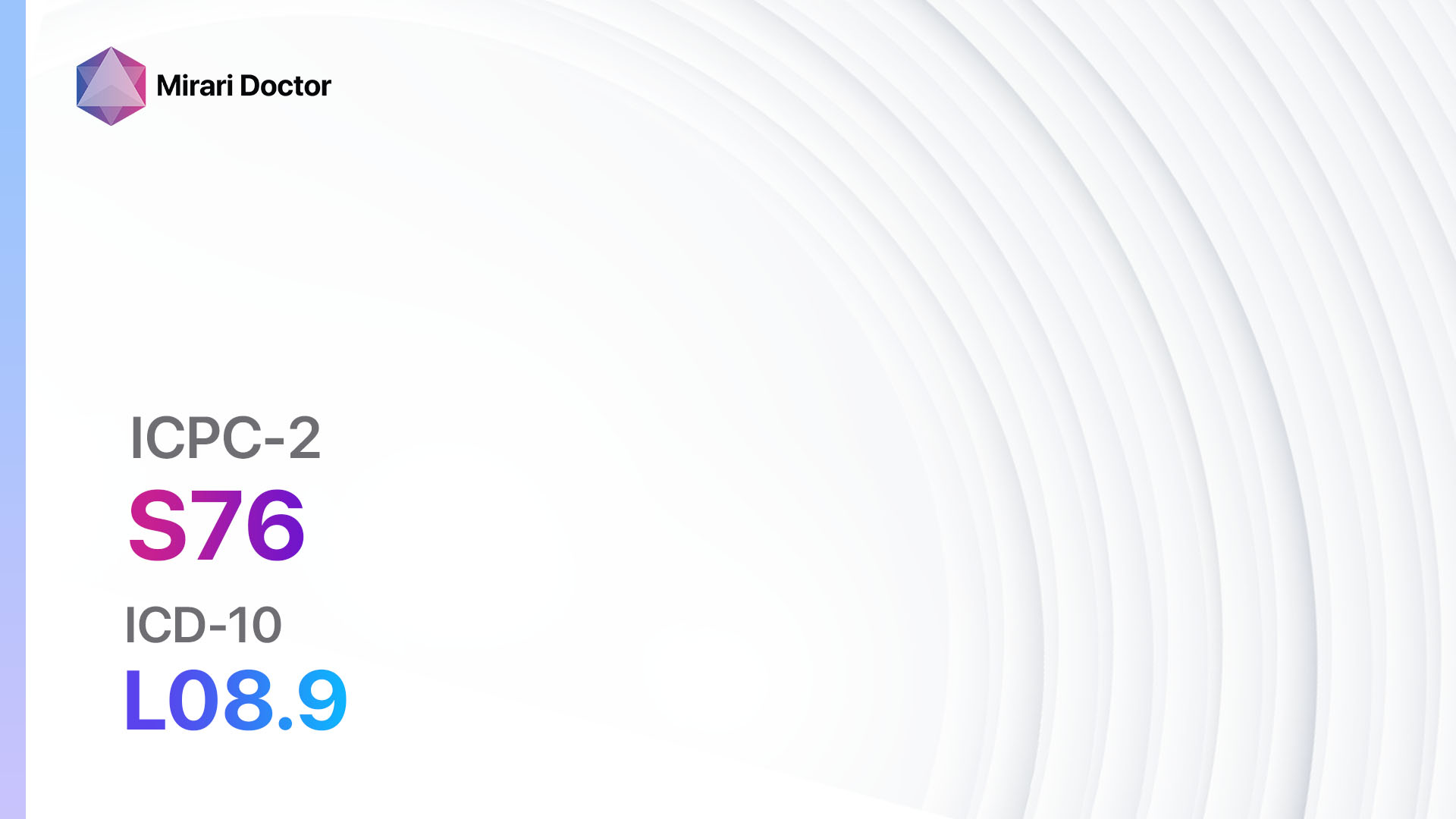
Codes
- ICPC-2 Code: S76 Skin infection other[2]
- ICD-10 Code: L08.9 Local infection of skin and subcutaneous tissue, unspecified[3]
Symptoms
- Redness and inflammation of the skin
- Swelling and tenderness
- Pain or discomfort
- Itching or a rash
- Warmth or increased skin temperature
- Pus or discharge from the affected area
- Fever or chills[4]
Causes
- Bacterial infection: Skin infections can be caused by bacteria such as Staphylococcus aureus or Streptococcus pyogenes.
- Fungal infection: Fungal infections, such as ringworm or athlete’s foot, can also affect the skin.
- Viral infection: Certain viruses, such as herpes simplex virus or varicella-zoster virus, can cause skin infections.
- Parasitic infection: Parasites like scabies mites or lice can infest the skin and cause infections.
- Allergic reactions: Skin infections can also be a result of an allergic reaction to certain substances or medications[5].
Diagnostic Steps
Medical History
- Obtain a detailed medical history, including any previous skin infections, allergies, or underlying medical conditions.
- Ask about recent exposure to potential sources of infection, such as contaminated water or contact with infected individuals.
- Inquire about any recent changes in personal hygiene practices or use of new skincare products[6].
Physical Examination
- Perform a thorough physical examination, paying close attention to the affected area.
- Assess the appearance of the skin, noting any redness, swelling, or discharge.
- Palpate the area to evaluate for tenderness or warmth.
- Look for any signs of systemic involvement, such as fever or lymph node enlargement[7].
Determine Severity
- Classify the skin infection based on severity and depth, if applicable:
- Superficial infection: Limited to the outermost layers of the skin.
- Deep infection: Involves deeper layers of the skin, such as the subcutaneous tissue or muscle.
- Systemic infection: Infection has spread beyond the skin and may involve other organs or systems[8].
Laboratory Tests
- Blood tests:
- Complete blood count (CBC) to assess for signs of infection, such as elevated white blood cell count.
- Blood cultures to identify the causative organism in severe or systemic infections.
- Wound culture: Collect a sample of the wound discharge for culture and sensitivity testing to guide antibiotic therapy.
- Skin scraping or biopsy: In cases of suspected fungal or parasitic infections, a sample of the affected skin may be taken for microscopic examination or culture[9].
Diagnostic Imaging
- In most cases, diagnostic imaging is not necessary for the diagnosis of skin infections.
- However, in severe or deep infections, imaging modalities such as ultrasound or MRI may be used to assess the extent of the infection and involvement of underlying structures[10].
Other Tests
- Polymerase chain reaction (PCR): PCR testing may be used to identify specific viral or bacterial pathogens in cases where the diagnosis is uncertain.
- Allergy testing: If an allergic reaction is suspected, allergy testing may be performed to identify the specific allergen.
Follow-up and Patient Education
- Schedule a follow-up appointment to monitor the progress of the infection and adjust treatment if necessary.
- Provide the patient with information on proper wound care, hygiene practices, and prevention strategies to minimize the risk of future infections.
- Educate the patient about the importance of completing the full course of prescribed medications and seeking medical attention if symptoms worsen or new symptoms develop.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Skin infection other:
- Antibiotics (e.g., Cephalexin, Clindamycin, Amoxicillin-Clavulanate):
- Cost: Generic versions can range from $10 to $50 for a course of treatment.
- Contraindications: Allergy to the specific antibiotic, history of severe adverse reactions.
- Side effects: Nausea, diarrhea, rash.
- Severe side effects: Severe allergic reactions, Clostridium difficile infection.
- Drug interactions: Warfarin, oral contraceptives, certain antifungal medications.
- Warning: Complete the full course of antibiotics as prescribed to prevent antibiotic resistance.
- Antifungal medications (e.g., Clotrimazole, Terbinafine, Fluconazole):
- Cost: Generic versions can range from $10 to $30 for a course of treatment.
- Contraindications: Allergy to the specific antifungal medication.
- Side effects: Skin irritation, burning or itching sensation.
- Severe side effects: Severe allergic reactions, liver toxicity.
- Drug interactions: Certain anticoagulants, oral hypoglycemic agents.
- Warning: Use antifungal medications as directed and continue treatment for the recommended duration.
- Antiviral medications (e.g., Acyclovir, Valacyclovir, Famciclovir):
- Cost: Generic versions can range from $10 to $50 for a course of treatment.
- Contraindications: Allergy to the specific antiviral medication.
- Side effects: Nausea, headache, dizziness.
- Severe side effects: Severe allergic reactions, kidney damage.
- Drug interactions: Certain medications that affect kidney function.
- Warning: Start antiviral treatment as soon as possible after the onset of symptoms for maximum effectiveness.
- Antiparasitic medications (e.g., Permethrin, Ivermectin):
- Cost: Generic versions can range from $10 to $30 for a course of treatment.
- Contraindications: Allergy to the specific antiparasitic medication.
- Side effects: Skin irritation, itching, redness.
- Severe side effects: Severe allergic reactions, neurologic symptoms.
- Drug interactions: None significant.
- Warning: Follow the instructions for proper application and use of antiparasitic medications.
- Corticosteroids (e.g., Hydrocortisone, Betamethasone, Triamcinolone):
- Cost: Generic versions can range from $10 to $30 for a course of treatment.
- Contraindications: Allergy to the specific corticosteroid medication, active infection.
- Side effects: Skin thinning, increased risk of infection, adrenal suppression.
- Severe side effects: Severe allergic reactions, Cushing’s syndrome.
- Drug interactions: None significant.
- Warning: Use corticosteroids sparingly and for a limited duration to minimize side effects.
Alternative Drugs:
- Topical antiseptics (e.g., Povidone-iodine, Chlorhexidine): Can be used as adjunctive therapy to prevent infection or promote wound healing.
- Topical antifungal creams (e.g., Miconazole, Ketoconazole): May be used for localized fungal infections.
- Topical antiviral creams (e.g., Acyclovir, Penciclovir): Can be used for localized viral infections.
- Topical corticosteroids (e.g., Hydrocortisone, Betamethasone): May provide symptomatic relief for inflammatory skin conditions.
Surgical Procedures:
- Incision and drainage: In cases of abscess formation, a healthcare professional may need to make an incision to drain the pus.
- Debridement: Removal of dead or infected tissue to promote wound healing.
Alternative Interventions
- Acupuncture: May help reduce inflammation and promote healing. Cost: $60-$120 per session.
- Herbal remedies: Certain herbs, such as tea tree oil or aloe vera, may have antimicrobial properties and can be applied topically. Cost: Varies depending on the specific product.
- Homeopathic remedies: Some homeopathic remedies, such as Calendula or Graphites, may be used to alleviate symptoms of skin infections. Cost: Varies depending on the specific product.
- Probiotics: Probiotic supplements or fermented foods may help support a healthy immune system and prevent recurrent infections. Cost: Varies depending on the specific product.
- Wet dressings: Applying wet dressings to the affected area can help soothe the skin and reduce inflammation. Cost: Minimal, as it involves using water and sterile dressings.
Lifestyle Interventions
- Good hygiene practices: Regularly washing the affected area with mild soap and water can help prevent the spread of infection.
- Avoiding irritants: Identify and avoid any potential irritants or allergens that may be contributing to the skin infection.
- Proper wound care: Keep the affected area clean and dry, and cover it with a sterile dressing if necessary.
- Healthy lifestyle habits: Maintaining a balanced diet, getting regular exercise, and managing stress can help support a healthy immune system and prevent recurrent infections.
- Avoiding tight-fitting clothing: Wearing loose-fitting clothing can help prevent friction and irritation of the skin.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – S76 Skin infection other (ICD-10:L08.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD | Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD |
 |
|
Use the Mirari Cold Plasma device to treat Skin infection other effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Skin infection other. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Ely JW, Rosenfeld S, Seabury Stone M. Diagnosis and management of tinea infections. Am Fam Physician. 2014;90(10):702-710.
- World Organization of Family Doctors (WONCA). International Classification of Primary Care, 2nd edition (ICPC-2).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10)-WHO Version for 2019.
- Hay RJ. Tinea Capitis: Current Status. Mycopathologia. 2017;182(1-2):87-93.
- Nenoff P, Krüger C, Ginter-Hanselmayer G, Tietz HJ. Mycology – an update. Part 1: Dermatomycoses: causative agents, epidemiology and pathogenesis. J Dtsch Dermatol Ges. 2014;12(3):188-209.
- Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian Dermatol Online J. 2016;7(2):77-86.
- Gupta AK, Versteeg SG, Shear NH. Onychomycosis in the 21st Century: An Update on Diagnosis, Epidemiology, and Treatment. J Cutan Med Surg. 2017;21(6):525-539.
- Rouzaud C, Hay R, Chosidow O, et al. Severe dermatophytosis and acquired or innate immunodeficiency: a review. J Fungi (Basel). 2015;2(1):4.
- Gupta AK, Foley KA, Versteeg SG. New Antifungal Agents and New Formulations Against Dermatophytes. Mycopathologia. 2017;182(1-2):127-141.
- Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide. Mycoses. 2008;51 Suppl 4:2-15.
Related articles
Made in USA