Introduction
Tonsillitis acute is a common condition characterized by inflammation of the tonsils, which are located at the back of the throat. It is usually caused by a viral or bacterial infection and can result in symptoms such as sore throat, difficulty swallowing, and swollen tonsils.[1] The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of acute tonsillitis.
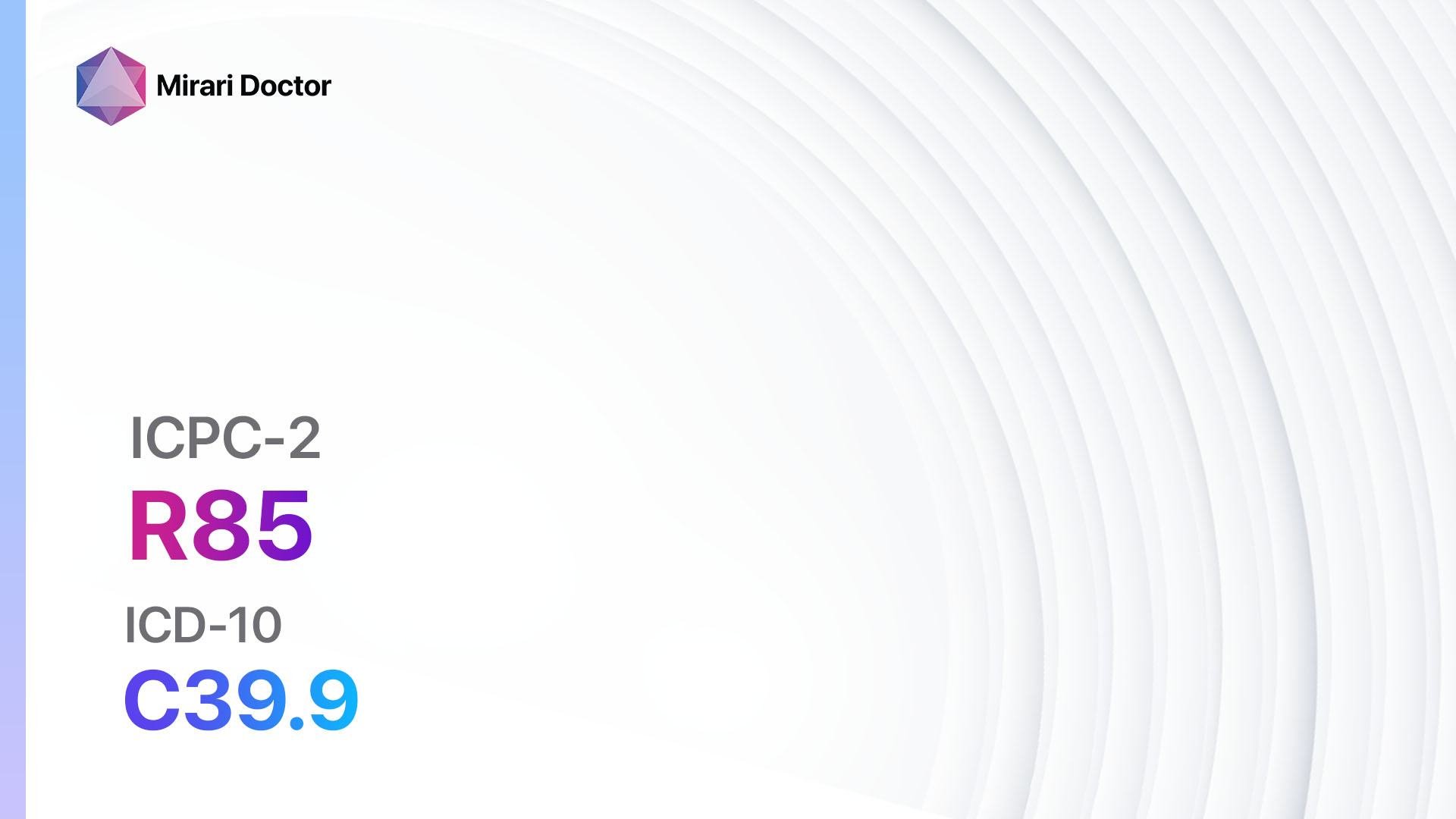
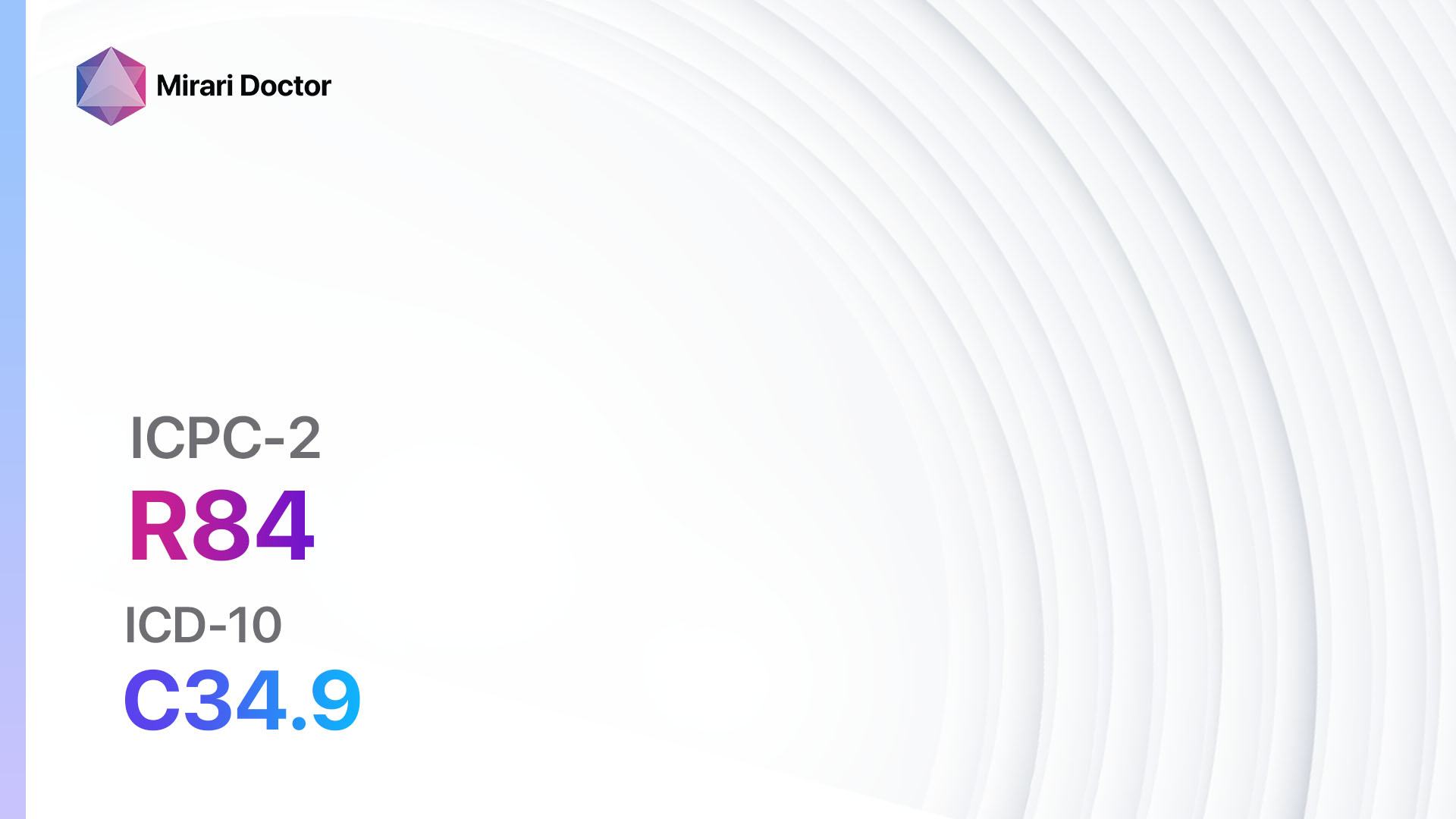
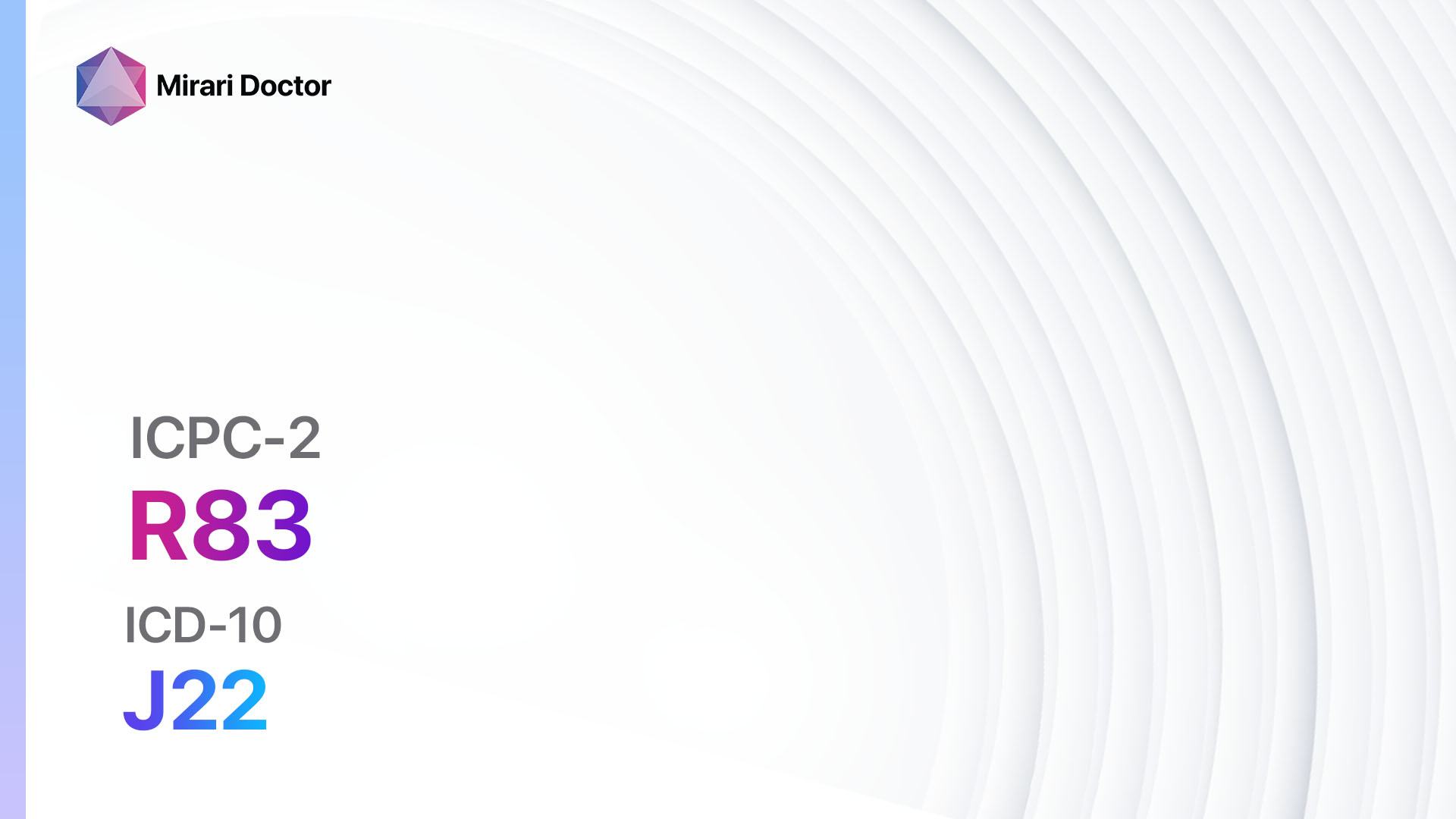
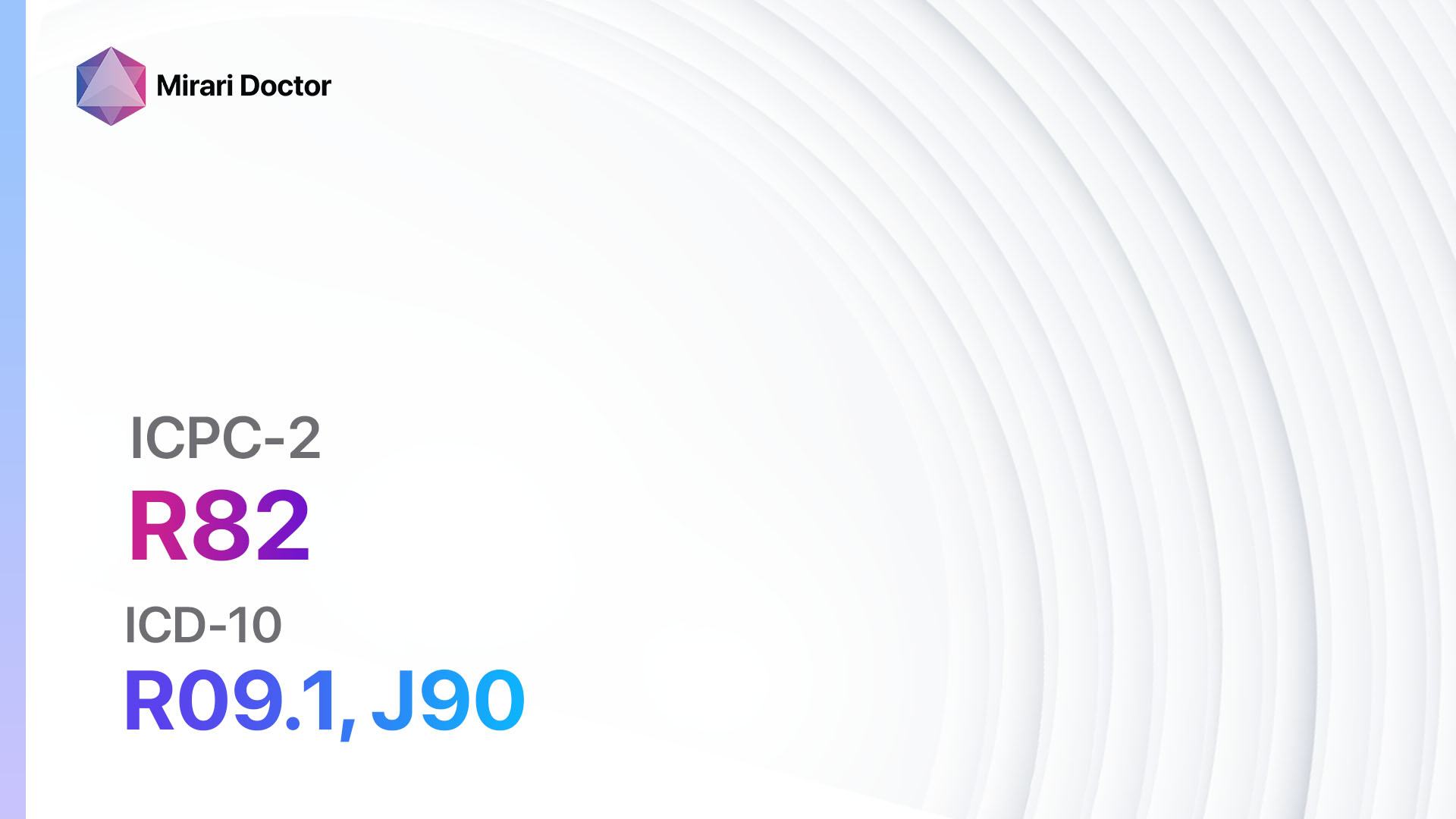
Codes
Symptoms
- Sore throat: Patients may experience pain or discomfort in the throat, especially when swallowing.
- Difficulty swallowing: Swelling of the tonsils can make it difficult to swallow food or liquids.
- Swollen tonsils: The tonsils may appear red and swollen, and may have white or yellow spots or patches.
- Fever: Patients may have a high temperature, usually above 38°C (100.4°F).
- Enlarged lymph nodes: The lymph nodes in the neck may become swollen and tender.
- Bad breath: Foul-smelling breath may be present due to the infection.[4][5]
Causes
- Viral infection: Acute tonsillitis is commonly caused by viruses, such as the common cold virus or the flu virus.
- Bacterial infection: Streptococcus pyogenes (group A streptococcus) is the most common bacterial cause of acute tonsillitis.[6]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration and severity of sore throat, difficulty swallowing, and fever.
- Ask about any recent exposure to individuals with respiratory infections.
- Inquire about any history of recurrent tonsillitis or tonsillectomy.[7]
Physical Examination
- Inspect the throat for redness, swelling, and the presence of white or yellow spots or patches on the tonsils.
- Palpate the neck to check for enlarged and tender lymph nodes.
- Measure the patient’s temperature to assess for fever.[8]
Laboratory Tests
- Rapid antigen test for streptococcal infection: This test can help confirm the presence of group A streptococcus bacteria in the throat.
- Throat culture: A throat swab may be sent to the laboratory for culture to identify the specific bacteria causing the infection.[9]
Diagnostic Imaging
- Diagnostic imaging is generally not necessary for the diagnosis of acute tonsillitis. However, in rare cases, a CT scan may be ordered if there are concerns about complications, such as peritonsillar abscess.[10]
Other Tests
- Monospot test: This blood test may be performed to rule out infectious mononucleosis, which can present with similar symptoms to acute tonsillitis.
Follow-up and Patient Education
- Advise the patient to rest and drink plenty of fluids to stay hydrated.
- Recommend over-the-counter pain relievers, such as acetaminophen or ibuprofen, to alleviate pain and reduce fever.
- Instruct the patient to avoid contact with others to prevent the spread of infection.
- Provide information on the importance of completing the full course of antibiotics if bacterial tonsillitis is diagnosed.
- Schedule a follow-up appointment to monitor the patient’s progress and ensure resolution of symptoms.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for acute tonsillitis:
- Penicillin V:
- Cost: $5-$20 for a 10-day course.
- Contraindications: Hypersensitivity to penicillin.
- Side effects: Nausea, vomiting, diarrhea.
- Severe side effects: Allergic reactions, anaphylaxis.
- Drug interactions: None significant.
- Warning: Complete the full course of antibiotics as prescribed.
- Amoxicillin:
- Cost: $5-$20 for a 10-day course.
- Contraindications: Hypersensitivity to penicillin.
- Side effects: Nausea, vomiting, diarrhea.
- Severe side effects: Allergic reactions, anaphylaxis.
- Drug interactions: None significant.
- Warning: Complete the full course of antibiotics as prescribed.
- Cephalosporins (e.g., cephalexin):
- Cost: $10-$30 for a 10-day course.
- Contraindications: Hypersensitivity to cephalosporins.
- Side effects: Nausea, vomiting, diarrhea.
- Severe side effects: Allergic reactions, anaphylaxis.
- Drug interactions: None significant.
- Warning: Complete the full course of antibiotics as prescribed.
- Macrolides (e.g., azithromycin):
- Cost: $10-$40 for a 5-day course.
- Contraindications: Hypersensitivity to macrolides.
- Side effects: Nausea, vomiting, diarrhea.
- Severe side effects: Prolonged QT interval, liver toxicity.
- Drug interactions: None significant.
- Warning: Complete the full course of antibiotics as prescribed.
- Clindamycin:
- Cost: $20-$50 for a 10-day course.
- Contraindications: Hypersensitivity to clindamycin.
- Side effects: Nausea, vomiting, diarrhea.
- Severe side effects: Clostridium difficile infection, severe allergic reactions.
- Drug interactions: None significant.
- Warning: Complete the full course of antibiotics as prescribed.
Alternative Drugs:
- Erythromycin: An alternative for patients with penicillin allergy.
- Clarithromycin: An alternative for patients with penicillin allergy.
- Doxycycline: An alternative for patients with penicillin allergy.
Surgical Procedures:
- Tonsillectomy: Surgical removal of the tonsils may be considered in cases of recurrent or chronic tonsillitis that significantly affects the patient’s quality of life. Cost: $3,000-$6,000.
Alternative Interventions
- Saltwater gargles: Gargling with warm saltwater can help soothe a sore throat. Cost: Minimal.
- Herbal teas: Drinking herbal teas, such as chamomile or ginger tea, may provide relief from symptoms. Cost: Varies depending on the specific tea.
- Honey and lemon: Mixing honey and lemon in warm water can help soothe a sore throat. Cost: Minimal.
- Probiotics: Taking probiotic supplements may help boost the immune system and reduce the severity of symptoms. Cost: $10-$30 per month.
- Homeopathic remedies: Some individuals find relief from acute tonsillitis symptoms with homeopathic remedies, such as Belladonna or Mercurius solubilis. Cost: Varies depending on the specific remedy.
Lifestyle Interventions
- Rest: Adequate rest is essential for the body to recover from the infection. Cost: Minimal.
- Hydration: Drinking plenty of fluids helps keep the throat moist and can alleviate discomfort. Cost: Minimal.
- Warm compress: Applying a warm compress to the neck can help reduce swelling and relieve pain. Cost: Minimal.
- Avoiding irritants: Encourage the patient to avoid smoking, exposure to secondhand smoke, and other irritants that can worsen symptoms. Cost: Minimal.
- Healthy diet: Consuming a balanced diet rich in fruits and vegetables can support the immune system. Cost: Varies depending on food choices.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R76 Tonsillitis acute (ICD-10:J03.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Tonsillitis acute effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Tonsillitis acute. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Georgalas CC, Tolley NS, Narula PA. Tonsillitis. BMJ Clin Evid. 2014;2014:0503.
- World Health Organization. International Classification of Primary Care, Second edition (ICPC-2). 2003.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). 2019.
- Stelter K. Tonsillitis and sore throat in children. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2014;13:Doc07.
- Bathala S, Eccles R. A review on the mechanism of sore throat in tonsillitis. J Laryngol Otol. 2013;127(3):227-232.
- Pichichero ME. Group A streptococcal tonsillopharyngitis: cost-effective diagnosis and treatment. Ann Emerg Med. 1995;25(3):390-403.
- Windfuhr JP, Toepfner N, Steffen G, Waldfahrer F, Berner R. Clinical practice guideline: tonsillitis I. Diagnostics and nonsurgical management. Eur Arch Otorhinolaryngol. 2016;273(4):973-987.
- Choby BA. Diagnosis and treatment of streptococcal pharyngitis. Am Fam Physician. 2009;79(5):383-390.
- Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55(10):e86-e102.
- Galioto NJ. Peritonsillar abscess. Am Fam Physician. 2017;95(8):501-506.
Related articles
Made in USA