Introduction
Lacerations or cuts are common injuries that involve a break or tear in the skin. They can occur due to various causes, such as accidents, falls, or sharp objects. Lacerations can range from minor cuts that only affect the superficial layers of the skin to deep wounds that may involve underlying tissues or organs. The aim of this guide is to provide a comprehensive overview of the diagnosis and management of lacerations/cuts.[1]
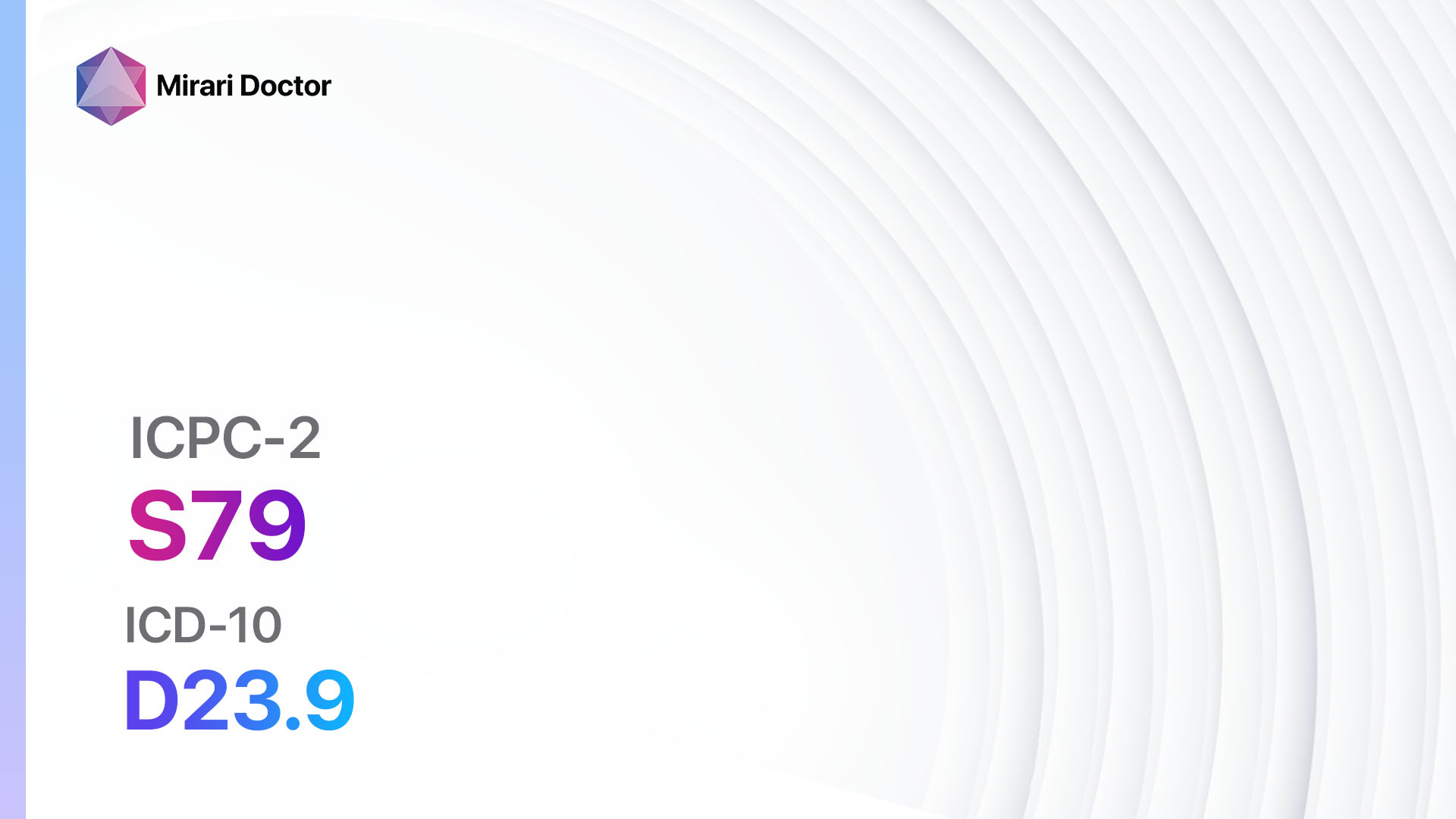
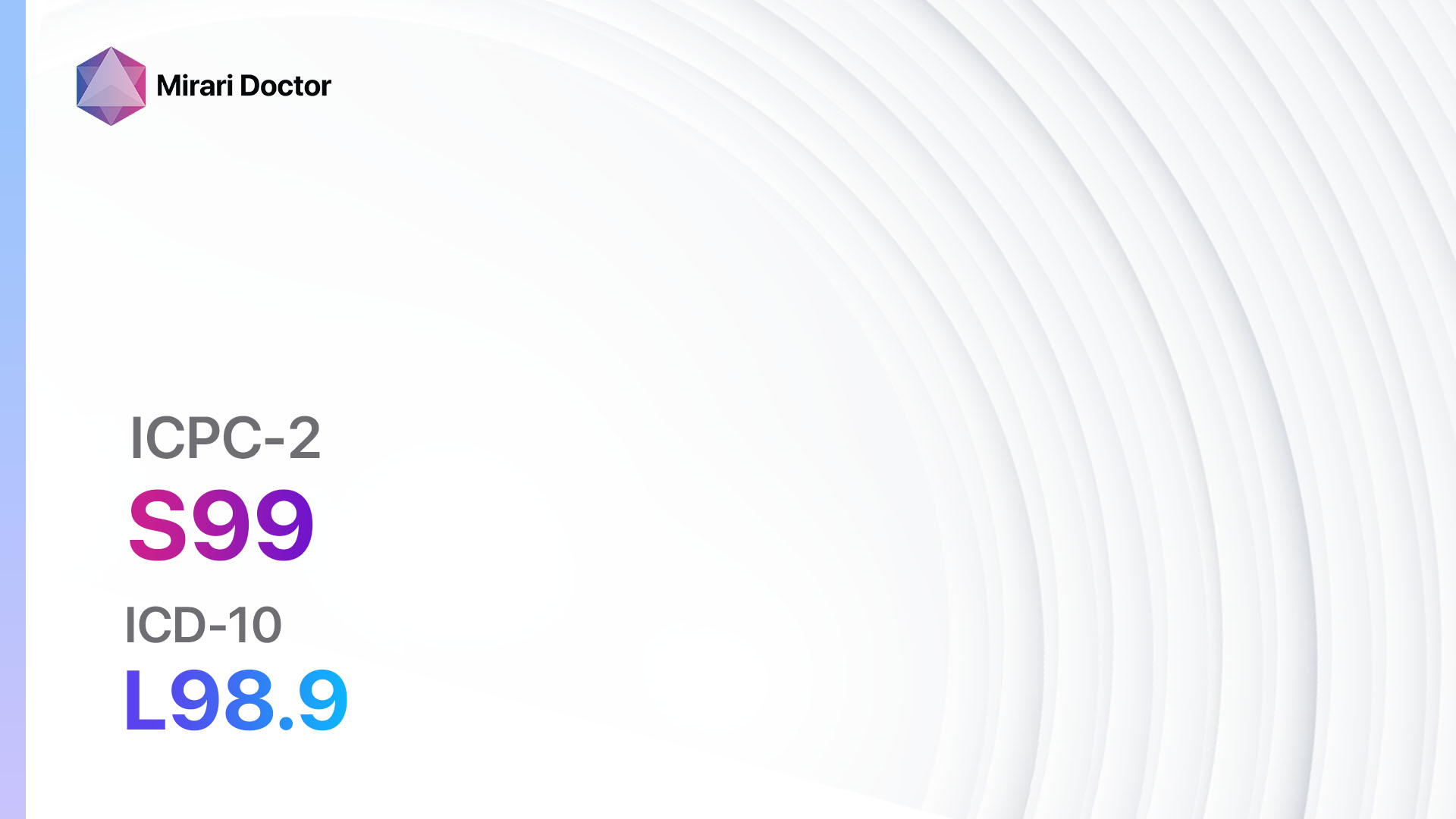
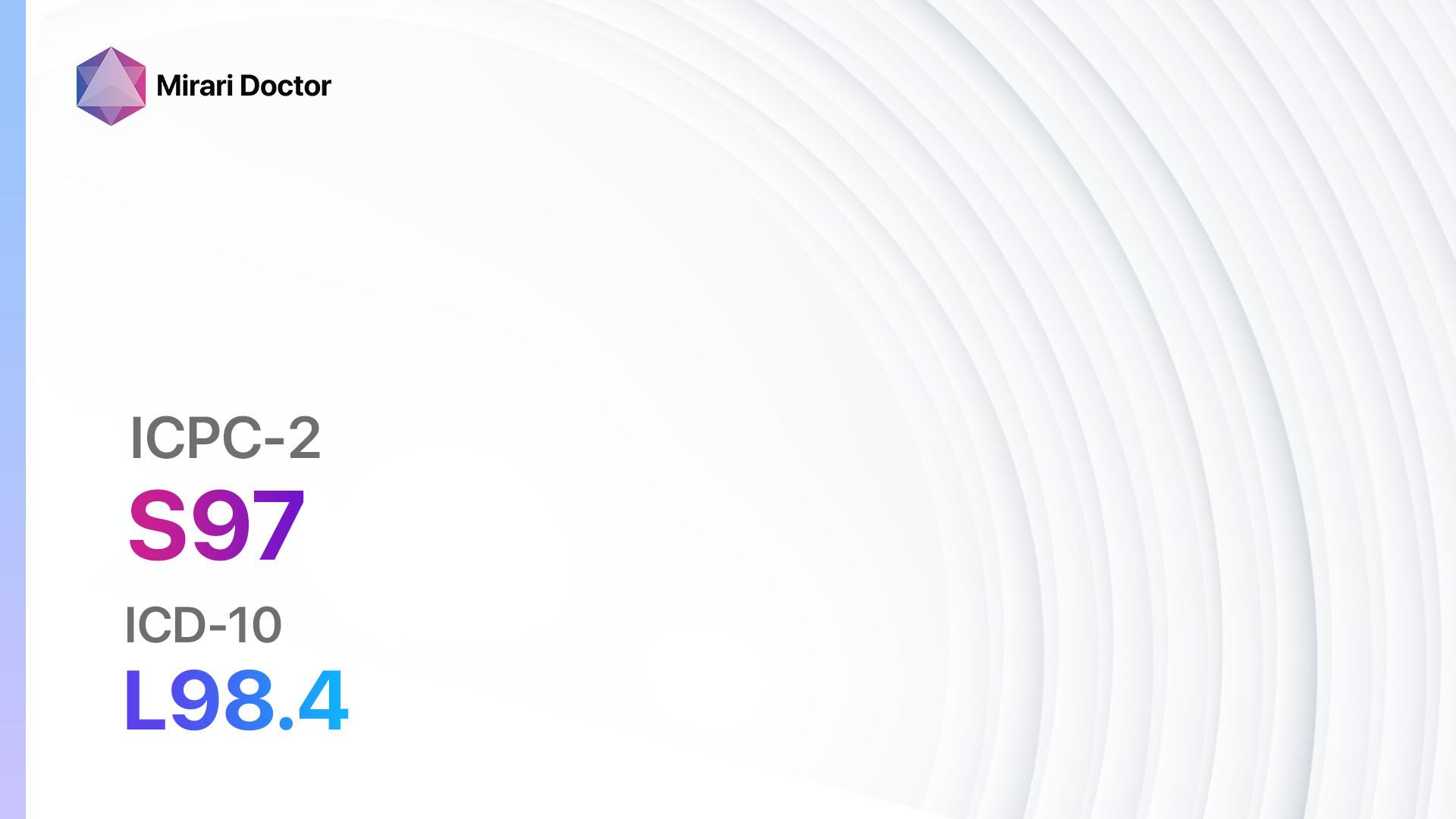
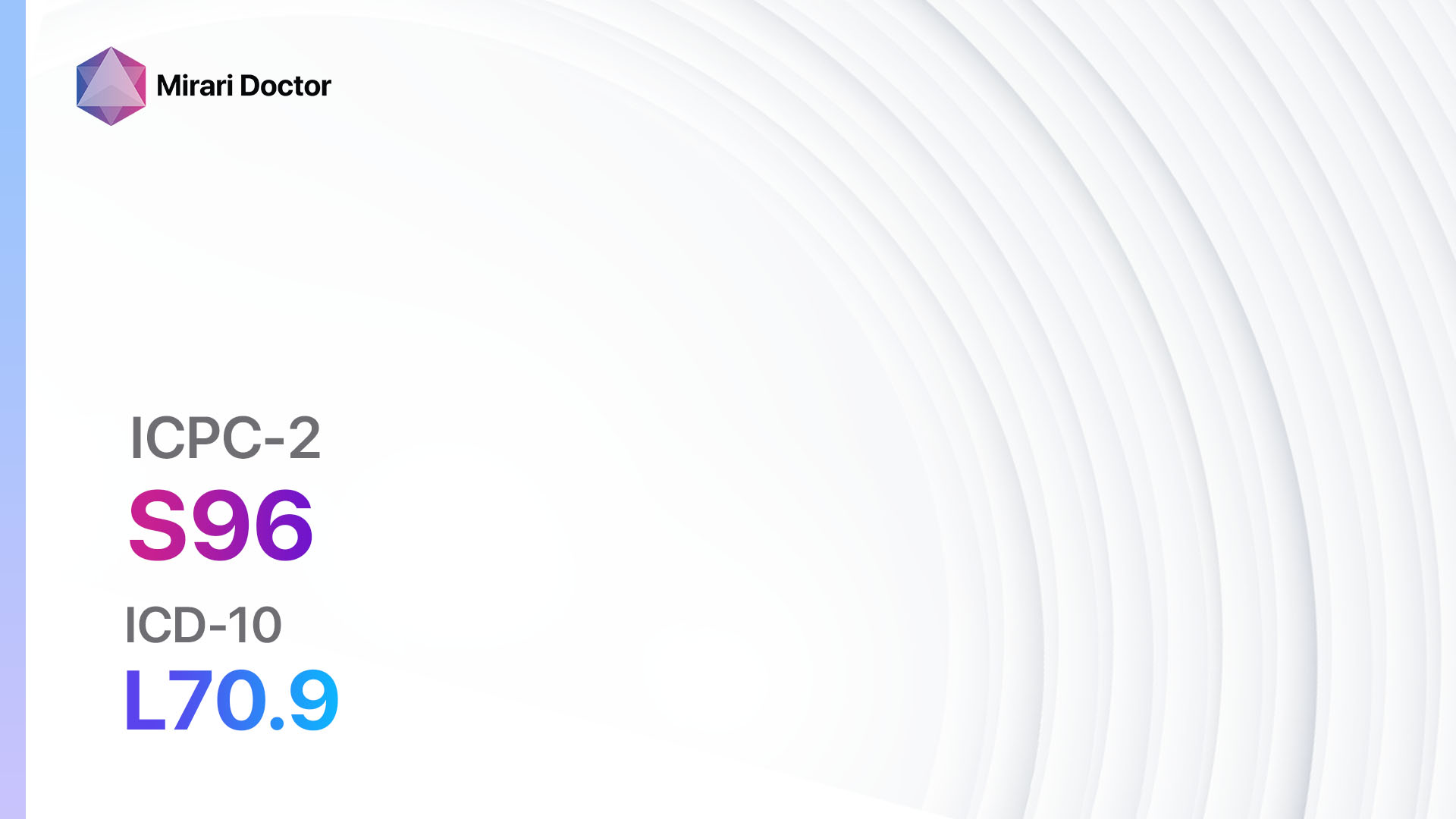
Codes
Symptoms
- Pain: Lacerations can cause localized pain at the site of the injury.[4]
- Bleeding: Depending on the severity of the laceration, there may be varying degrees of bleeding.[4]
- Swelling: Inflammation and swelling may occur around the laceration site.[4]
- Redness: The skin around the laceration may appear red or inflamed.[4]
- Impaired function: Deep or extensive lacerations may affect the normal functioning of the affected body part.[4]
Causes
- Accidents: Lacerations can occur as a result of accidents, such as falls, car crashes, or sports injuries.[5]
- Sharp objects: Contact with sharp objects, such as knives, broken glass, or metal edges, can cause lacerations.[5]
- Blunt force trauma: High-impact injuries, such as being hit by a heavy object, can lead to lacerations.[5]
Diagnostic Steps
Medical History
- Gather information about the circumstances surrounding the laceration, including the cause and mechanism of injury.[6]
- Assess the patient’s medical history, including any underlying medical conditions or medications that may affect wound healing.[6]
- Inquire about tetanus vaccination status, as lacerations can increase the risk of tetanus infection.[6]
Physical Examination
- Inspect the laceration site for the size, depth, and location of the wound.[7]
- Assess the extent of bleeding and the presence of any foreign objects in the wound.[7]
- Evaluate the surrounding tissues for signs of infection, such as redness, swelling, or pus.[7]
- Check for any damage to underlying structures, such as tendons, nerves, or blood vessels.[7]
Determine Severity
- Classify the laceration based on severity and depth:
- Superficial laceration: Involves only the outermost layer of the skin.[8]
- Partial-thickness laceration: Extends through the epidermis and into the dermis.[8]
- Full-thickness laceration: Involves all layers of the skin and may extend into underlying tissues or organs.[8]
Laboratory Tests
- Complete blood count (CBC): Assess for signs of infection or anemia.[9]
- Coagulation profile: Evaluate the patient’s clotting ability, especially if there is excessive bleeding.[9]
- Tetanus status: Check the patient’s immunization history and administer a tetanus booster if necessary.[9]
Diagnostic Imaging
- X-ray: Use X-rays to assess for the presence of any foreign objects, fractures, or damage to underlying bones.[10]
- Ultrasound: May be used to evaluate the depth and extent of the laceration, especially if there is concern for underlying organ injury.[10]
- CT scan: In cases of deep or complex lacerations, a CT scan may be necessary to assess for any internal injuries or bleeding.[10]
Other Tests
- Wound culture: Collect a sample from the laceration site for culture and sensitivity testing if there are signs of infection.
- Biopsy: In certain cases, a biopsy of the laceration site may be necessary to rule out any underlying malignancy or unusual pathology.
Follow-up and Patient Education
- Provide appropriate wound care instructions, including cleaning, dressing changes, and signs of infection.
- Schedule a follow-up appointment to monitor wound healing and remove any sutures or staples.
- Educate the patient about the importance of tetanus vaccination and the signs of tetanus infection.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for laceration/cut:
- Topical antibiotics (e.g., Neosporin, Bacitracin):
- Cost: $5-$10 for a tube.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Skin irritation or allergic reactions.
- Severe side effects: Rare, but may include severe allergic reactions.
- Drug interactions: None reported.
- Warning: Use only as directed and avoid prolonged use to prevent antibiotic resistance.
- Analgesics (e.g., Acetaminophen, Ibuprofen):
- Cost: $5-$10 for a bottle.
- Contraindications: Allergy to the medication, certain medical conditions (e.g., liver disease, bleeding disorders).
- Side effects: Upset stomach, dizziness.
- Severe side effects: Rare, but may include liver damage or gastrointestinal bleeding.
- Drug interactions: Other pain medications, blood thinners.
- Warning: Follow recommended dosages and avoid exceeding the maximum daily dose.
- Tetanus prophylaxis (e.g., Tetanus toxoid vaccine):
- Cost: $20-$50 for a vaccine dose.
- Contraindications: Severe allergic reaction to a previous dose of the vaccine.
- Side effects: Mild pain or swelling at the injection site.
- Severe side effects: Rare, but may include severe allergic reactions.
- Drug interactions: None reported.
- Warning: Ensure up-to-date tetanus vaccination status and administer booster doses as necessary.
- Systemic antibiotics (e.g., Amoxicillin, Cephalexin):
- Cost: $10-$50 for a course of treatment.
- Contraindications: Allergy to the medication, certain medical conditions (e.g., kidney disease, history of antibiotic-associated colitis).
- Side effects: Upset stomach, diarrhea.
- Severe side effects: Rare, but may include severe allergic reactions or antibiotic-associated colitis.
- Drug interactions: Other medications that may interact with antibiotics.
- Warning: Use only when necessary and as prescribed to prevent antibiotic resistance.
- Tissue adhesives (e.g., Dermabond, SurgiSeal):
- Cost: $20-$50 per vial.
- Contraindications: Deep or contaminated wounds, certain medical conditions (e.g., poor wound healing, compromised blood supply).
- Side effects: Skin irritation or allergic reactions.
- Severe side effects: Rare, but may include severe allergic reactions or poor wound healing.
- Drug interactions: None reported.
- Warning: Use only on appropriate wounds and follow manufacturer instructions for application.
Surgical Procedures:
- Suture closure: In cases of deep or extensive lacerations, sutures may be used to bring the wound edges together and promote healing. Cost: $100-$500.
- Staple closure: Staples may be used as an alternative to sutures for certain lacerations, especially in areas with high tension or hair-bearing regions. Cost: $100-$500.
- Wound debridement: In cases of contaminated or infected lacerations, surgical debridement may be necessary to remove necrotic tissue and promote wound healing. Cost: $500-$2000.
- Skin grafting: For large or complex lacerations, skin grafting may be required to cover the wound and facilitate healing. Cost: $2000-$10,000.
- Flap reconstruction: In cases where there is significant tissue loss or damage, flap reconstruction may be performed to replace the missing tissue and restore function. Cost: $5000-$20,000.
Alternative Interventions
- Acupuncture: May help reduce pain and promote healing. Cost: $60-$120 per session.
- Hyperbaric oxygen therapy: Involves breathing pure oxygen in a pressurized chamber to enhance wound healing. Cost: $200-$300 per session.
- Herbal remedies: Certain herbs, such as aloe vera or calendula, may have potential benefits for wound healing. Cost: Varies depending on the specific product.
- Homeopathy: Some homeopathic remedies, such as Arnica montana, may be used to reduce pain and inflammation. Cost: Varies depending on the specific remedy.
- Cold therapy: Applying cold packs or ice to the laceration site may help reduce pain and swelling. Cost: Varies depending on the availability of cold packs or ice.
Lifestyle Interventions
- Proper wound care: Clean the laceration with mild soap and water, apply an antibiotic ointment, and cover with a sterile dressing. Cost: Minimal.
- Healthy diet: Consuming a balanced diet rich in vitamins and minerals can promote wound healing. Cost: Varies depending on food choices.
- Adequate rest: Getting enough rest and sleep allows the body to heal more efficiently. Cost: None.
- Smoking cessation: Smoking can impair wound healing, so quitting smoking can improve healing outcomes. Cost: Varies depending on smoking cessation methods.
- Stress management: Stress can delay wound healing, so practicing stress management techniques, such as meditation or yoga, may be beneficial. Cost: Varies depending on the chosen stress management method.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – S18 Laceration/cut (ICD-10:T14.1)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD | Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD |
 |
|
Use the Mirari Cold Plasma device to treat Laceration/cut effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Laceration/cut. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Laceration – StatPearls – NCBI Bookshelf. (n.d.). Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK545166/
- ICPC-2 Codes – RxReasoner. (n.d.). Retrieved from https://www.rxreasoner.com/icpc2codes/component/T
- ICD-10 code: T14.1 Open wound of unspecified body region. (n.d.). Retrieved from https://gesund.bund.de/en/icd-code-search/t14-1
- Laceration – PubMed. (n.d.). Retrieved from https://pubmed.ncbi.nlm.nih.gov/31424750/
- Lacerations | Johns Hopkins Medicine. (n.d.). Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/lacerations
- Assessment and management of facial lacerations – UpToDate. (n.d.). Retrieved from https://www.uptodate.com/contents/assessment-and-management-of-facial-lacerations
- Facial Soft Tissue Injuries Clinical Presentation – Medscape Reference. (n.d.). Retrieved from https://emedicine.medscape.com/article/84727-clinical
- Clinical Practice Guidelines : Lacerations. (n.d.). Retrieved from https://www.rch.org.au/clinicalguide/guideline_index/lacerations/
- A Laceration that Needed a Proper Exam, Not an X-Ray. | PSNet. (n.d.). Retrieved from https://psnet.ahrq.gov/web-mm/laceration-needed-proper-exam-not-x-ray
- Flexor Tendon Lacerations Clinical Presentation. (n.d.). Retrieved from https://emedicine.medscape.com/article/1286303-clinical
Related articles
Made in USA