Introduction
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to symptoms such as wheezing, coughing, shortness of breath, and chest tightness. It is a common condition that affects people of all ages and can significantly impact their quality of life.[1] The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnostic steps, possible interventions, and patient education for asthma.
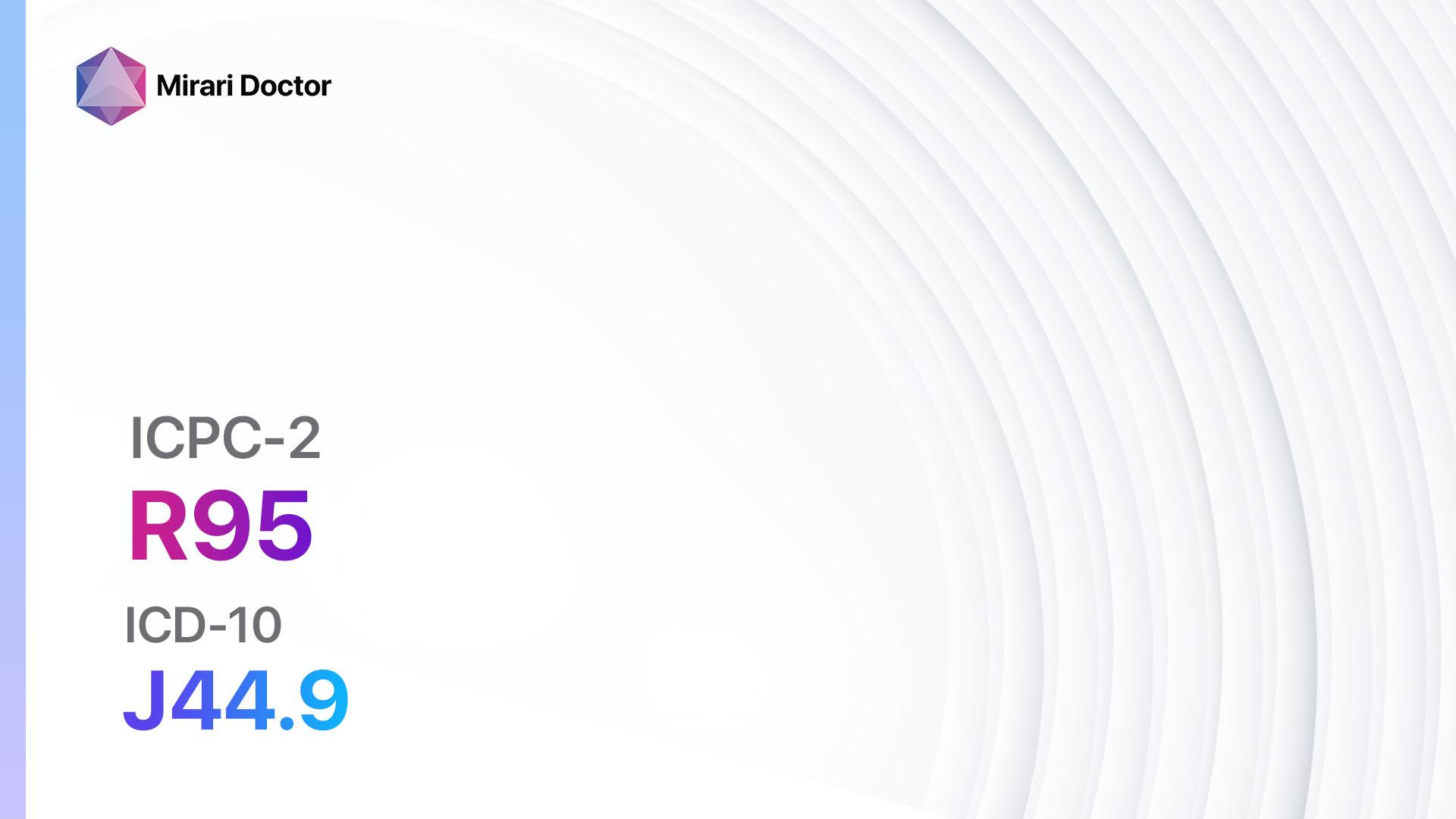
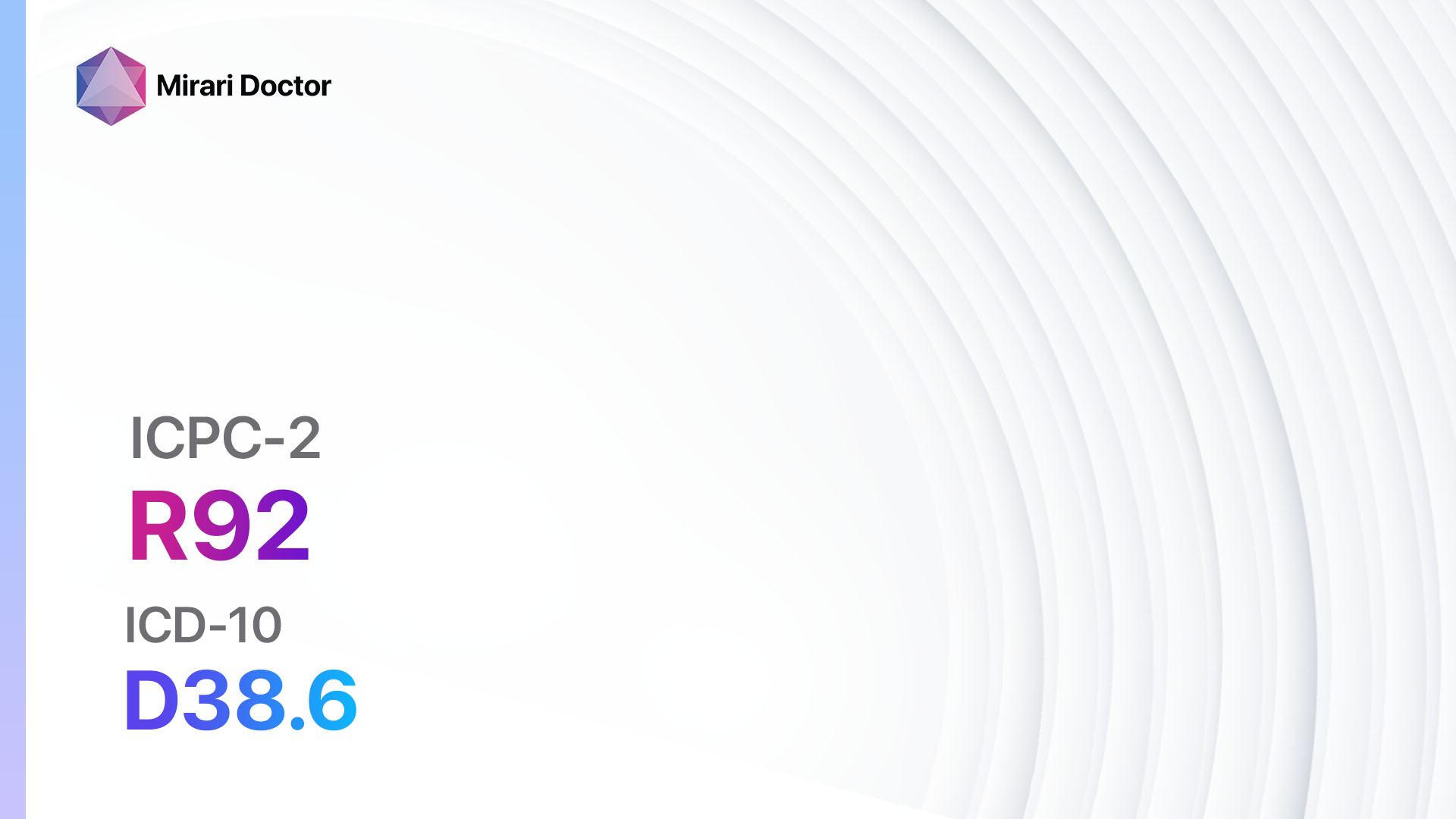
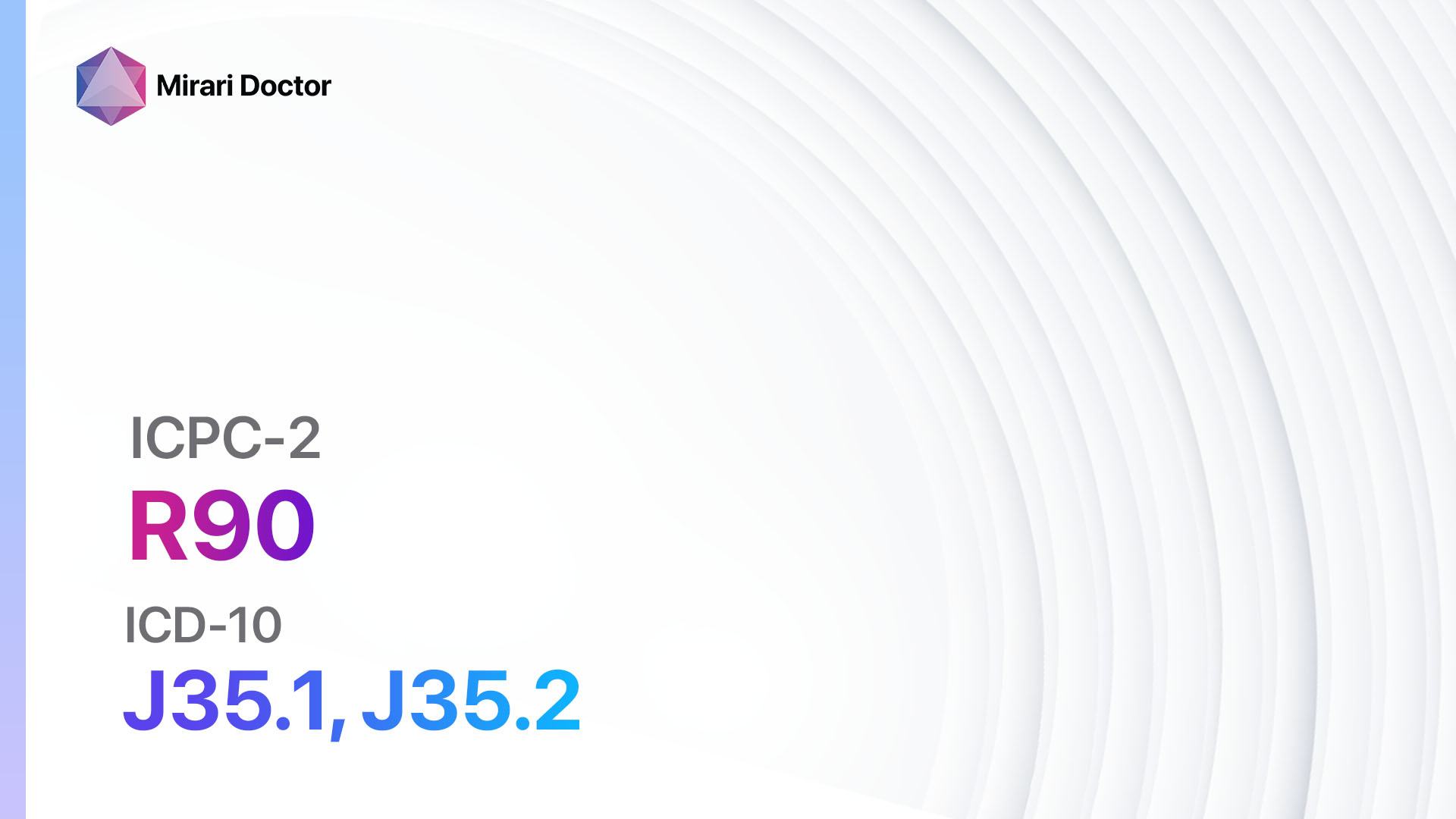
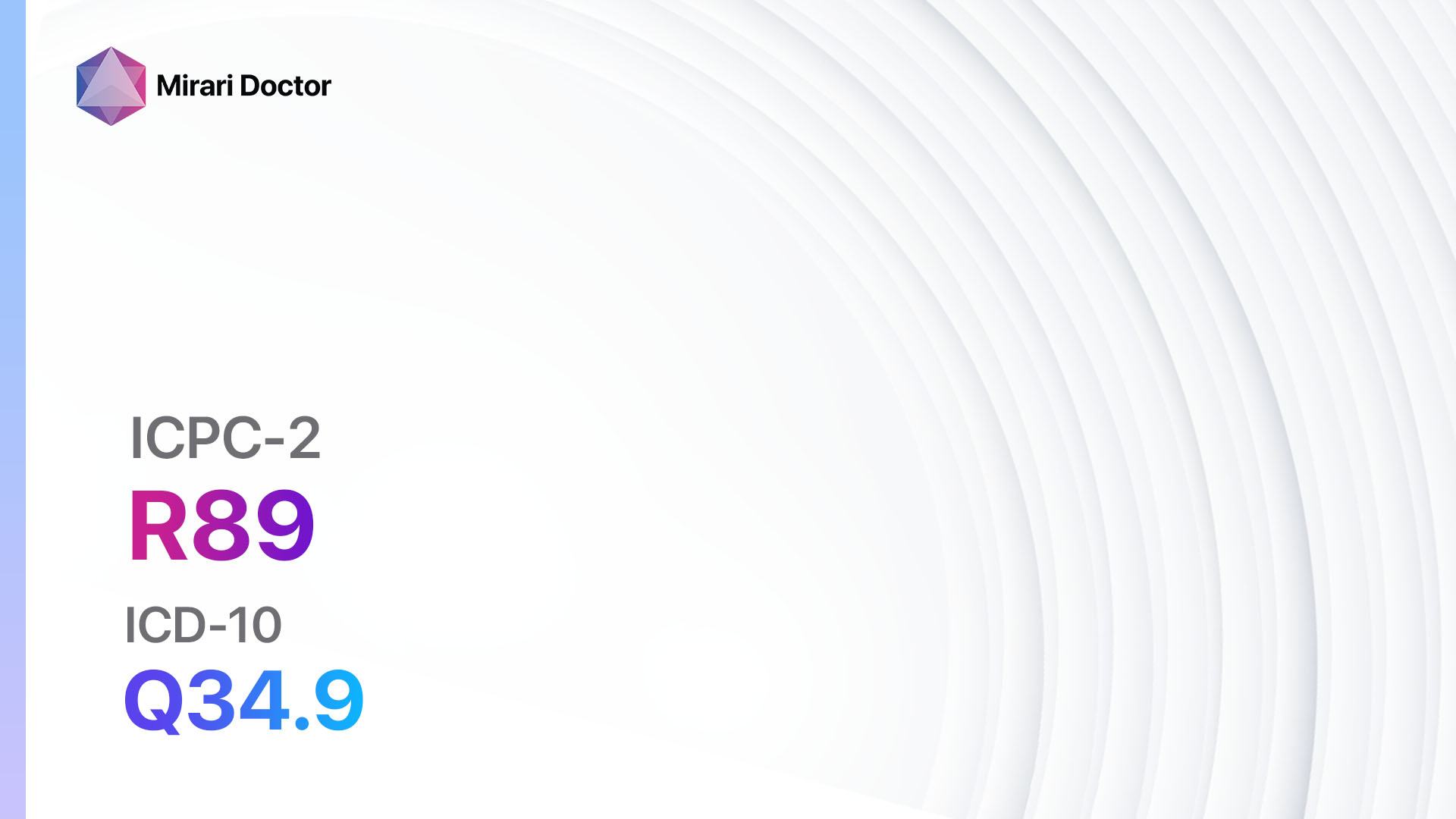
Codes
Symptoms
- Wheezing: A high-pitched whistling sound when breathing out.
- Coughing: Especially at night or early in the morning.
- Shortness of breath: Difficulty breathing, feeling out of breath.
- Chest tightness: A feeling of pressure or squeezing in the chest.[3]
Causes
- Allergens: Common triggers include pollen, dust mites, pet dander, and mold.
- Irritants: Tobacco smoke, air pollution, strong odors, and chemicals.
- Respiratory infections: Viral or bacterial infections can worsen asthma symptoms.
- Exercise-induced: Physical activity can trigger asthma symptoms.
- Cold air or changes in weather: Cold air or sudden weather changes can provoke symptoms.
- Emotions: Stress, anxiety, or strong emotions can trigger asthma attacks.[4]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including frequency, duration, and severity.
- Identify any triggers or factors that worsen the symptoms.
- Assess the impact of symptoms on daily activities and quality of life.
- Determine if there is a family history of asthma or other respiratory conditions.
- Inquire about any previous diagnoses or treatments for asthma.[5]
Physical Examination
- Listen for wheezing or other abnormal lung sounds using a stethoscope.
- Assess respiratory rate and effort.
- Check for signs of nasal congestion or postnasal drip.
- Evaluate the patient’s overall lung function using spirometry or peak flow measurements.[6]
Laboratory Tests
- Complete blood count (CBC): To assess for signs of infection or allergies.
- Allergy testing: Skin prick or blood tests to identify specific allergens.
- Sputum eosinophil count: To measure the presence of eosinophils, which indicate airway inflammation.
- Fractional exhaled nitric oxide (FeNO) test: Measures the level of nitric oxide in the breath, which is elevated in patients with asthma.[7]
Diagnostic Imaging
- Chest X-ray: To rule out other lung conditions and assess lung structure.
- High-resolution computed tomography (HRCT): Provides detailed images of the lungs to evaluate for structural abnormalities or complications.[8]
Other Tests
- Bronchoprovocation test: Measures lung function before and after exposure to a substance that triggers asthma symptoms.
- Methacholine challenge test: Measures airway responsiveness to determine the presence of asthma.
- Exercise challenge test: Evaluates lung function before and after exercise to assess exercise-induced asthma.[9]
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor symptoms and adjust treatment if necessary.
- Educate the patient about asthma triggers and how to avoid them.
- Teach proper inhaler technique and ensure the patient understands their medication regimen.
- Provide an asthma action plan to guide the patient in managing their symptoms and knowing when to seek medical help.
- Encourage the patient to monitor their peak flow measurements at home and keep a symptom diary.[10]
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Asthma:
- Inhaled corticosteroids (e.g., Fluticasone, Budesonide):
- Cost: Generic versions can range from $20 to $100 per month.
- Contraindications: None.
- Side effects: Sore throat, hoarseness, oral thrush.
- Severe side effects: Adrenal suppression, osteoporosis (with long-term use).
- Drug interactions: None.
- Warning: Rinse mouth after each use to minimize side effects.
- Short-acting beta-agonists (e.g., Albuterol, Levalbuterol):
- Cost: Generic versions can range from $10 to $50 per inhaler.
- Contraindications: None.
- Side effects: Tremor, increased heart rate.
- Severe side effects: Chest pain, irregular heart rhythm.
- Drug interactions: None.
- Warning: Should be used as a rescue medication for acute symptoms.
- Long-acting beta-agonists (e.g., Salmeterol, Formoterol):
- Cost: Generic versions can range from $50 to $150 per inhaler.
- Contraindications: None.
- Side effects: Tremor, increased heart rate.
- Severe side effects: Chest pain, irregular heart rhythm.
- Drug interactions: None.
- Warning: Should always be used in combination with an inhaled corticosteroid.
- Leukotriene modifiers (e.g., Montelukast, Zafirlukast):
- Cost: Generic versions can range from $20 to $100 per month.
- Contraindications: None.
- Side effects: Headache, upset stomach.
- Severe side effects: Mood changes, allergic reactions.
- Drug interactions: None.
- Warning: Can be used as an alternative to inhaled corticosteroids in some cases.
- Mast cell stabilizers (e.g., Cromolyn sodium, Nedocromil):
- Cost: Generic versions can range from $20 to $100 per inhaler.
- Contraindications: None.
- Side effects: Throat irritation, cough.
- Severe side effects: None.
- Drug interactions: None.
- Warning: Should be used regularly to prevent asthma symptoms.
Alternative Drugs:
- Theophylline: A bronchodilator that can be used in patients who do not respond well to inhaled medications. Cost: $20-$100 per month.
- Omalizumab: An injectable medication for severe allergic asthma. Cost: $1,000-$2,000 per month.
- Dupilumab: An injectable medication for moderate to severe asthma with eosinophilic phenotype. Cost: $3,000-$5,000 per month.
- Mepolizumab: An injectable medication for severe eosinophilic asthma. Cost: $2,000-$3,000 per month.
- Benralizumab: An injectable medication for severe eosinophilic asthma. Cost: $2,000-$3,000 per month.
Surgical Procedures:
- Bronchial thermoplasty: A procedure that uses heat to reduce the smooth muscle in the airways. Cost: $10,000-$20,000.
- Lung volume reduction surgery: Removes damaged lung tissue to improve lung function. Cost: $50,000-$100,000.
Alternative Interventions
- Acupuncture: May help improve lung function and reduce asthma symptoms. Cost: $60-$120 per session.
- Breathing exercises: Techniques such as diaphragmatic breathing and pursed lip breathing can help manage asthma symptoms. Cost: Free.
- Yoga: Incorporating yoga poses and breathing exercises can improve lung function and reduce stress. Cost: $10-$20 per class.
- Herbal supplements: Some herbs, such as Boswellia and Butterbur, may have anti-inflammatory properties that can help manage asthma symptoms. Cost: Varies depending on the specific supplement.
- Homeopathy: Some homeopathic remedies, such as Natrum sulphuricum and Arsenicum album, may be used to treat asthma symptoms. Cost: Varies depending on the specific remedy.
Lifestyle Interventions
- Avoiding triggers: Identifying and avoiding allergens, irritants, and other triggers can help prevent asthma attacks. Cost: Free.
- Maintaining a healthy weight: Losing weight if overweight or obese can improve asthma control. Cost: Varies depending on the chosen weight loss method.
- Regular exercise: Engaging in regular physical activity can improve lung function and overall fitness. Cost: Varies depending on the chosen activity.
- Quitting smoking: Smoking worsens asthma symptoms and increases the risk of complications. Cost: Varies depending on the chosen smoking cessation method.
- Stress management: Techniques such as meditation, deep breathing, and relaxation exercises can help reduce stress and manage asthma symptoms. Cost: Free.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R96 Asthma (ICD-10:J45.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Asthma effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Asthma. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2021. Available from: www.ginasthma.org
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Geneva: WHO; 2019.
- National Heart, Lung, and Blood Institute. Asthma. Available from: https://www.nhlbi.nih.gov/health-topics/asthma
- Boulet LP, Reddel HK, Bateman E, et al. The Global Initiative for Asthma (GINA): 25 years later. Eur Respir J. 2019;54(2):1900598.
- Cloutier MM, Baptist AP, Blake KV, et al. 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol. 2020;146(6):1217-1270.
- Graham BL, Steenbruggen I, Miller MR, et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200(8):e70-e88.
- Dweik RA, Boggs PB, Erzurum SC, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med. 2011;184(5):602-615.
- Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343-373.
- Coates AL, Wanger J, Cockcroft DW, et al. ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests. Eur Respir J. 2017;49(5):1601526.
- Pinnock H, Parke HL, Panagioti M, et al. Systematic meta-review of supported self-management for asthma: a healthcare perspective. BMC Med. 2017;15(1):64.
Related articles
Made in USA