Introduction
Malignant neoplasm of the bronchus/lung, also known as lung cancer, is a serious and potentially life-threatening condition. It is one of the most common types of cancer worldwide and is responsible for a significant number of cancer-related deaths.[1] The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of malignant neoplasm bronchus/lung.
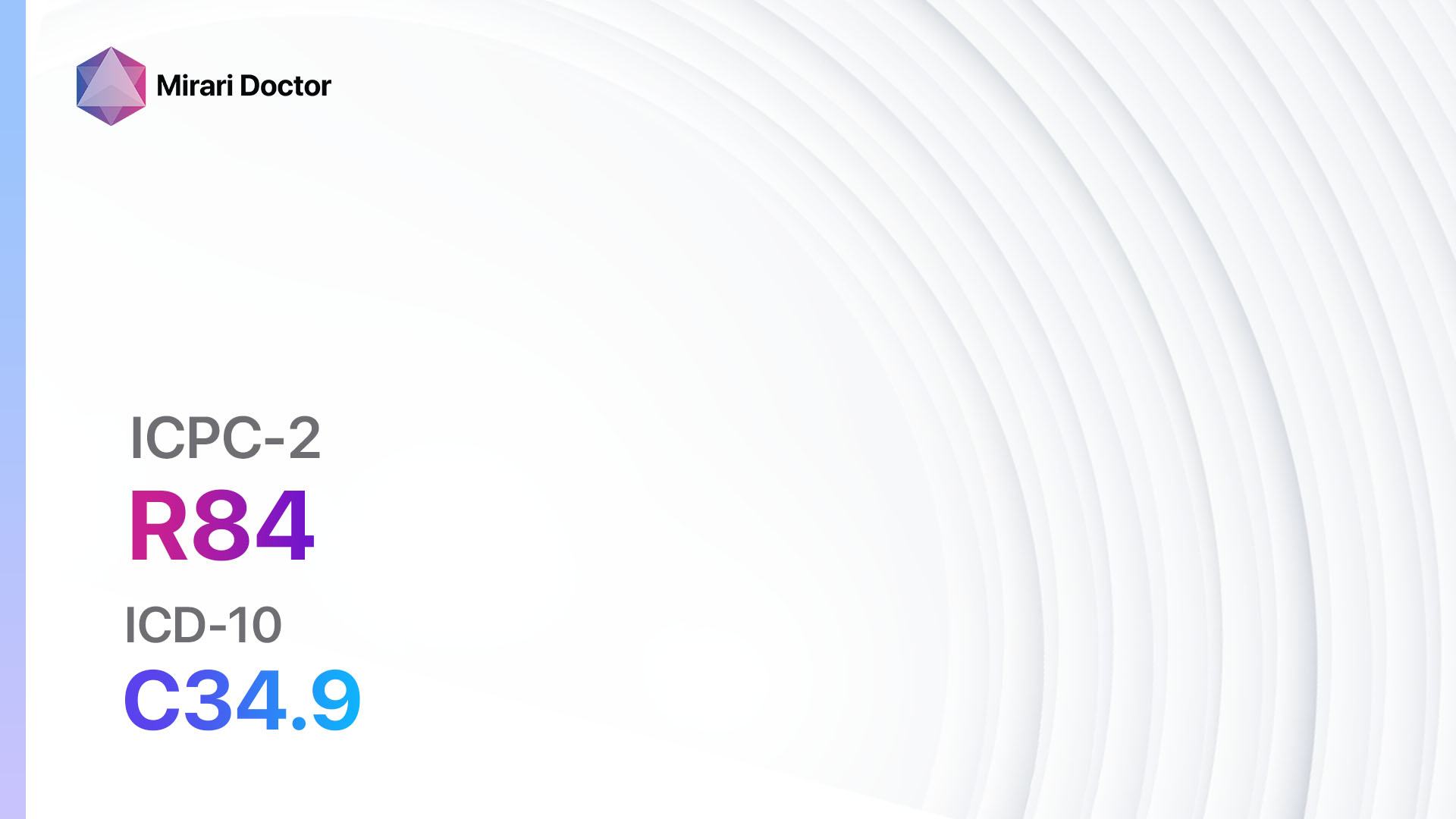
Codes
- ICPC-2 Code: R84 Malignant neoplasm bronchus/lung
- ICD-10 Code: C34.9 Malignant neoplasm of bronchus or lung, unspecified[2]
Symptoms
- Persistent cough: A chronic cough that does not go away or worsens over time.
- Shortness of breath: Difficulty breathing or feeling breathless, especially with physical activity.
- Chest pain: Dull or sharp pain in the chest, which may worsen with deep breathing, coughing, or laughing.
- Unexplained weight loss: Significant weight loss without any known cause.
- Fatigue: Feeling tired or weak, even with adequate rest.
- Hoarseness: A change in the voice, such as a deepening or raspiness.
- Wheezing: A high-pitched whistling sound when breathing.
- Coughing up blood: Blood in the sputum or phlegm.
- Recurrent respiratory infections: Frequent infections, such as bronchitis or pneumonia.[3]
Causes
- Smoking: The leading cause of lung cancer, with approximately 85% of cases attributed to smoking tobacco products.
- Secondhand smoke: Exposure to tobacco smoke from others, such as family members or coworkers.
- Radon gas: Inhalation of radon gas, a naturally occurring radioactive gas that can accumulate in homes and buildings.
- Asbestos exposure: Inhalation of asbestos fibers, commonly found in certain occupations or older buildings.
- Air pollution: Long-term exposure to air pollution, including vehicle exhaust and industrial emissions.
- Genetic factors: Certain genetic mutations or family history of lung cancer may increase the risk.[4]
Diagnostic Steps
Medical History
- Obtain a detailed medical history, including smoking history, occupational exposures, and family history of lung cancer.
- Assess for symptoms related to lung cancer, such as persistent cough, shortness of breath, chest pain, and weight loss.
- Identify any risk factors, such as smoking or exposure to environmental toxins.[5]
Physical Examination
- Perform a thorough physical examination, including auscultation of the lungs for abnormal breath sounds or wheezing.
- Assess for any signs of advanced disease, such as clubbing of the fingers or enlarged lymph nodes.[6]
Laboratory Tests
- Complete blood count (CBC): To assess for anemia or infection.
- Liver function tests (LFTs): To evaluate liver function, as lung cancer can spread to the liver.
- Kidney function tests: To assess renal function, as some cancer treatments can affect the kidneys.
- Tumor markers: Blood tests, such as carcinoembryonic antigen (CEA) or cytokeratin 19 fragment (CYFRA 21-1), may be elevated in lung cancer but are not diagnostic on their own.[7]
Diagnostic Imaging
- Chest X-ray: A basic imaging modality that can detect abnormalities in the lungs, such as masses or nodules.
- Computed tomography (CT) scan: Provides detailed cross-sectional images of the chest, allowing for better visualization of lung tumors and metastases.
- Positron emission tomography (PET) scan: A nuclear medicine imaging technique that can help determine the extent of cancer spread and identify metastatic lesions.
- Magnetic resonance imaging (MRI): May be used in specific cases to further evaluate the extent of disease or assess for brain metastases.[8]
Other Tests
- Bronchoscopy: A procedure in which a flexible tube with a camera is inserted through the nose or mouth to visualize the airways and collect tissue samples for biopsy.
- Fine-needle aspiration (FNA) biopsy: A minimally invasive procedure in which a thin needle is used to extract cells or tissue from a suspicious lung nodule or lymph node.
- Thoracentesis: Removal of fluid from the pleural space for analysis, which can help determine if cancer has spread to the lining of the lungs.
- Molecular testing: Genetic testing of tumor tissue to identify specific mutations or biomarkers that may guide treatment decisions.[9]
Follow-up and Patient Education
- Provide the patient with a clear understanding of the diagnosis, including the stage and prognosis of the disease.
- Discuss treatment options, including surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy.
- Emphasize the importance of smoking cessation and lifestyle modifications to improve overall health and treatment outcomes.
- Schedule regular follow-up appointments to monitor disease progression, response to treatment, and manage any side effects or complications.[10]
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Malignant neoplasm bronchus/lung:
- Chemotherapy (e.g., Cisplatin, Carboplatin, Paclitaxel):
- Cost: Varies depending on the specific drugs and treatment regimen.
- Contraindications: Severe kidney or liver dysfunction, pre-existing hearing loss, pregnancy.
- Side effects: Nausea, vomiting, hair loss, fatigue, decreased blood cell counts.
- Severe side effects: Kidney damage, nerve damage, severe allergic reactions.
- Drug interactions: Many potential drug interactions, including other chemotherapy drugs and medications that affect kidney function.
- Warning: Regular monitoring of blood cell counts and kidney function required.
- Targeted therapy (e.g., Erlotinib, Gefitinib, Crizotinib):
- Cost: Varies depending on the specific drugs and treatment regimen.
- Contraindications: Severe liver dysfunction, pregnancy.
- Side effects: Skin rash, diarrhea, nausea, fatigue.
- Severe side effects: Interstitial lung disease, liver toxicity.
- Drug interactions: Many potential drug interactions, including other targeted therapy drugs and medications that affect liver function.
- Warning: Regular monitoring of liver function required.
- Immunotherapy (e.g., Pembrolizumab, Nivolumab, Atezolizumab):
- Cost: Varies depending on the specific drugs and treatment regimen.
- Contraindications: Severe autoimmune disease, pregnancy.
- Side effects: Fatigue, skin rash, diarrhea, cough.
- Severe side effects: Pneumonitis, colitis, hepatitis.
- Drug interactions: Many potential drug interactions, including other immunosuppressive medications.
- Warning: Regular monitoring of immune-related adverse events required.
- Radiation therapy:
- Cost: Varies depending on the treatment regimen and duration.
- Contraindications: Pregnancy, severe lung disease.
- Side effects: Fatigue, skin changes, difficulty swallowing.
- Severe side effects: Radiation pneumonitis, esophagitis.
- Drug interactions: None.
- Warning: Regular monitoring of treatment response and potential late effects required.
- Pain management (e.g., Opioids, Nonsteroidal anti-inflammatory drugs):
- Cost: Varies depending on the specific drugs and treatment regimen.
- Contraindications: Severe respiratory depression, allergy to opioids.
- Side effects: Constipation, sedation, nausea.
- Severe side effects: Respiratory depression, addiction.
- Drug interactions: Many potential drug interactions, including other sedating medications.
- Warning: Regular monitoring of pain control and potential opioid-related side effects required.
Alternative Drugs:
- Photodynamic therapy: Uses a photosensitizing agent and light to destroy cancer cells. Cost: Varies depending on the treatment center and duration.
- Cryotherapy: Freezing of cancer cells to destroy them. Cost: Varies depending on the treatment center and duration.
- Radiofrequency ablation: Uses heat to destroy cancer cells. Cost: Varies depending on the treatment center and duration.
- Gene therapy: Experimental treatment that aims to replace or repair faulty genes. Cost: Currently not widely available.
Surgical Procedures:
- Lobectomy: Removal of a lobe of the lung. Cost: $20,000 to $40,000.
- Pneumonectomy: Removal of an entire lung. Cost: $30,000 to $60,000.
- Wedge resection: Removal of a small, wedge-shaped portion of the lung. Cost: $15,000 to $30,000.
- Lymph node dissection: Removal of nearby lymph nodes for staging purposes. Cost: $5,000 to $10,000.
- Video-assisted thoracoscopic surgery (VATS): Minimally invasive surgery using small incisions and a camera. Cost: $15,000 to $30,000.
Alternative Interventions
- Acupuncture: May help manage symptoms such as pain, nausea, and fatigue. Cost: $60-$120 per session.
- Meditation: Can help reduce stress and improve overall well-being. Cost: Free to minimal cost.
- Yoga: May improve flexibility, strength, and quality of life. Cost: $10-$20 per class or free with online resources.
- Massage therapy: Can provide relaxation and relief from muscle tension. Cost: $50-$100 per session.
- Herbal supplements: Some herbs, such as turmeric and green tea, may have potential benefits for cancer prevention and symptom management. Cost: Varies depending on the specific supplement.
Lifestyle Interventions
- Smoking cessation: Quitting smoking is crucial in improving treatment outcomes and reducing the risk of cancer recurrence. Cost: Varies depending on the method used, but can range from free (self-help resources) to several hundred dollars (nicotine replacement therapy or prescription medications).
- Healthy diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health and well-being. Cost: Varies depending on food choices, but can be affordable with proper planning and budgeting.
- Regular exercise: Engaging in regular physical activity can improve strength, endurance, and overall quality of life. Cost: Varies depending on the chosen activity, but can range from free (walking, jogging) to gym memberships or fitness classes ($20-$100 per month).
- Stress management: Techniques such as deep breathing exercises, mindfulness, or therapy can help reduce stress and improve emotional well-being. Cost: Varies depending on the chosen method, but can range from free (self-help resources) to the cost of therapy sessions ($50-$150 per session).
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R84 Malignant neoplasm bronchus/lung (ICD-10:C34.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Malignant neoplasm bronchus/lung effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Malignant neoplasm bronchus/lung. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Geneva: WHO; 2019.
- Latimer KM, Mott TF. Lung cancer: diagnosis, treatment principles, and screening. Am Fam Physician. 2015;91(4):250-256.
- Alberg AJ, Brock MV, Ford JG, Samet JM, Spivack SD. Epidemiology of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e1S-e29S.
- Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e142S-e165S.
- Spiro SG, Gould MK, Colice GL; American College of Chest Physicians. Initial evaluation of the patient with lung cancer: symptoms, signs, laboratory tests, and paraneoplastic syndromes: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest. 2007;132(3 Suppl):149S-160S.
- Grunnet M, Sorensen JB. Carcinoembryonic antigen (CEA) as tumor marker in lung cancer. Lung Cancer. 2012;76(2):138-143.
- Nair VS, Sundaram V, Desai M, Gould MK. Accuracy of models to identify lung nodule cancer risk in the National Lung Screening Trial. Am J Respir Crit Care Med. 2018;197(9):1220-1223.
- Lindeman NI, Cagle PT, Aisner DL, et al. Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors: Guideline From the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. J Mol Diagn. 2018;20(2):129-159.
- Postmus PE, Kerr KM, Oudkerk M, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl_4):iv1-iv21.
Related articles
Made in USA