Introduction
Tuberculosis (TB) is a contagious bacterial infection that primarily affects the lungs but can also affect other parts of the body[1]. It is caused by the bacteria Mycobacterium tuberculosis and is spread through the air when an infected person coughs or sneezes[2]. TB can be a serious condition if left untreated, but it is curable with appropriate treatment[3]. The aim of this guide is to provide a comprehensive overview of the diagnosis and management of tuberculosis.
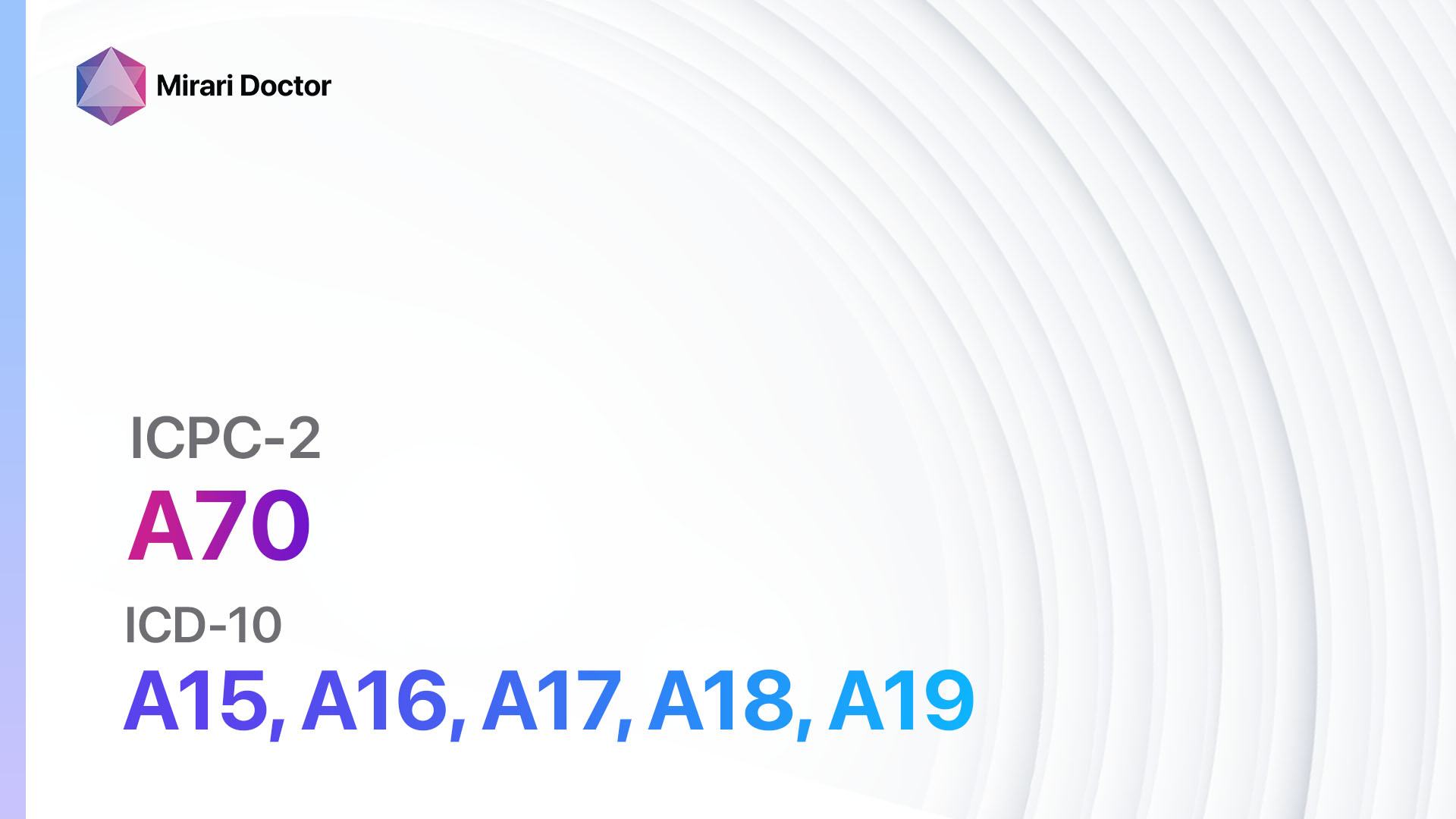
Codes
Symptoms
- Cough that lasts for more than three weeks[4]
- Chest pain
- Coughing up blood or sputum[5]
- Fatigue and weakness
- Weight loss
- Loss of appetite
- Night sweats
- Fever
- Chills
Causes
- Infection with Mycobacterium tuberculosis bacteria[6]
- Close contact with an infected person[7]
- Weakened immune system, such as HIV infection or certain medications[8]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration and severity of cough, presence of blood in sputum, weight loss, and night sweats.
- Ask about any known exposure to tuberculosis, such as close contact with an infected person.
- Assess the patient’s medical history, including any underlying medical conditions, such as HIV infection or diabetes, that may increase the risk of tuberculosis.
Physical Examination
- Perform a thorough physical examination, paying special attention to the lungs and lymph nodes.
- Look for signs of respiratory distress, such as rapid breathing or increased work of breathing.
- Check for enlarged lymph nodes, especially in the neck and armpits.
Laboratory Tests
- Sputum smear microscopy: This test involves examining a sample of sputum under a microscope to look for the presence of acid-fast bacilli, which are characteristic of tuberculosis[9].
- Sputum culture: A sputum sample is cultured in a laboratory to grow and identify the bacteria causing tuberculosis. This test can also determine the drug susceptibility of the bacteria[10].
- Interferon-gamma release assays (IGRAs): These blood tests can help diagnose latent tuberculosis infection by detecting the release of interferon-gamma in response to specific tuberculosis antigens.
- Chest X-ray: An X-ray of the chest can reveal abnormalities in the lungs, such as infiltrates or cavities, which may indicate tuberculosis.
- CT scan: A CT scan may be performed to obtain more detailed images of the lungs or other affected areas.
- Molecular tests: Polymerase chain reaction (PCR) tests can detect the DNA of Mycobacterium tuberculosis in sputum or other samples, providing a rapid diagnosis.
Diagnostic Imaging
- Chest X-ray: A chest X-ray is commonly used to evaluate the lungs for signs of tuberculosis, such as infiltrates or cavities.
- CT scan: A CT scan may be performed to obtain more detailed images of the lungs or other affected areas, especially if the chest X-ray is inconclusive.
Other Tests
- Tuberculin skin test (TST): This test involves injecting a small amount of purified protein derivative (PPD) into the skin and assessing the reaction after 48 to 72 hours. A positive reaction indicates exposure to tuberculosis but does not differentiate between latent infection and active disease.
- GeneXpert MTB/RIF assay: This molecular test can detect the DNA of Mycobacterium tuberculosis and also determine the presence of rifampicin resistance, a common drug resistance in tuberculosis.
Follow-up and Patient Education
- Provide education to the patient about tuberculosis, including the importance of completing the full course of treatment, infection control measures, and the need for regular follow-up visits.
- Schedule regular follow-up visits to monitor treatment response and assess for any adverse effects of medications.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Tuberculosis:
- Isoniazid (INH):
- Cost: $10-$50 for a 6-month course.
- Contraindications: Severe liver disease, history of INH-induced hepatitis.
- Side effects: Nausea, vomiting, peripheral neuropathy.
- Severe side effects: Hepatitis, severe skin reactions.
- Drug interactions: Rifampin, antiretroviral medications.
- Warning: Regular liver function tests required.
- Rifampin:
- Cost: $10-$50 for a 6-month course.
- Contraindications: Severe liver disease, history of rifampin-induced hepatitis.
- Side effects: Nausea, vomiting, orange discoloration of urine.
- Severe side effects: Hepatitis, severe skin reactions.
- Drug interactions: Isoniazid, antiretroviral medications.
- Warning: Regular liver function tests required.
- Pyrazinamide:
- Cost: $10-$50 for a 6-month course.
- Contraindications: Severe liver disease, acute gout.
- Side effects: Nausea, vomiting, joint pain.
- Severe side effects: Hepatitis, severe skin reactions.
- Drug interactions: None of major concern.
- Warning: Regular liver function tests required.
- Ethambutol:
- Cost: $10-$50 for a 6-month course.
- Contraindications: Optic neuritis, severe liver disease.
- Side effects: Vision changes, joint pain.
- Severe side effects: Optic neuritis, severe skin reactions.
- Drug interactions: None of major concern.
- Warning: Regular eye examinations required.
- Streptomycin:
- Cost: $10-$50 for a 6-month course.
- Contraindications: Severe kidney disease, severe hearing loss.
- Side effects: Nausea, vomiting, hearing loss.
- Severe side effects: Kidney damage, severe skin reactions.
- Drug interactions: None of major concern.
- Warning: Regular kidney function tests required.
Alternative Drugs:
- Levofloxacin: An alternative to isoniazid for the treatment of latent tuberculosis infection.
- Moxifloxacin: An alternative to isoniazid for the treatment of latent tuberculosis infection.
- Ethionamide: An alternative to pyrazinamide for the treatment of drug-resistant tuberculosis.
- Cycloserine: An alternative to ethambutol for the treatment of drug-resistant tuberculosis.
- Linezolid: An alternative for the treatment of extensively drug-resistant tuberculosis.
Surgical Procedures:
- Surgery is not typically indicated for the treatment of tuberculosis. However, in rare cases, surgical intervention may be necessary to remove infected lung tissue or to drain abscesses.
Alternative Interventions
- There are no alternative interventions that have been proven to effectively treat tuberculosis. It is important to follow the recommended standard treatment regimen for the best outcomes.
Lifestyle Interventions
- Adherence to the prescribed medication regimen is crucial for successful treatment of tuberculosis.
- Patients should be educated about the importance of infection control measures, such as covering the mouth and nose when coughing or sneezing, and proper disposal of tissues.
- A healthy diet and regular exercise can help support the immune system and aid in recovery from tuberculosis.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Video instructions for using Mirari Cold Plasma Device – A01 Pain general/multiple sites (ICD-10:M79.6, R07.4, R10.4, R51)
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – A70 Tuberculosis (ICD-10:A15, A16, A17, A18, A19)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 3 (Antiviral Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 3 (Antiviral Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD | Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, | Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520USD – $3,360 USD | Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD |
 |
|
Use the Mirari Cold Plasma device to treat Tuberculosis effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Tuberculosis. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- World Health Organization. (2021). Tuberculosis. //www.who.int/news-room/fact-sheets/detail/tuberculosis
- Centers for Disease Control and Prevention. (2021). How TB Spreads. //www.cdc.gov/tb/topic/basics/howtbspreads.htm
- National Institute of Allergy and Infectious Diseases. (2018). Tuberculosis (TB) Treatment. //www.niaid.nih.gov/diseases-conditions/tuberculosis-treatment
- Mayo Clinic. (2021). Tuberculosis. //www.mayoclinic.org/diseases-conditions/tuberculosis/symptoms-causes/syc-20351250
- American Lung Association. (2022). Tuberculosis Symptoms and Diagnosis. //www.lung.org/lung-health-diseases/lung-disease-lookup/tuberculosis/symptoms-diagnosis
- Narasimhan, P., Wood, J., MacIntyre, C. R., & Mathai, D. (2013). Risk factors for tuberculosis. Pulmonary medicine, 2013, 828939. //doi.org/10.1155/2013/828939
- NHS. (2023). Tuberculosis (TB) – Causes. //www.nhs.uk/conditions/tuberculosis-tb/causes/
- Ai, J. W., Ruan, Q. L., Liu, Q. H., & Zhang, W. H. (2016). Updates on the risk factors for latent tuberculosis reactivation and their managements. Emerging microbes & infections, 5(2), e10. //doi.org/10.1038/emi.2016.10
- Desikan P. (2013). Sputum smear microscopy in tuberculosis: is it still relevant?. The Indian journal of medical research, 137(3), 442–444.
- Pfyffer, G. E., & Wittwer, F. (2012). Incubation time of mycobacterial cultures: how long is long enough to issue a final negative report to the clinician?. Journal of clinical microbiology, 50(12), 4188–4189. //doi.org/10.1128/JCM.02283-12
Related articles
Made in USA