Introduction
Urticaria, also known as hives, is a common skin condition characterized by the appearance of raised, itchy welts on the skin[1]. It can be acute or chronic and may be caused by various factors such as allergies, infections, medications, or underlying medical conditions[2]. The aim of this guide is to provide a comprehensive overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for urticaria.
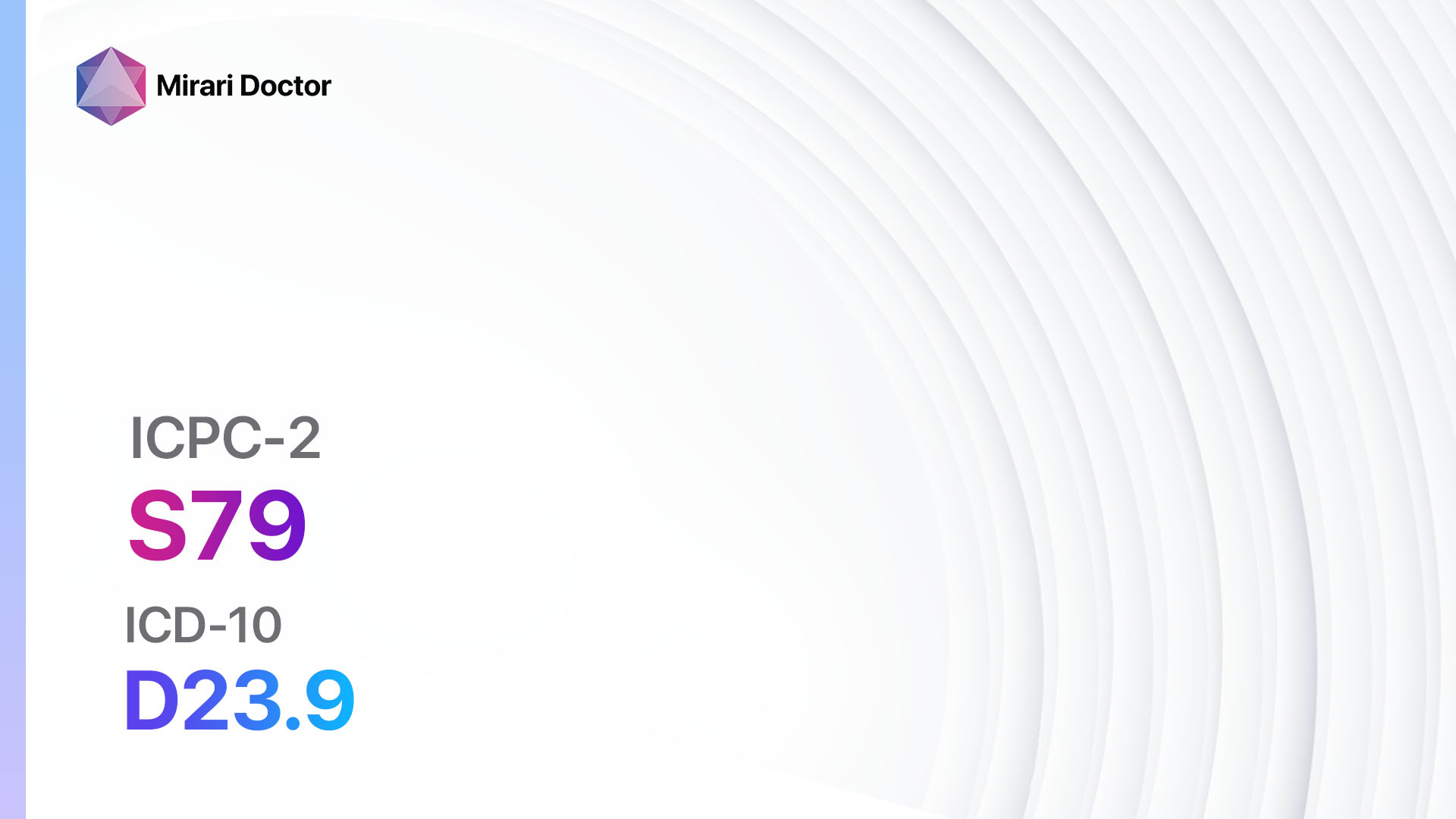
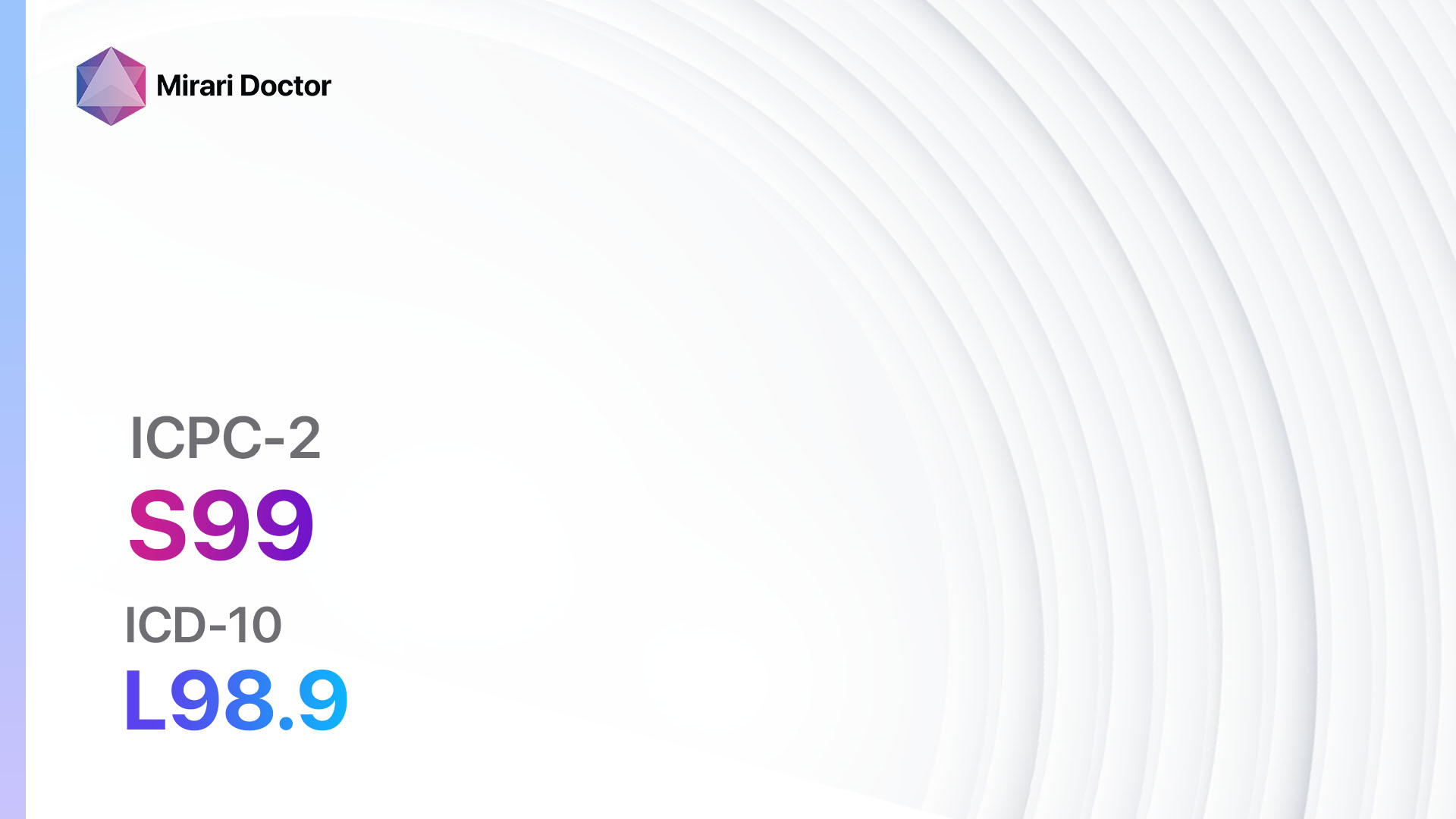
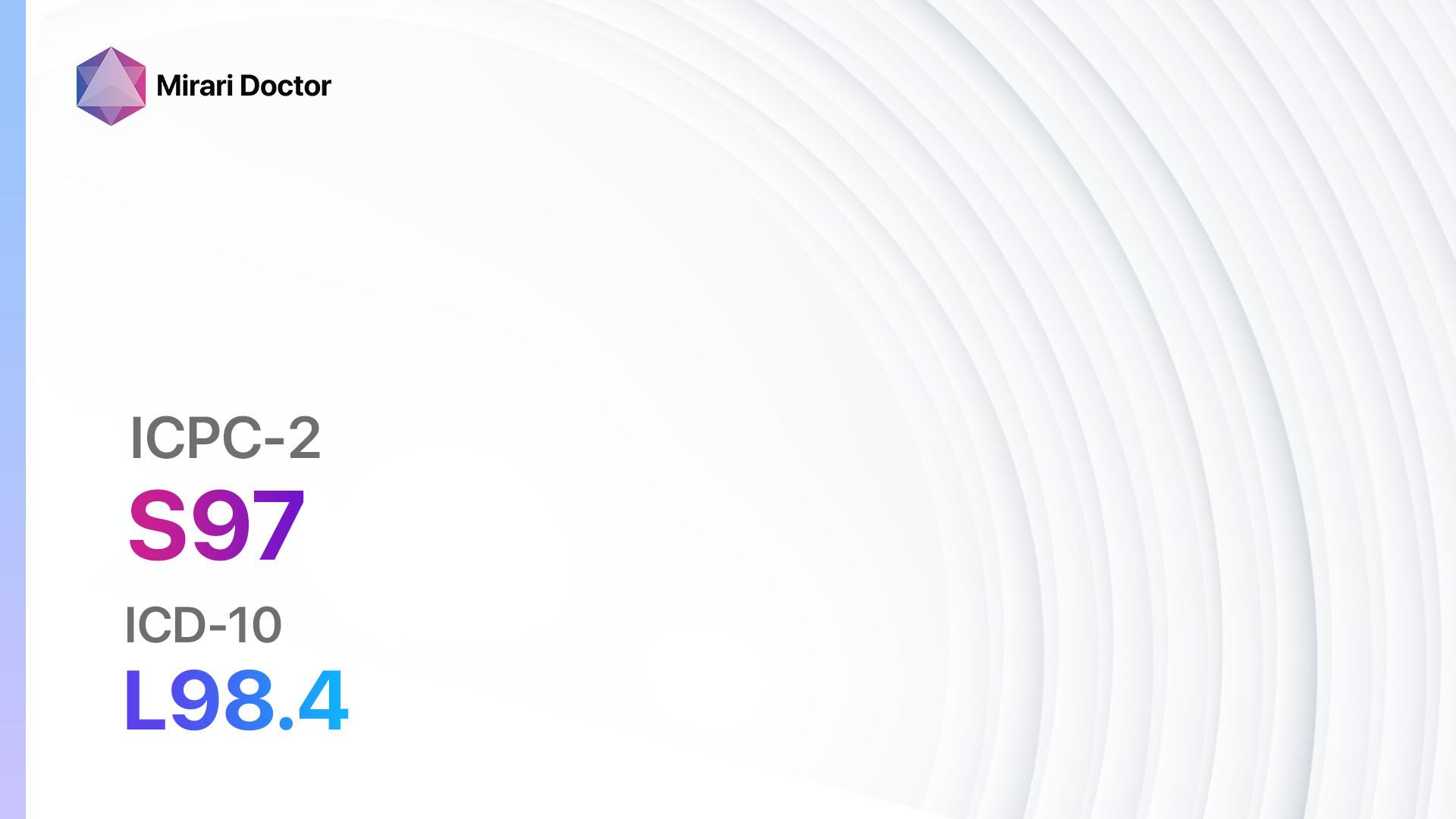
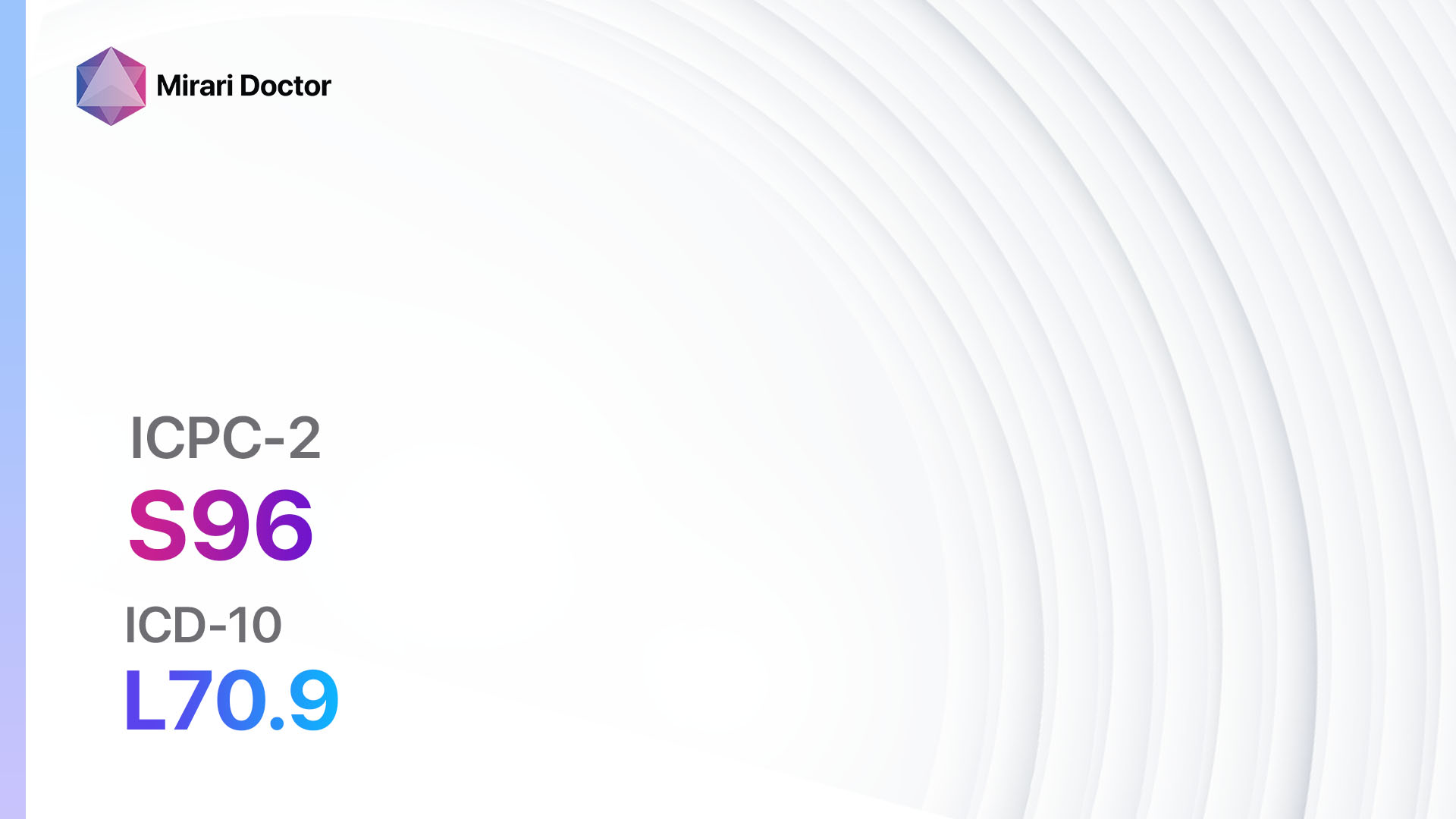
Codes
Symptoms
- Itchy, raised welts on the skin (hives)
- Red or pink skin rash
- Swelling of the affected area
- Burning or stinging sensation
- The rash may change shape, size, and location within a few hours[3]
Causes
- Allergic reactions to certain foods, medications, or insect bites
- Infections, such as viral or bacterial infections
- Physical triggers, such as pressure, heat, cold, or sunlight
- Underlying medical conditions, such as autoimmune disorders or thyroid disease
- Stress or emotional factors[4]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration, frequency, and triggers of the hives
- Identify any potential risk factors, such as a history of allergies or underlying medical conditions
- Ask about recent exposure to potential allergens or triggers
- Inquire about any recent changes in medications or lifestyle factors[5]
Physical Examination
- Perform a thorough examination of the skin to assess the appearance and distribution of the hives
- Look for any signs of swelling or other associated symptoms
- Check for any signs of underlying medical conditions or infections[6]
Determine Severity
- Classify the severity of urticaria based on the following criteria:
- Mild: Hives are localized and do not cause significant discomfort or interference with daily activities.
- Moderate: Hives are more widespread and may cause moderate itching or discomfort.
- Severe: Hives are extensive, causing severe itching, swelling, and significant interference with daily activities[7].
Laboratory Tests
- Complete blood count (CBC) to assess for any underlying infections or abnormalities
- Allergy testing to identify potential allergens that may be triggering the hives
- Thyroid function tests to rule out any underlying thyroid disorders
- Erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) to assess for any signs of inflammation[8]
Diagnostic Imaging
- No diagnostic imaging is typically necessary for the diagnosis of urticaria.
Other Tests
- Skin biopsy may be performed in certain cases to rule out other skin conditions or to assess for any underlying autoimmune disorders[9].
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the progress of the hives and adjust treatment if necessary.
- Educate the patient about potential triggers and how to avoid them.
- Provide information on self-care measures, such as avoiding hot showers, wearing loose-fitting clothing, and using cool compresses to relieve itching[10].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Urticaria:
- Antihistamines (e.g., Cetirizine, Loratadine, Fexofenadine):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: Hypersensitivity to antihistamines.
- Side effects: Drowsiness, dry mouth, dizziness.
- Severe side effects: Rare, but may include severe allergic reactions.
- Drug interactions: Sedatives, alcohol.
- Warning: May cause drowsiness, avoid driving or operating heavy machinery.
- Corticosteroids (e.g., Prednisone, Methylprednisolone):
- Cost: Generic versions can be $4-$30/month.
- Contraindications: Active infections, systemic fungal infections.
- Side effects: Increased appetite, weight gain, mood changes.
- Severe side effects: Increased risk of infections, osteoporosis.
- Drug interactions: Nonsteroidal anti-inflammatory drugs (NSAIDs), anticoagulants.
- Warning: Long-term use may require gradual tapering to avoid adrenal insufficiency.
- Leukotriene receptor antagonists (e.g., Montelukast):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to leukotriene receptor antagonists.
- Side effects: Headache, gastrointestinal disturbances.
- Severe side effects: Rare, but may include psychiatric reactions.
- Drug interactions: None reported.
- Warning: Monitor for any signs of psychiatric reactions, especially in children.
- Immunosuppressants (e.g., Cyclosporine, Azathioprine):
- Cost: Generic versions can be $50-$200/month.
- Contraindications: Active infections, malignancies.
- Side effects: Increased risk of infections, gastrointestinal disturbances.
- Severe side effects: Increased risk of malignancies, kidney damage.
- Drug interactions: Other immunosuppressants, certain antibiotics.
- Warning: Regular monitoring of blood counts and kidney function is required.
- Omalizumab (anti-IgE monoclonal antibody):
- Cost: Approximately $1,000-$2,000 per month.
- Contraindications: None reported.
- Side effects: Injection site reactions, headache, fatigue.
- Severe side effects: Rare, but may include severe allergic reactions.
- Drug interactions: None reported.
- Warning: Requires subcutaneous injection by a healthcare professional.
Alternative Drugs:
- Dapsone: May be used in refractory cases of chronic urticaria.
- Cyclosporine: An alternative immunosuppressant for severe chronic urticaria.
- Methotrexate: May be considered in severe cases of chronic urticaria.
- Colchicine: May be used in patients with urticarial vasculitis.
- Rituximab: An option for refractory cases of chronic urticaria.
Surgical Procedures:
- No surgical procedures are typically necessary for the treatment of urticaria.
Alternative Interventions
- Acupuncture: May help alleviate symptoms of urticaria and reduce itching. Cost: $60-$120 per session.
- Herbal supplements: Certain herbs, such as stinging nettle or chamomile, may have anti-inflammatory properties and provide relief from itching. Cost: Varies depending on the specific supplement.
- Probiotics: Some studies suggest that probiotics may help improve symptoms of urticaria by modulating the immune system. Cost: Varies depending on the specific probiotic supplement.
- Relaxation techniques: Stress and anxiety can worsen symptoms of urticaria, so relaxation techniques such as deep breathing exercises or meditation may be beneficial. Cost: Free.
- Avoidance of triggers: Identifying and avoiding triggers, such as certain foods or environmental factors, can help prevent or minimize episodes of urticaria. Cost: Varies depending on individual circumstances.
Lifestyle Interventions
- Avoidance of known triggers: Educate the patient about common triggers and advise them to avoid exposure to these triggers.
- Cool compresses: Apply cool compresses to the affected areas to reduce itching and inflammation. Cost: Free.
- Loose-fitting clothing: Advise the patient to wear loose-fitting clothing made of breathable fabrics to minimize irritation. Cost: Varies depending on individual preferences.
- Moisturizers: Recommend the use of fragrance-free moisturizers to keep the skin hydrated and prevent dryness. Cost: Varies depending on the specific product.
- Stress management: Encourage the patient to engage in stress-reducing activities, such as exercise, yoga, or meditation. Cost: Varies depending on individual preferences.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – S98 Urticaria (ICD-10:L50.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Urticaria effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Urticaria. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Zuberbier, T., Aberer, W., Asero, R., Abdul Latiff, A. H., Baker, D., Ballmer-Weber, B., … & Maurer, M. (2018). The EAACI/GA²LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy, 73(7), 1393-1414.
- Schaefer, P. (2017). Acute and chronic urticaria: evaluation and treatment. American family physician, 95(11), 717-724.
- Bernstein, J. A., Lang, D. M., Khan, D. A., Craig, T., Dreyfus, D., Hsieh, F., … & Wallace, D. (2014). The diagnosis and management of acute and chronic urticaria: 2014 update. Journal of Allergy and Clinical Immunology, 133(5), 1270-1277.
- Kaplan, A. P. (2004). Chronic urticaria: pathogenesis and treatment. Journal of Allergy and Clinical Immunology, 114(3), 465-474.
- Maurer, M., Weller, K., Bindslev-Jensen, C., Giménez-Arnau, A., Bousquet, P. J., Bousquet, J., … & Zuberbier, T. (2011). Unmet clinical needs in chronic spontaneous urticaria. A GA²LEN task force report. Allergy, 66(3), 317-330.
- Saini, S. S. (2014). Chronic spontaneous urticaria: etiology and pathogenesis. Immunology and Allergy Clinics, 34(1), 33-52.
- Zuberbier, T., Balke, M., Worm, M., Edenharter, G., & Maurer, M. (2010). Epidemiology of urticaria: a representative cross-sectional population survey. Clinical and experimental dermatology, 35(8), 869-873.
- Kolkhir, P., Church, M. K., Weller, K., Metz, M., Schmetzer, O., & Maurer, M. (2017). Autoimmune chronic spontaneous urticaria: What we know and what we do not know. Journal of Allergy and Clinical Immunology, 139(6), 1772-1781.
- Amin, P., & Levin, L. (2015). The role of skin biopsy in the diagnosis of chronic urticaria. Current Allergy and Asthma Reports, 15(1), 1-5.
- Sharma, M., Bennett, C., Cohen, S. N., & Carter, B. (2014). H1-antihistamines for chronic spontaneous urticaria. Cochrane Database of Systematic Reviews, (11).
Related articles
Made in USA