Introduction
Abrasion, scratch, and blister are common skin injuries that can occur due to various causes. These injuries can cause discomfort, pain, and potential complications if not properly managed. The aim of this guide is to provide healthcare professionals with a comprehensive clinical procedural guide for the diagnosis and management of abrasion/scratch/blister[1].
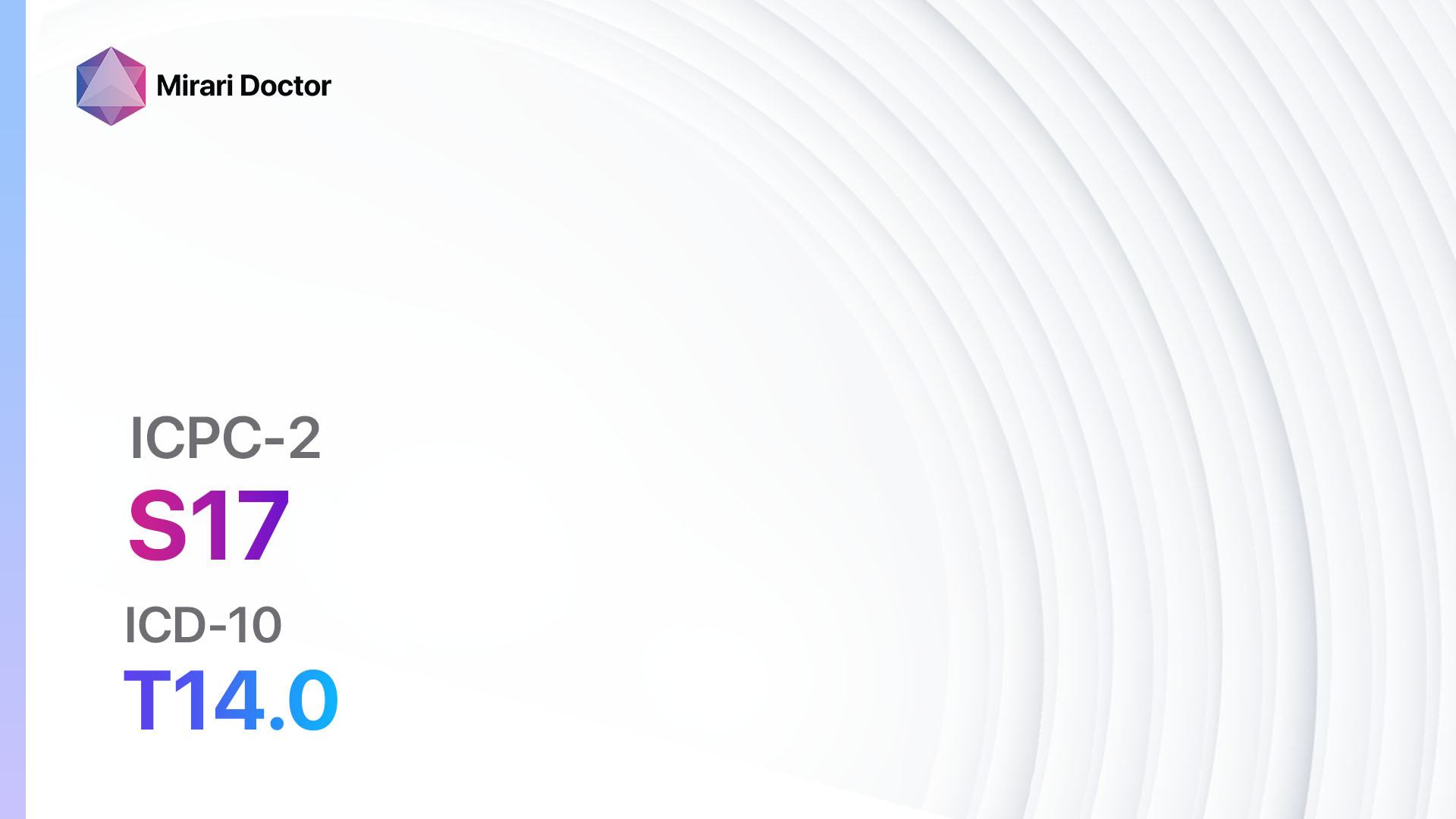
Codes
- ICPC-2 Code: S17 Abrasion/scratch/blister[2]
- ICD-10 Code: T14.0 Superficial injury of unspecified body region[3]
Symptoms
- Abrasion: Superficial skin injury characterized by the removal of the top layer of skin, resulting in a raw and painful area.[4]
- Scratch: A shallow mark or wound on the skin caused by the act of scratching.[5]
- Blister: A raised area on the skin filled with fluid, resulting from friction, burns, or other injuries.[6]
Causes
- Abrasion: Friction, falls, scrapes, or contact with rough surfaces.[7]
- Scratch: Itching, insect bites, skin conditions (e.g., eczema), or self-inflicted.[8]
- Blister: Friction, burns, allergic reactions, or infections.[9]
Diagnostic Steps
Medical History
- Gather information about the patient’s recent activities, including any incidents or exposure to potential causes of abrasion/scratch//blister.[10]
- Identify any underlying medical conditions or medications that may affect wound healing or increase the risk of infection.
- Assess the patient’s pain level and any associated symptoms, such as itching or redness.
Physical Examination
- Inspect the affected area for signs of abrasion, scratch, or blister, including redness, swelling, or fluid-filled lesions.
- Assess the size, depth, and location of the wound.
- Evaluate the surrounding skin for signs of infection, such as warmth, tenderness, or pus.
Determine Severity
- Classify the abrasion/scratch/blister based on severity and depth:
- Superficial abrasion: Involves only the top layer of skin.
- Partial-thickness abrasion: Involves the top layer and part of the underlying layer of skin.
- Full-thickness abrasion: Involves the entire thickness of the skin, including the underlying tissues.
- Superficial scratch: Shallow mark on the skin without significant tissue damage.
- Deep scratch: Extends beyond the superficial layers of the skin, potentially causing bleeding or scarring.
- Superficial blister: Fluid-filled lesion confined to the top layer of skin.
- Deep blister: Involves the deeper layers of the skin, potentially causing pain and increased risk of infection.
Laboratory Tests
- In most cases, laboratory tests are not necessary for the diagnosis of abrasion/scratch/blister.
- However, if there are signs of infection or the wound is not healing properly, a wound culture may be performed to identify the causative organism and guide appropriate treatment.
Diagnostic Imaging
- Diagnostic imaging is typically not necessary for the diagnosis of abrasion/scratch/blister.
- However, in cases of suspected underlying fractures or foreign bodies, X-rays may be performed to rule out associated injuries.
Other Tests
- Other diagnostic tests may not be necessary for the diagnosis of abrasion/scratch/blister.
- However, if there is a suspicion of an underlying medical condition contributing to the skin injury, further investigations may be required, such as blood tests or skin biopsies.
Follow-up and Patient Education
- Advise the patient on proper wound care, including cleaning the wound with mild soap and water, applying a sterile dressing, and keeping the wound clean and dry.
- Educate the patient on signs of infection, such as increased pain, redness, swelling, or pus, and instruct them to seek medical attention if these symptoms occur.
- Schedule a follow-up appointment to monitor wound healing and address any concerns or complications.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Abrasion/scratch/blister:
- Topical antibiotics (e.g., Neosporin, Polysporin):
- Cost: $5-$15 per tube.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Rare, but may include skin irritation or allergic reactions.
- Severe side effects: Uncommon, but may include severe allergic reactions.
- Drug interactions: None reported.
- Warning: Use only as directed and avoid prolonged use.
- Topical antiseptics (e.g., Betadine, hydrogen peroxide):
- Cost: $5-$15 per bottle.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Rare, but may include skin irritation or allergic reactions.
- Severe side effects: Uncommon, but may include severe allergic reactions.
- Drug interactions: None reported.
- Warning: Use only as directed and avoid contact with eyes or mucous membranes.
- Topical analgesics (e.g., lidocaine, benzocaine):
- Cost: $5-$20 per tube.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Rare, but may include skin irritation or allergic reactions.
- Severe side effects: Uncommon, but may include severe allergic reactions.
- Drug interactions: None reported.
- Warning: Use only as directed and avoid application on open wounds or broken skin.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., ibuprofen, naproxen):
- Cost: $5-$20 per bottle.
- Contraindications: History of NSAID allergy or gastrointestinal bleeding.
- Side effects: Upset stomach, heartburn, or increased risk of bleeding.
- Severe side effects: Rare, but may include severe allergic reactions or kidney problems.
- Drug interactions: Avoid concomitant use with other NSAIDs or blood thinners.
- Warning: Take with food to minimize stomach upset and follow the recommended dosage.
- Tetanus prophylaxis (e.g., tetanus toxoid vaccine):
- Cost: $20-$50 per dose.
- Contraindications: Severe allergic reaction to a previous dose or any component of the vaccine.
- Side effects: Mild pain or swelling at the injection site.
- Severe side effects: Rare, but may include severe allergic reactions.
- Drug interactions: None reported.
- Warning: Ensure up-to-date tetanus vaccination status and administer booster doses as recommended.
Alternative Drugs:
- Topical corticosteroids (e.g., hydrocortisone): May help reduce inflammation and itching.
- Oral analgesics (e.g., acetaminophen): For pain relief if topical analgesics are not sufficient.
- Antihistamines (e.g., diphenhydramine): For relief of itching associated with allergic reactions.
- Systemic antibiotics (e.g., amoxicillin, cephalexin): If there is a risk of infection or signs of spreading cellulitis.
- Tetanus immunoglobulin (TIG): For individuals who are not adequately immunized against tetanus and have a high-risk wound.
Surgical Procedures:
- Surgical procedures are typically not necessary for the management of abrasion/scratch/blister.
- However, in cases of severe or infected wounds, surgical debridement or drainage may be required.
Alternative Interventions
- Aloe vera gel: May help soothe and promote wound healing. Cost: $5-$20 per bottle.
- Honey: Has antimicrobial properties and may aid in wound healing. Cost: $10-$20 per jar.
- Hydrocolloid dressings: Provide a moist environment for wound healing. Cost: $10-$30 per box.
- Wound healing ointments: Contain ingredients such as vitamin E or zinc oxide to promote healing. Cost: $5-$20 per tube.
- Cold compress: Helps reduce pain, swelling, and inflammation. Cost: $5-$10 per pack.
Lifestyle Interventions
- Proper wound care: Clean the wound with mild soap and water, apply a sterile dressing, and keep the wound clean and dry. Cost: Minimal.
- Avoid scratching or picking at the wound: Minimize the risk of infection and promote healing. Cost: None.
- Protective clothing or equipment: Use appropriate protective gear to prevent skin injuries during activities. Cost: Varies depending on the specific gear.
- Moisturize the skin: Keep the skin hydrated to prevent dryness and cracking. Cost: $5-$20 per bottle of moisturizer.
- Avoid exposure to irritants: Minimize contact with substances that may cause skin irritation or allergic reactions. Cost: None.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – S17 Abrasion/scratch/blister (ICD-10:T14.0)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 30 minutes approx. $5 USD, Evening: 30 minutes approx. $5 USD |
Total Morning: 60 minutes approx. $10 USD, Lunch: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD, |
Total Morning: 60 minutes approx. $10 USD, Lunch: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD, |
| Usual treatment for 7-60 days approx. $70 USD – $600 USD | Usual treatment for 6-8 weeks approx. $1,260 USD – $1,680 USD |
Usual treatment for 3-6 months approx. $2,700 USD – $5,400 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Abrasion/scratch/blister effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Abrasion/scratch/blister. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Abrasion, scratch, and blister. (n.d.). Retrieved from https://www.health.com/abrasions-8385913
- ICPC-2 Code: S17 Abrasion/scratch/blister. (n.d.). Retrieved from https://www.healthline.com/health/abrasion
- ICD-10 Code: T14.0 Superficial injury of unspecified body region. (n.d.). Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554465/
- Abrasion. (n.d.). Retrieved from https://www.healthline.com/health/abrasion
- Scratch. (n.d.). Retrieved from https://www.healthline.com/health/cuts-scratches
- Blister. (n.d.). Retrieved from https://www.health.com/condition/skin-conditions/friction-blister
- Causes of abrasion. (n.d.). Retrieved from https://www.healthline.com/health/abrasion
- Causes of scratch. (n.d.). Retrieved from https://www.healthline.com/health/cuts-scratches
- Causes of blister. (n.d.). Retrieved from https://www.health.com/condition/skin-conditions/friction-blister
- Medical history. (n.d.). Retrieved from https://www.seattlechildrens.org/conditions/a-z/skin-injury/
Related articles
Made in USA