Introduction
Sneezing and nasal congestion are common symptoms that can be caused by various factors, including allergies, infections, and irritants. These symptoms can significantly impact a person’s quality of life, affecting their ability to breathe properly and causing discomfort[1]. The aim of this guide is to provide healthcare professionals with a comprehensive approach to diagnosing and managing sneezing and nasal congestion in patients.
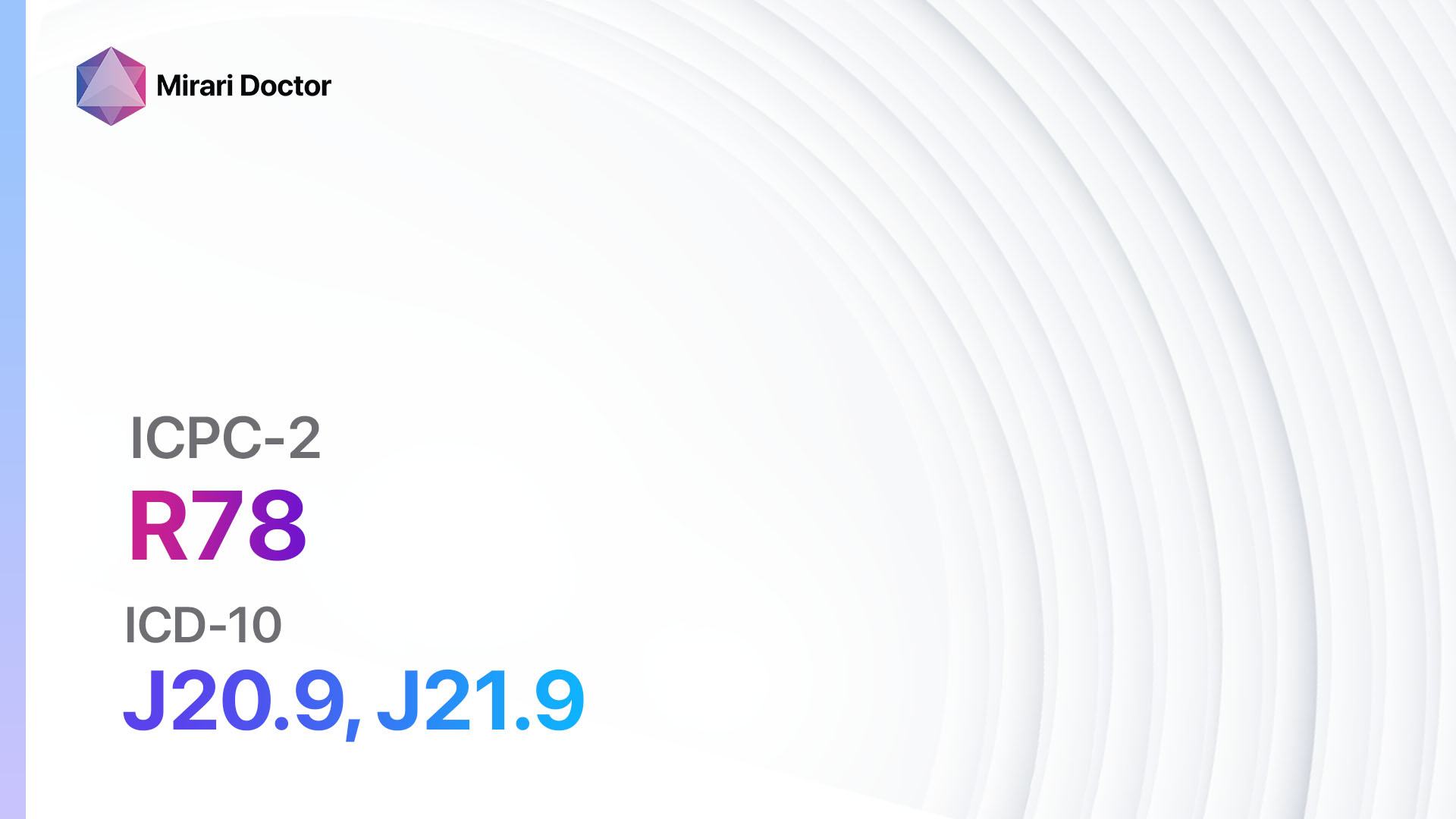
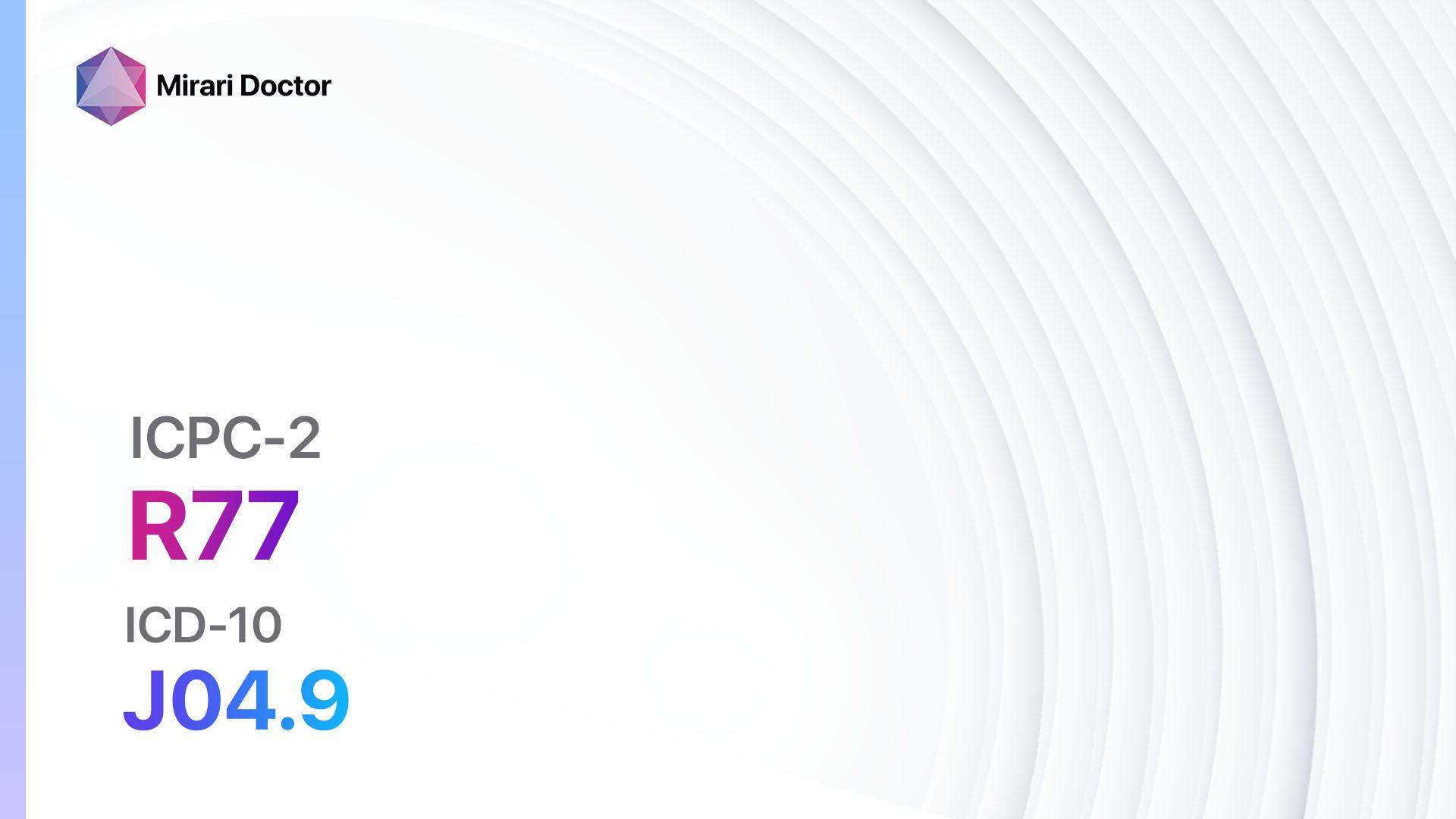
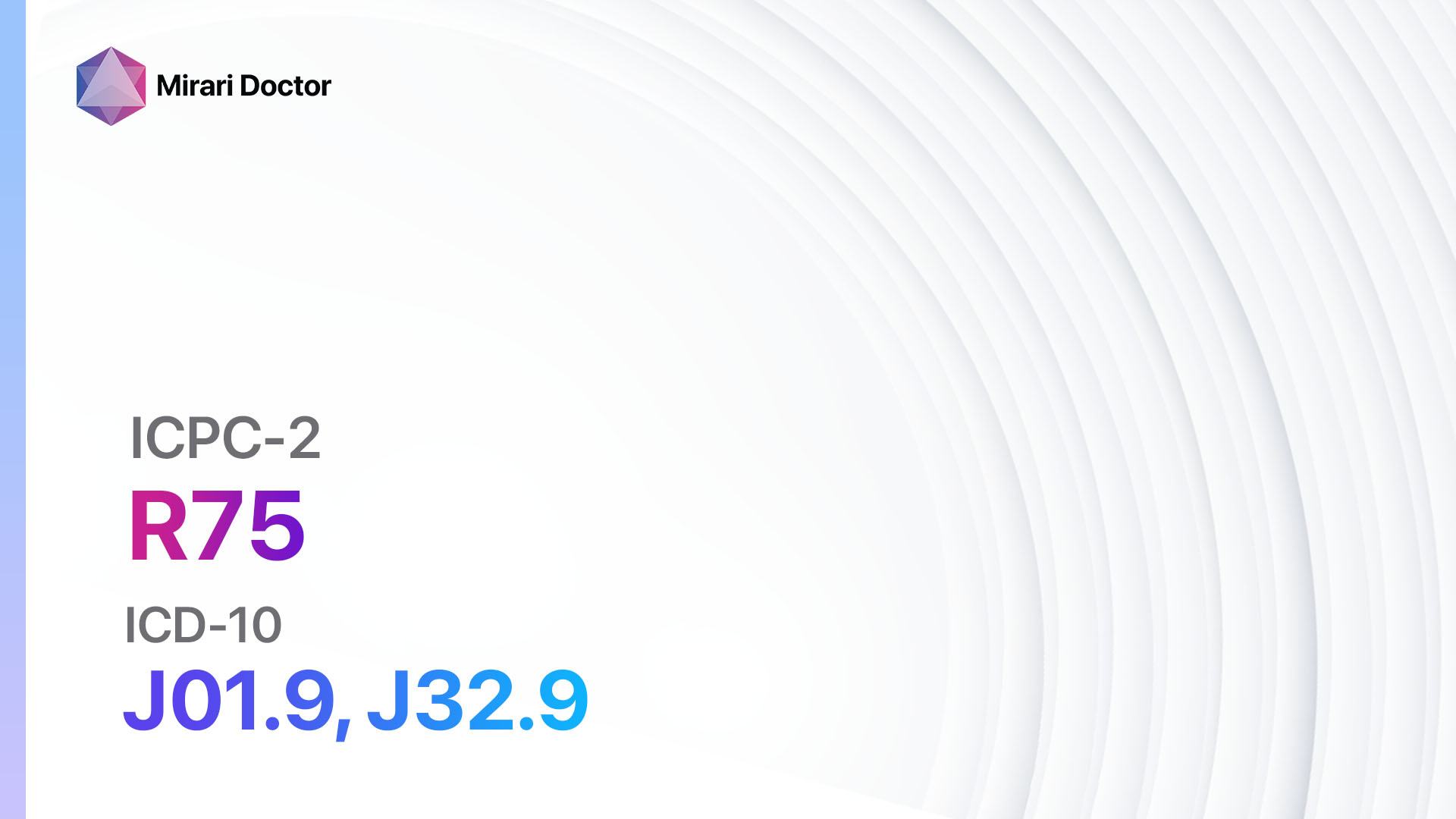
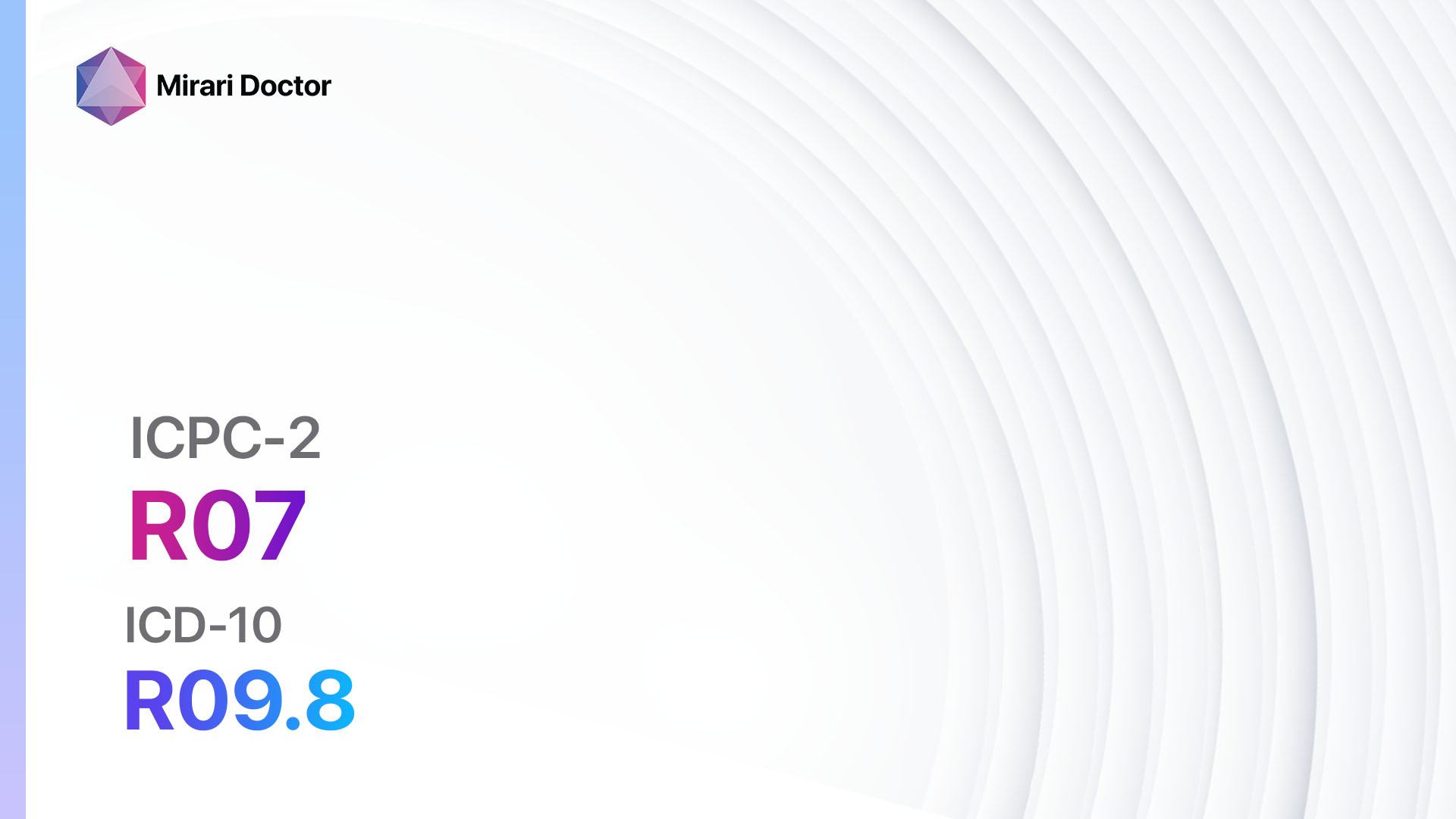
Codes
- ICPC-2 Code: R07 Sneezing/nasal congestion[2]
- ICD-10 Code: R09.8 Other specified symptoms and signs involving the circulatory and respiratory systems[3]
Symptoms
- Sneezing: Uncontrollable, sudden expulsion of air through the nose and mouth[4].
- Nasal congestion: Blockage or stuffiness in the nasal passages[5].
Causes
- Allergies: Allergic rhinitis, also known as hay fever, is a common cause of sneezing and nasal congestion. It occurs when the immune system overreacts to allergens such as pollen, dust mites, or pet dander[6].
- Infections: Viral or bacterial infections, such as the common cold or sinusitis, can cause sneezing and nasal congestion[7].
- Irritants: Exposure to irritants like cigarette smoke, strong odors, or air pollution can trigger sneezing and nasal congestion[8].
- Structural abnormalities: Deviated septum or nasal polyps can obstruct the nasal passages and lead to congestion[9].
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the frequency, duration, and severity of sneezing and nasal congestion.
- Ask about any associated symptoms, such as itching, runny nose, or postnasal drip.
- Inquire about potential triggers, such as exposure to allergens or irritants.
- Assess the patient’s medical history, including any previous diagnoses of allergies, sinusitis, or other respiratory conditions.
- Identify any relevant risk factors, such as a family history of allergies or a history of smoking[10].
Physical Examination
- Inspect the nasal passages for signs of inflammation, swelling, or discharge.
- Palpate the sinuses to check for tenderness or pain.
- Evaluate the throat and tonsils for signs of infection or inflammation.
- Assess the lungs for any abnormal breath sounds that may indicate an underlying respiratory condition.
- Examine the eyes and skin for signs of allergic reactions, such as redness or hives.
Laboratory Tests
- Allergy testing: Skin prick tests or blood tests (e.g., IgE levels) can help identify specific allergens that may be causing the symptoms.
- Complete blood count (CBC): Elevated white blood cell count may indicate an infection.
- Nasal swab: Collect a sample from the nasal passages to test for viral or bacterial infections.
- C-reactive protein (CRP): Elevated levels may indicate inflammation.
Diagnostic Imaging
- X-ray: Useful for evaluating the sinuses and ruling out structural abnormalities.
- CT scan: Provides detailed images of the nasal passages and sinuses, helping to identify any obstructions or abnormalities.
- MRI: May be used to assess the nasal passages and sinuses in more detail, particularly in cases where a CT scan is contraindicated.
Other Tests
- Nasal endoscopy: A thin, flexible tube with a light and camera is inserted into the nasal passages to visualize any abnormalities or obstructions.
- Pulmonary function tests: Assess lung function and rule out underlying respiratory conditions.
- Allergen challenge test: In cases of suspected allergies, exposing the patient to specific allergens in a controlled environment can help confirm the diagnosis.
Follow-up and Patient Education
- Schedule a follow-up appointment to review test results and discuss treatment options.
- Provide patient education on the causes of sneezing and nasal congestion, including allergens, infections, and irritants.
- Discuss strategies to minimize exposure to triggers, such as using air purifiers, avoiding cigarette smoke, and practicing good hygiene.
- Explain the importance of adhering to prescribed medications and following up with healthcare professionals for ongoing management.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for sneezing/nasal congestion:
- Antihistamines (e.g., Loratadine, Cetirizine, Fexofenadine):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: Hypersensitivity to antihistamines.
- Side effects: Drowsiness, dry mouth, dizziness.
- Severe side effects: Rare, but may include allergic reactions or difficulty breathing.
- Drug interactions: Sedatives, tranquilizers, or other medications that cause drowsiness.
- Warning: Avoid driving or operating machinery if experiencing drowsiness.
- Decongestants (e.g., Phenylephrine, Pseudoephedrine):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: High blood pressure, heart disease, glaucoma.
- Side effects: Increased heart rate, elevated blood pressure, restlessness.
- Severe side effects: Rare, but may include severe allergic reactions or difficulty breathing.
- Drug interactions: MAO inhibitors, beta blockers, or other medications that increase blood pressure.
- Warning: Limit use to short-term relief (3-5 days) to avoid rebound congestion.
- Intranasal corticosteroids (e.g., Fluticasone, Budesonide, Mometasone):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to corticosteroids.
- Side effects: Nasal irritation, nosebleeds, headache.
- Severe side effects: Rare, but may include adrenal suppression or increased risk of infection.
- Drug interactions: None significant.
- Warning: Proper technique for nasal spray administration should be demonstrated.
- Leukotriene receptor antagonists (e.g., Montelukast):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to leukotriene receptor antagonists.
- Side effects: Headache, gastrointestinal upset.
- Severe side effects: Rare, but may include psychiatric symptoms or liver problems.
- Drug interactions: None significant.
- Warning: Monitor for any changes in mood or behavior.
- Nasal saline irrigation:
- Cost: $5-$20 for a saline nasal rinse kit.
- Contraindications: None.
- Side effects: Temporary stinging or burning sensation.
- Severe side effects: None.
- Drug interactions: None.
- Warning: Proper technique for nasal irrigation should be demonstrated.
Alternative Drugs:
- Anticholinergic nasal sprays (e.g., Ipratropium bromide): Can help reduce nasal secretions.
- Mast cell stabilizers (e.g., Cromolyn sodium): Useful for allergic rhinitis.
- Nasal antihistamine sprays (e.g., Azelastine): Provide relief for sneezing and itching.
- Oral corticosteroids (e.g., Prednisone): Reserved for severe cases or short-term use.
Surgical Procedures:
- Septoplasty: Corrects a deviated septum that may be causing nasal congestion. Cost: $3,000-$7,000.
- Turbinoplasty: Reduces the size of nasal turbinates to improve airflow. Cost: $2,000-$5,000.
- Endoscopic sinus surgery: Removes nasal polyps or clears blocked sinuses. Cost: $5,000-$10,000.
Alternative Interventions
- Acupuncture: May help relieve nasal congestion and improve overall well-being. Cost: $60-$120 per session.
- Nasal irrigation with herbal solutions: Using herbal solutions in nasal rinses may provide additional relief. Cost: Varies depending on the specific herbs used.
- Steam inhalation: Breathing in steam from hot water or essential oils can help alleviate nasal congestion. Cost: Minimal, using household items.
- Probiotics: Some evidence suggests that certain probiotics may help reduce the severity of allergic rhinitis symptoms. Cost: Varies depending on the specific probiotic supplement.
- Butterbur: A herbal supplement that may have antihistamine properties. Cost: Varies depending on the brand and dosage.
Lifestyle Interventions
- Avoidance of triggers: Identify and avoid allergens or irritants that may be causing the symptoms.
- Humidification: Use a humidifier to add moisture to the air and reduce nasal dryness. Cost: $20-$100.
- Nasal strips: External nasal strips can help open up the nasal passages and improve airflow. Cost: $5-$15 for a pack.
- Elevating the head: Sleeping with an extra pillow or using a wedge pillow can help reduce nasal congestion during sleep. Cost: Minimal, using household items.
- Regular exercise: Physical activity can help improve overall respiratory health and reduce nasal congestion. Cost: Varies depending on the chosen exercise.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – R07 Sneezing/nasal congestion (ICD-10:R09.8)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Sneezing/nasal congestion effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Sneezing/nasal congestion. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Bousquet J, Khaltaev N, Cruz AA, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008;63 Suppl 86:8-160. doi:10.1111/j.1398-9995.2007.01620.x
- WONCA International Classification Committee. ICPC-2: International Classification of Primary Care. 2nd ed. Oxford: Oxford University Press; 1998.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems (ICD-10). 10th Revision. Geneva: World Health Organization; 2016.
- Eccles R. Mechanisms of the sneeze reflex. In: Baraniuk JN, Shusterman D, eds. Nonallergic Rhinitis. New York: Informa Healthcare; 2007:19-34.
- Naclerio RM, Bachert C, Baraniuk JN. Pathophysiology of nasal congestion. Int J Gen Med. 2010;3:47-57. Published 2010 Apr 8. doi:10.2147/ijgm.s8088
- Wheatley LM, Togias A. Clinical practice. Allergic rhinitis. N Engl J Med. 2015;372(5):456-463. doi:10.1056/NEJMcp1412282
- Heikkinen T, Järvinen A. The common cold. Lancet. 2003;361(9351):51-59. doi:10.1016/S0140-6736(03)12162-9
- Bernstein JA. Allergic and mixed rhinitis: Epidemiology and natural history. Allergy Asthma Proc. 2010;31(5):365-369. doi:10.2500/aap.2010.31.3380
- Bhattacharyya N. Nasal obstruction: diagnosis and management. Otolaryngol Clin North Am. 2009;42(2):195-205. doi:10.1016/j.otc.2009.01.008
- Wallace DV, Dykewicz MS, Bernstein DI, et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol. 2008;122(2 Suppl):S1-S84. doi:10.1016/j.jaci.2008.06.003
Related articles
Made in USA