Introduction
Warts, also known as verrucae, are common skin growths caused by the human papillomavirus (HPV). They are typically non-cancerous and can appear on various parts of the body, including the hands, feet, face, and genitals. Warts can be unsightly and may cause discomfort or pain, especially if they are located in areas that are frequently irritated or subjected to pressure.[1] The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of warts.
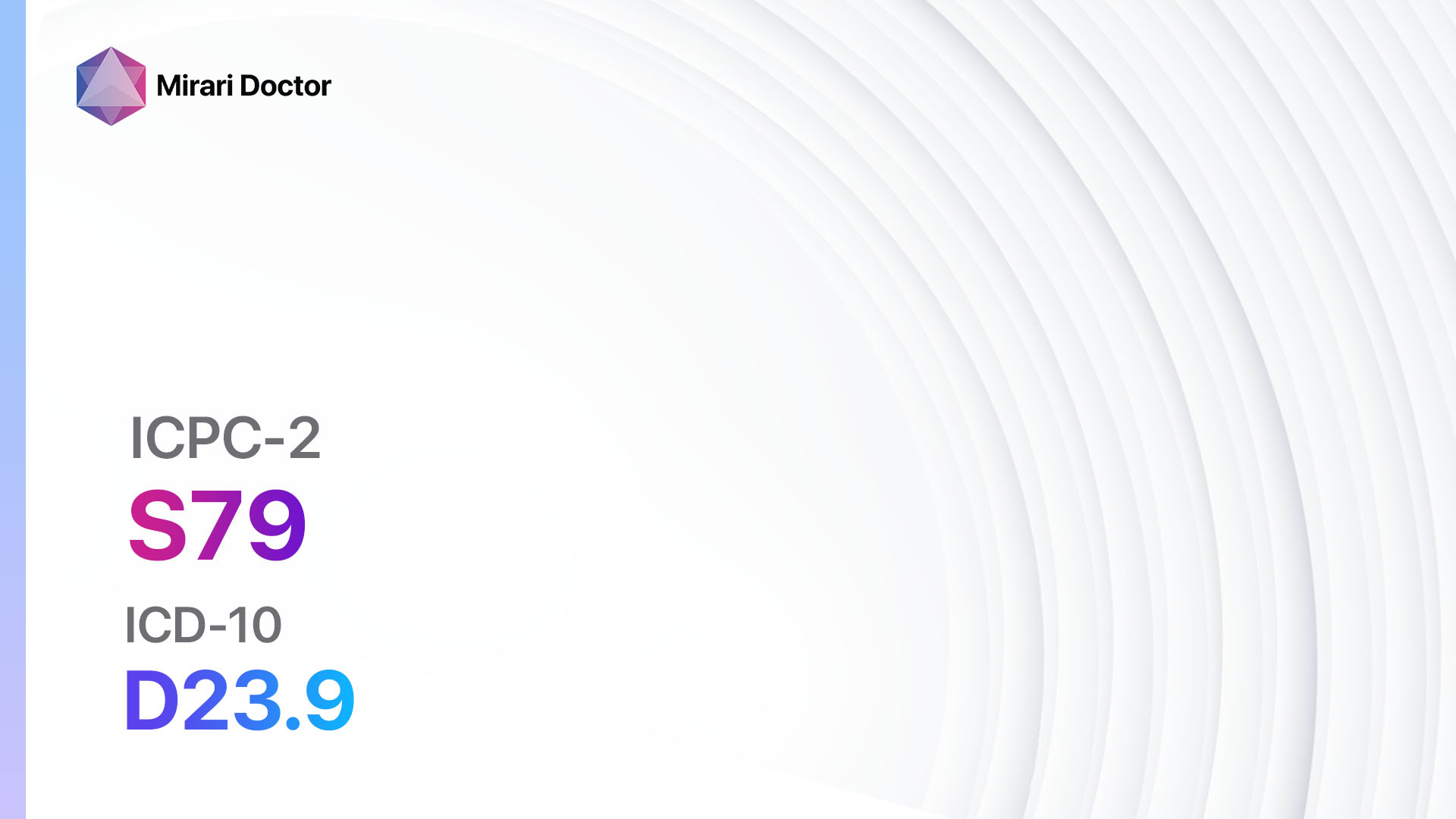
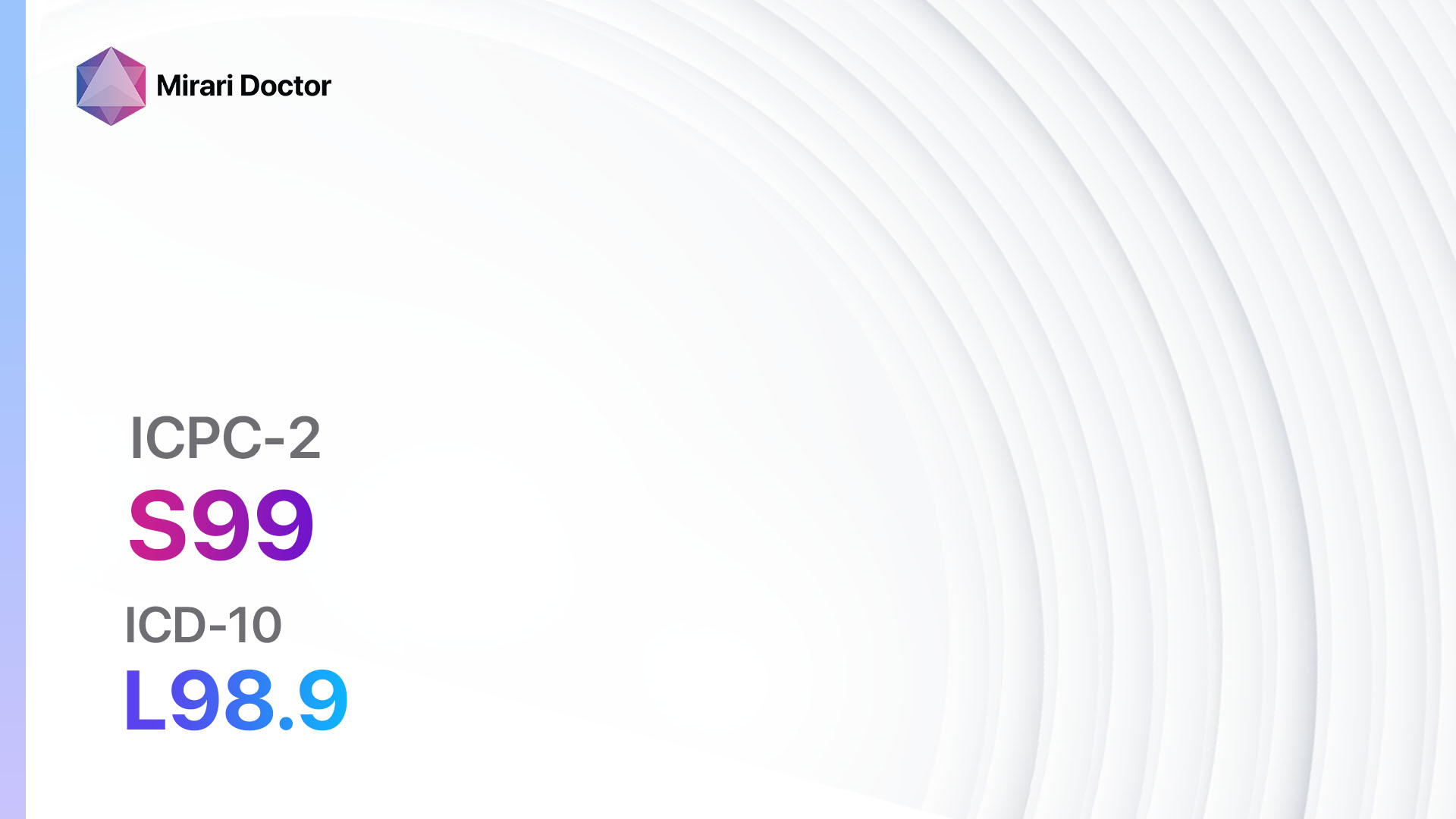
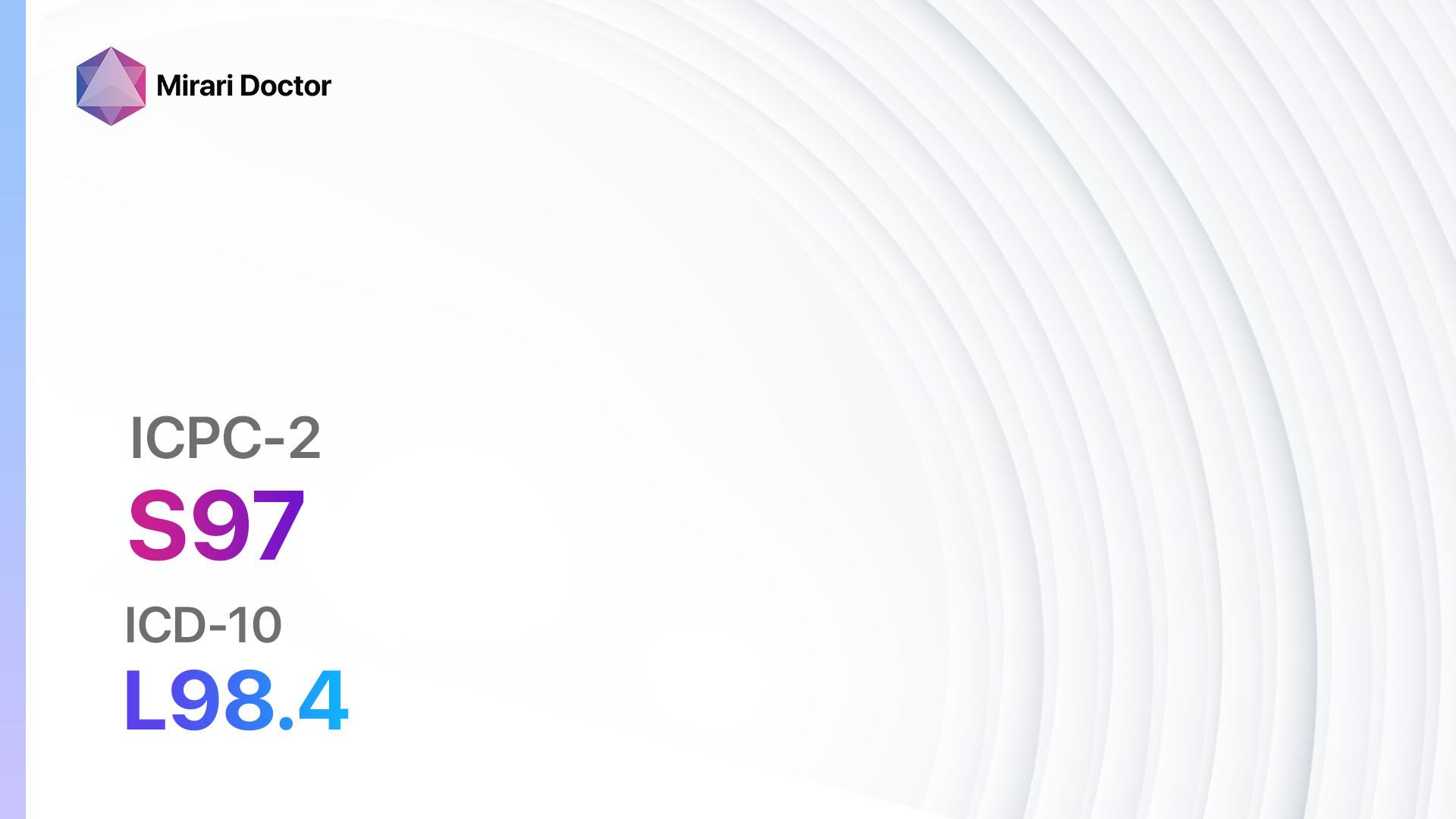
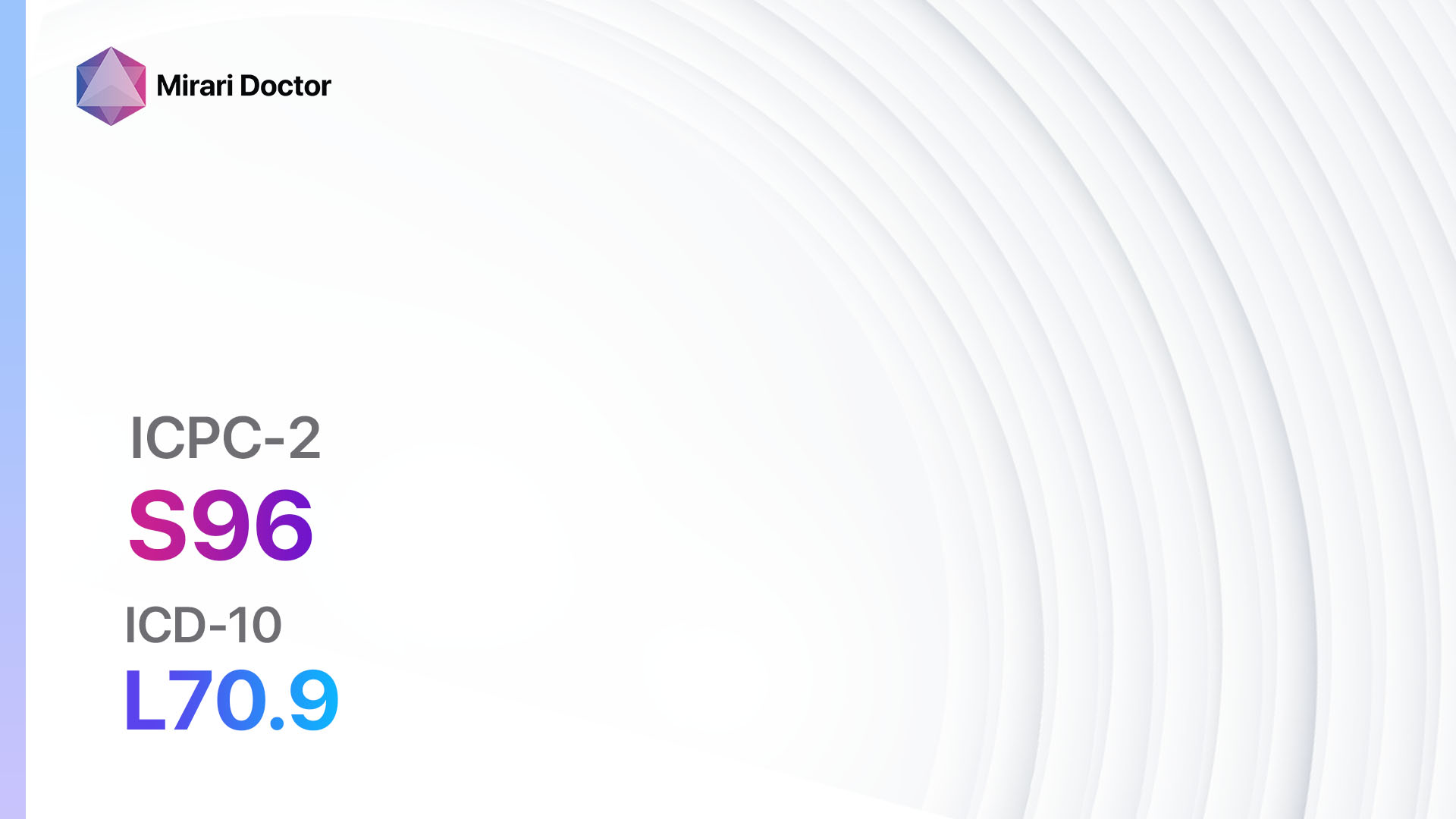
Codes
Symptoms
- Raised, rough, or bumpy growths on the skin
- Flesh-colored, white, pink, or tan in appearance
- Small, grainy, or cauliflower-like texture
- May have black dots (clotted blood vessels) in the center
- Itching or tenderness in the affected area
- Pain or discomfort when pressure is applied[3]
Causes
- Human papillomavirus (HPV) infection
- Direct contact with an infected person or contaminated surfaces
- Weakened immune system
- Skin-to-skin contact during sexual activity (genital warts)[4]
Diagnostic Steps
Medical History
- Inquire about the duration and progression of the warts
- Assess the patient’s overall health and immune status
- Determine if the patient has any underlying medical conditions or risk factors for HPV infection
- Ask about any previous treatments or interventions for warts[5]
Physical Examination
- Inspect the affected area for the presence of warts
- Note the size, shape, and location of the warts
- Observe the texture and color of the warts
- Assess for any signs of infection or inflammation
- Palpate the warts to evaluate tenderness or pain[6]
Determine Severity
- Classify the warts based on their severity and depth:
- Common warts (verruca vulgaris): Raised, rough, and typically found on the hands, fingers, or knees.
- Plantar warts: Located on the soles of the feet, often painful due to pressure.
- Flat warts (verruca plana): Small, smooth, and flat-topped warts commonly found on the face, neck, or legs.
- Genital warts (condyloma acuminatum): Located on or around the genitals or anus, sexually transmitted.[7]
Laboratory Tests
- No specific laboratory tests are required for the diagnosis of warts.
- In some cases, a skin biopsy may be performed to rule out other skin conditions or to confirm the diagnosis.[8]
Diagnostic Imaging
- No diagnostic imaging is necessary for the diagnosis of warts.
Other Tests
- No other specific tests are necessary for the diagnosis of warts[9].
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the progress of treatment and assess for recurrence.
- Educate the patient about the nature of warts, transmission, and prevention strategies.
- Provide information on self-care measures and when to seek medical attention[10].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Warts:
- Salicylic acid:
- Cost: Over-the-counter preparations range from $5 to $20.
- Contraindications: Allergy to salicylates, diabetes, poor circulation, or neuropathy.
- Side effects: Skin irritation, redness, or peeling.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Avoid use on the face or genitals.
- Cryotherapy (liquid nitrogen):
- Cost: $100 to $500 per session.
- Contraindications: Cold sensitivity, Raynaud’s disease, or cryoglobulinemia.
- Side effects: Pain, blistering, or hypopigmentation.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Multiple sessions may be required for complete clearance.
- Cantharidin:
- Cost: $100 to $500 per session.
- Contraindications: Allergy to cantharidin or other blistering agents, pregnancy, or breastfeeding.
- Side effects: Pain, blistering, or erythema.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Application should be done by a healthcare professional.
- Imiquimod:
- Cost: $100 to $500 per session.
- Contraindications: Allergy to imiquimod or other immune response modifiers.
- Side effects: Local skin reactions, such as redness, itching, or burning.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Apply a thin layer to the affected area before bedtime and wash off after 6-10 hours.
- Podophyllin resin:
- Cost: $100 to $500 per session.
- Contraindications: Pregnancy, breastfeeding, or allergy to podophyllin.
- Side effects: Skin irritation, redness, or ulceration.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Application should be done by a healthcare professional.
Alternative Drugs:
- Dinitrochlorobenzene (DNCB): Stimulates an immune response against the wart.
- Bleomycin: Injected directly into the wart to destroy the abnormal cells.
- 5-fluorouracil (5-FU): Inhibits the growth of abnormal cells in the wart.
- Interferon: Stimulates the immune system to fight against the HPV infection.
- Trichloroacetic acid (TCA): Causes controlled chemical burns to destroy the wart tissue.
Surgical Procedures:
- Electrosurgery: Uses an electric current to burn or cut off the wart.
- Cauterization: Uses heat to destroy the wart tissue.
- Excision: Surgically removes the wart and surrounding tissue.
- Laser surgery: Uses a laser beam to destroy the wart tissue.
Alternative Interventions
- Duct tape occlusion: Covering the wart with duct tape to suffocate the virus. Cost: $5-$10 for a roll of duct tape.
- Apple cider vinegar: Applying apple cider vinegar to the wart to promote its removal. Cost: $5-$10 for a bottle of apple cider vinegar.
- Tea tree oil: Applying tea tree oil to the wart to inhibit viral growth. Cost: $5-$10 for a bottle of tea tree oil.
- Garlic: Applying crushed garlic to the wart to stimulate the immune system. Cost: $2-$5 for a bulb of garlic.
- Aloe vera: Applying aloe vera gel to the wart to soothe and promote healing. Cost: $5-$10 for a bottle of aloe vera gel.
Lifestyle Interventions
- Good hygiene practices: Regular handwashing and avoiding touching or scratching the warts can help prevent the spread of the virus. Cost: Minimal.
- Avoidance of sharing personal items: Not sharing towels, socks, shoes, or other personal items can reduce the risk of transmission. Cost: Minimal.
- Avoidance of barefoot walking: Wearing shoes or sandals in public areas, especially around swimming pools or locker rooms, can reduce the risk of contracting plantar warts. Cost: Minimal.
- Stress reduction: Stress management techniques, such as exercise, meditation, or counseling, may help boost the immune system and reduce the recurrence of warts. Cost: Varies depending on the chosen method.
- Healthy diet: Consuming a balanced diet rich in fruits, vegetables, and immune-boosting nutrients may help support the immune system’s ability to fight off HPV infections. Cost: Varies depending on food choices.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – S03 Warts (ICD-10:B07)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Warts effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Warts. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Ockenfels HM. Therapeutic management of cutaneous and genital warts. J Dtsch Dermatol Ges. 2016;14(9):892-899.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Geneva: WHO; 2019.
- Jablonska S, Majewski S, Obalek S, Orth G. Cutaneous warts. Clin Dermatol. 1997;15(3):309-319.
- Doorbar J, Egawa N, Griffin H, Kranjec C, Murakami I. Human papillomavirus molecular biology and disease association. Rev Med Virol. 2015;25 Suppl 1:2-23.
- Sterling JC, Gibbs S, Haque Hussain SS, Mohd Mustapa MF, Handfield-Jones SE. British Association of Dermatologists’ guidelines for the management of cutaneous warts 2014. Br J Dermatol. 2014;171(4):696-712.
- Lipke MM. An armamentarium of wart treatments. Clin Med Res. 2006;4(4):273-293.
- Cardoso JC, Calonje E. Cutaneous manifestations of human papillomaviruses: A review. Acta Dermatovenerol Alp Pannonica Adriat. 2011;20(3):145-154.
- Beutner KR, Tyring SK, Trofatter KF Jr, et al. Imiquimod, a patient-applied immune-response modifier for treatment of external genital warts. Antimicrob Agents Chemother. 1998;42(4):789-794.
- Kwok CS, Gibbs S, Bennett C, Holland R, Abbott R. Topical treatments for cutaneous warts. Cochrane Database Syst Rev. 2012;(9):CD001781.
- Loo SK, Tang WY. Warts (non-genital). BMJ Clin Evid. 2014;2014:1710.
Related articles
Made in USA