Introduction
Pruritus, commonly known as itching, is a symptom that can occur in various conditions and diseases. It is characterized by an unpleasant sensation that triggers the urge to scratch the affected area. Pruritus can significantly impact a person’s quality of life, causing discomfort and distress.[1] The aim of this guide is to provide healthcare professionals with a comprehensive approach to diagnosing and managing pruritus.
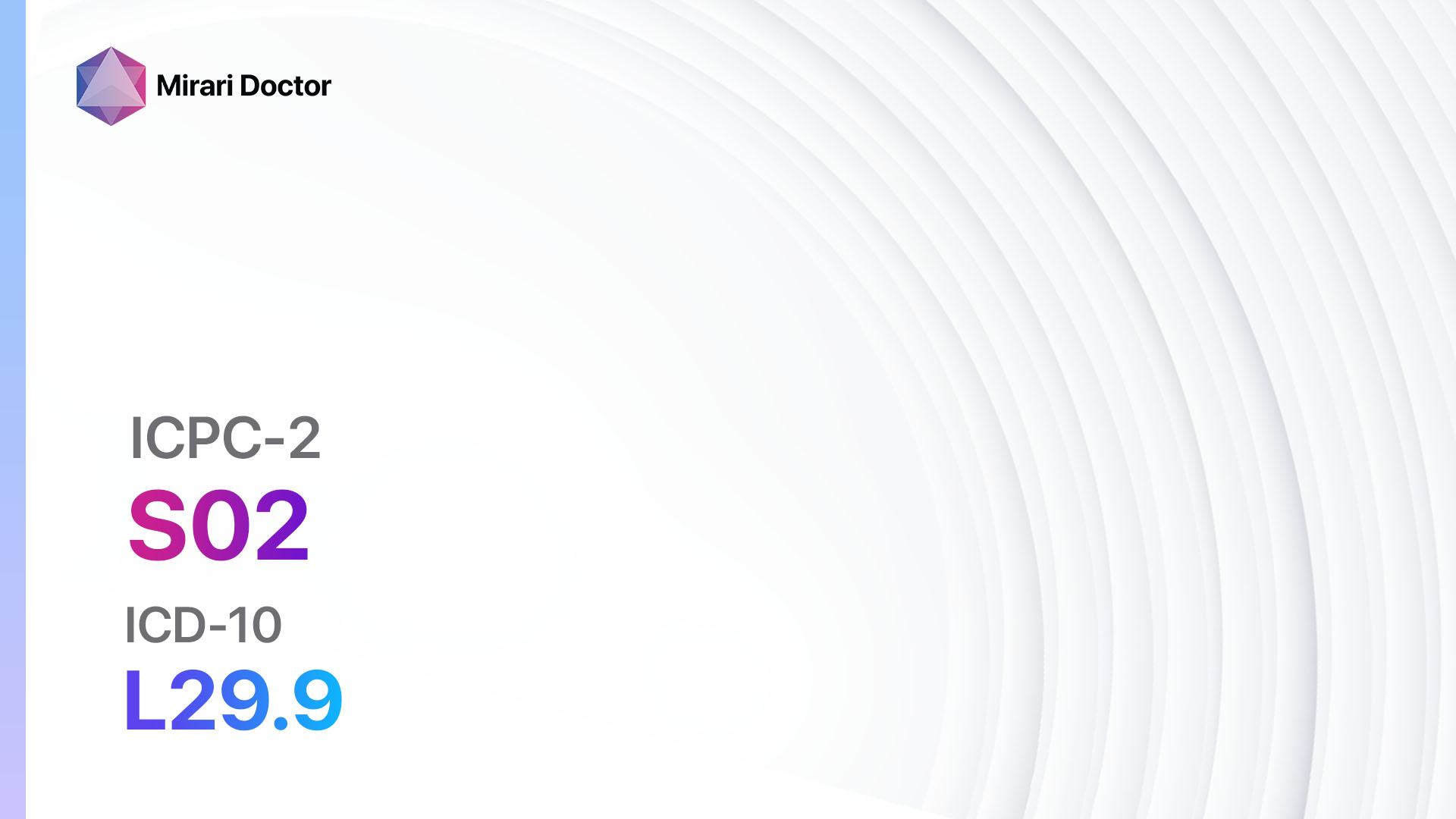
Codes
Symptoms
- Intense itching sensation
- Redness or rash in the affected area
- Dry or scaly skin
- Bumps or blisters
- Swelling or inflammation[3]
Causes
- Skin conditions: Eczema, psoriasis, dermatitis, hives
- Allergic reactions: Contact dermatitis, insect bites, medication allergies
- Systemic diseases: Liver disease, kidney disease, thyroid disorders
- Neurological conditions: Multiple sclerosis, neuropathy
- Infections: Fungal infections, scabies, lice
- Medications: Opioids, antifungals, antibiotics[4]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration, severity, and triggers of itching.
- Identify any underlying medical conditions or medications that may be contributing to pruritus.
- Assess the patient’s personal and family history of skin conditions or allergies.[5]
Physical Examination
- Inspect the affected area for any visible signs of skin inflammation, redness, or rash.
- Palpate the skin to assess for texture, moisture, and temperature changes.
- Examine other areas of the body for potential secondary skin lesions or systemic signs of disease.[6]
Determine Severity
- Mild pruritus: Occasional itching that does not significantly impact daily activities.
- Moderate pruritus: Frequent itching that causes discomfort and affects daily functioning.
- Severe pruritus: Constant itching that interferes with sleep, work, and quality of life.[7]
Laboratory Tests
- Complete blood count (CBC): To assess for any underlying systemic diseases or infections.
- Liver function tests: To evaluate liver function in cases of suspected liver disease.
- Kidney function tests: To assess renal function in cases of suspected kidney disease.
- Thyroid function tests: To evaluate thyroid hormone levels in cases of suspected thyroid disorders.
- Allergy testing: To identify potential allergens causing pruritus.[8]
Diagnostic Imaging
- No diagnostic imaging is typically necessary for the diagnosis of pruritus.
Other Tests
- Skin biopsy: In cases where the cause of pruritus is unclear, a skin biopsy may be performed to evaluate for underlying skin conditions or diseases.
- Patch testing: To identify potential allergens causing contact dermatitis.
- Scabies or lice examination: Microscopic examination of skin scrapings or hair to identify the presence of scabies mites or lice.[9]
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the effectiveness of treatment and adjust management strategies if needed.
- Provide patient education on proper skincare, avoiding triggers, and managing itching episodes.
- Discuss the importance of adhering to prescribed medications and lifestyle modifications.[10]
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Pruritus:
- Antihistamines (e.g., Diphenhydramine, Loratadine):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: Glaucoma, urinary retention, severe liver disease.
- Side effects: Drowsiness, dry mouth, blurred vision.
- Severe side effects: Seizures, irregular heartbeat.
- Drug interactions: Alcohol, sedatives, other antihistamines.
- Warning: May cause drowsiness, avoid driving or operating machinery.
- Topical corticosteroids (e.g., Hydrocortisone, Betamethasone):
- Cost: Generic versions can be $5-$30/tube.
- Contraindications: Skin infections, open wounds, rosacea.
- Side effects: Thinning of the skin, skin discoloration, acne.
- Severe side effects: Allergic reactions, adrenal suppression.
- Drug interactions: None significant.
- Warning: Prolonged use may lead to skin thinning and increased risk of infections.
- Topical calcineurin inhibitors (e.g., Tacrolimus, Pimecrolimus):
- Cost: Generic versions can be $50-$200/tube.
- Contraindications: Skin infections, open wounds, skin cancer.
- Side effects: Burning or stinging sensation, skin redness.
- Severe side effects: Increased risk of skin infections, skin cancer.
- Drug interactions: None significant.
- Warning: Long-term safety is still being studied, avoid excessive sun exposure.
- Opioid antagonists (e.g., Naltrexone):
- Cost: Generic versions can be $20-$100/month.
- Contraindications: Opioid use, acute hepatitis, liver failure.
- Side effects: Nausea, headache, abdominal pain.
- Severe side effects: Liver toxicity, allergic reactions.
- Drug interactions: Opioids, alcohol, certain antidepressants.
- Warning: Requires close monitoring of liver function.
- Immunosuppressants (e.g., Cyclosporine, Methotrexate):
- Cost: Generic versions can be $50-$300/month.
- Contraindications: Active infections, liver or kidney disease.
- Side effects: Increased risk of infections, gastrointestinal symptoms.
- Severe side effects: Kidney or liver damage, bone marrow suppression.
- Drug interactions: Many potential interactions, consult a pharmacist.
- Warning: Requires regular monitoring of blood counts and organ function.
Alternative Drugs:
- Capsaicin cream: Derived from chili peppers, it can help relieve itching by desensitizing nerve endings. Cost: $10-$30/tube.
- Menthol or camphor-based creams: Cooling effect can provide temporary relief from itching. Cost: $5-$20/tube.
- Antidepressants: Certain antidepressants, such as doxepin, can help relieve itching. Cost: Varies depending on the specific medication.
Surgical Procedures:
- No surgical procedures are typically indicated for the treatment of pruritus.
Alternative Interventions
- Acupuncture: May help reduce itching sensation and promote relaxation. Cost: $60-$120 per session.
- Hypnotherapy: Can help manage itching through relaxation techniques and suggestion. Cost: $75-$150 per session.
- Aromatherapy: Essential oils like lavender or chamomile may provide relief from itching. Cost: Varies depending on the specific oils.
- Herbal supplements: Some herbs, such as chamomile or calendula, may have anti-inflammatory properties. Cost: Varies depending on the specific supplement.
Lifestyle Interventions
- Avoiding triggers: Identify and avoid potential triggers, such as certain fabrics, soaps, or allergens.
- Moisturizing: Regularly moisturize the skin to prevent dryness and itching. Cost: $5-$20/bottle.
- Cool compresses: Apply cool compresses to the affected area to relieve itching. Cost: $5-$10/pack.
- Stress management: Practice stress-reducing techniques, such as meditation or yoga, to minimize itching episodes. Cost: Varies depending on the specific technique.
- Proper hygiene: Maintain good hygiene practices to prevent skin infections. Cost: Varies depending on personal care products.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – S02 Pruritus (ICD-10:L29.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 10 (Dermatitis/Fungus) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 5 (Lungs) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Pruritus effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Pruritus. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Yosipovitch G, Bernhard JD. Clinical practice. Chronic pruritus. N Engl J Med. 2013;368(17):1625-1634.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Geneva: WHO; 2019.
- Ständer S, Weisshaar E, Mettang T, et al. Clinical classification of itch: a position paper of the International Forum for the Study of Itch. Acta Derm Venereol. 2007;87(4):291-294.
- Oaklander AL. Neuropathic itch. Semin Cutan Med Surg. 2011;30(2):87-92.
- Weisshaar E, Szepietowski JC, Darsow U, et al. European guideline on chronic pruritus. Acta Derm Venereol. 2012;92(5):563-581.
- Patel T, Yosipovitch G. Therapy of pruritus. Expert Opin Pharmacother. 2010;11(10):1673-1682.
- Reich A, Heisig M, Phan NQ, et al. Visual analogue scale: evaluation of the instrument for the assessment of pruritus. Acta Derm Venereol. 2012;92(5):497-501.
- Mettang T, Kremer AE. Uremic pruritus. Kidney Int. 2015;87(4):685-691.
- Elmariah SB, Lerner EA. Topical therapies for pruritus. Semin Cutan Med Surg. 2011;30(2):118-126.
- Leslie TA. Itch management in the elderly. Curr Probl Dermatol. 2016;50:192-201.
Related articles
Made in USA