Introduction
Risk factors for malignancy play a crucial role in the development and progression of cancer. Identifying these risk factors is essential for early detection, prevention, and management of malignancies[1]. This guide aims to provide healthcare professionals with a comprehensive understanding of the symptoms, causes, diagnostic steps, possible interventions, and patient education related to risk factors for malignancy.
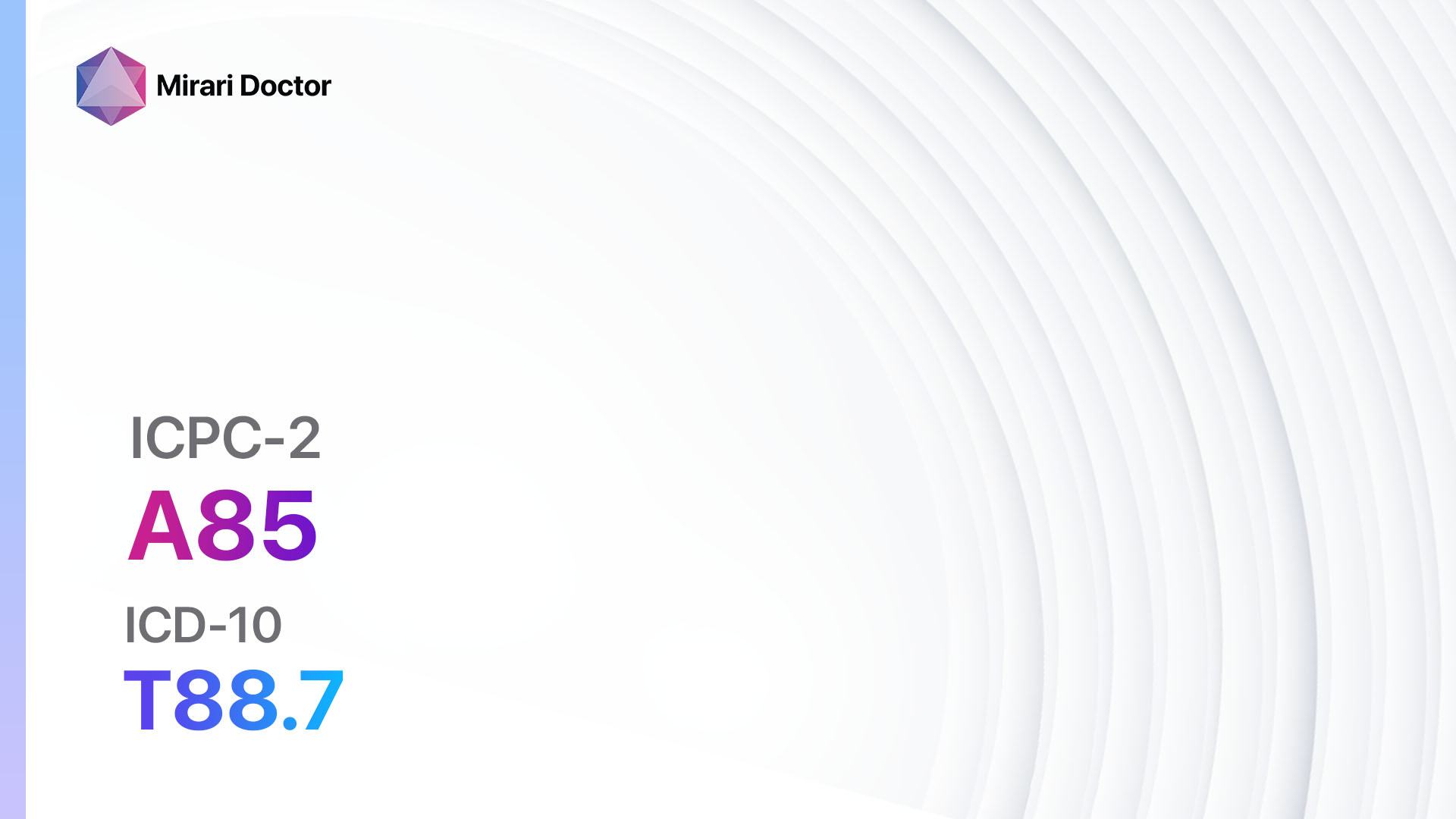
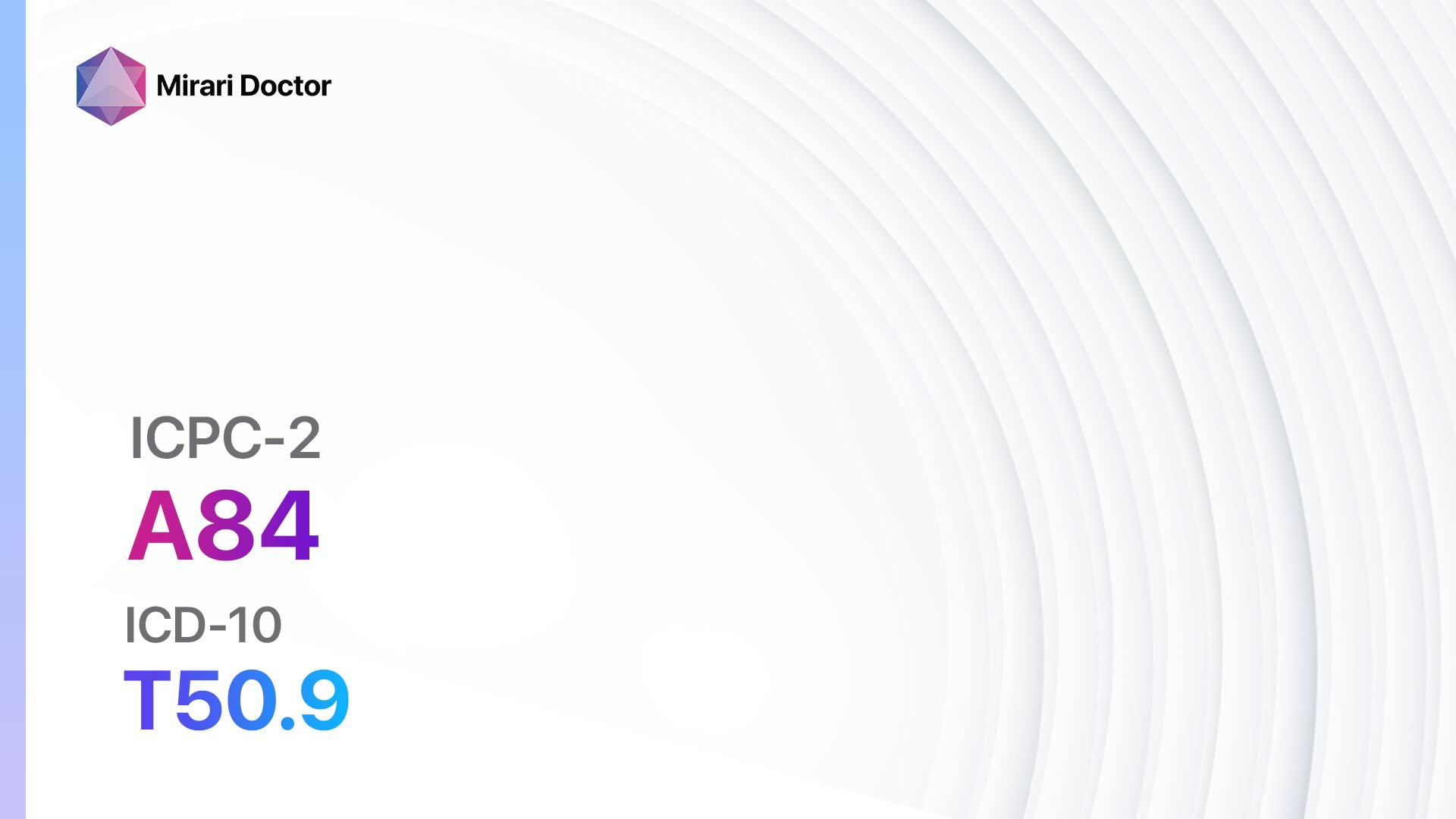
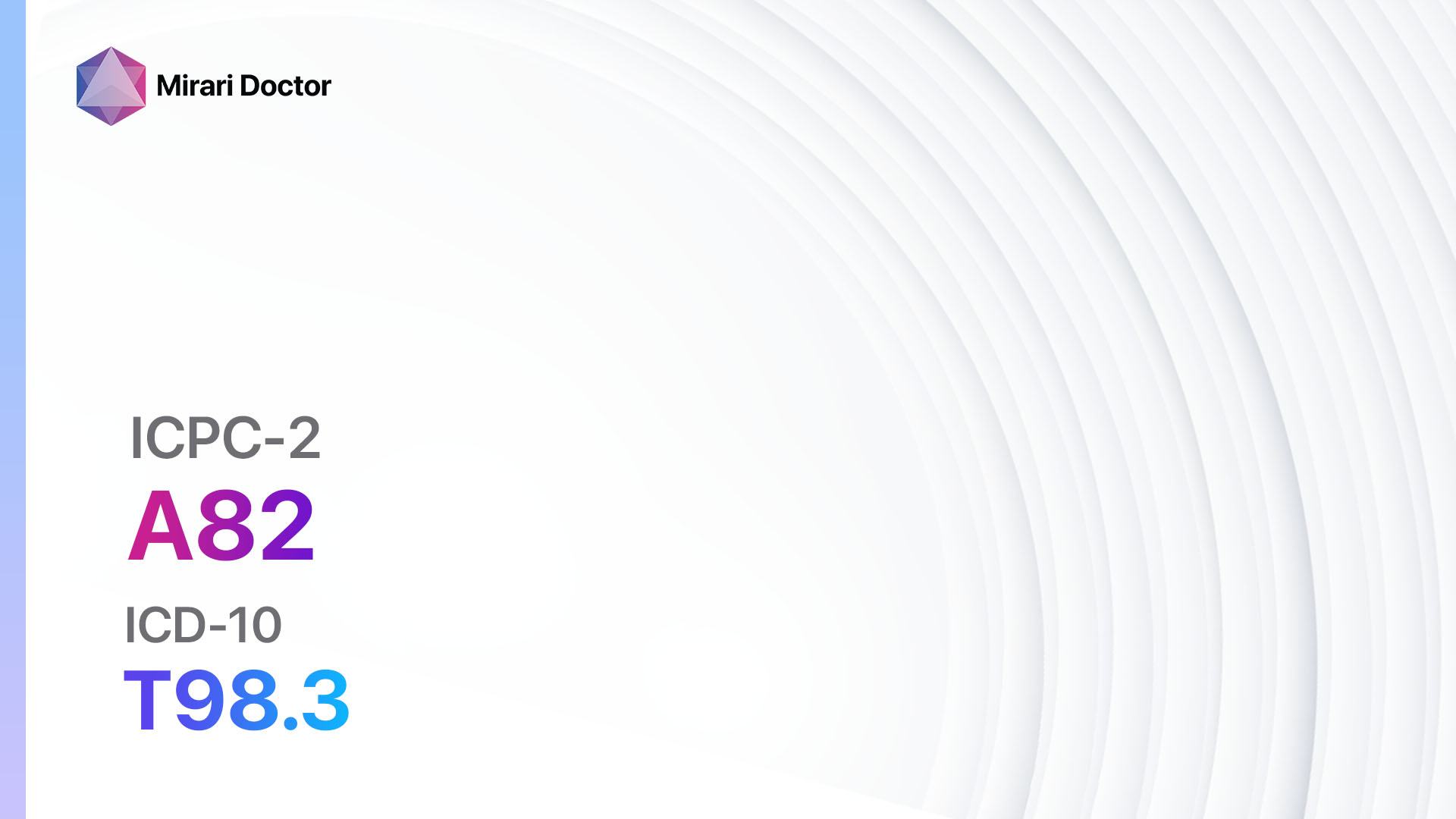
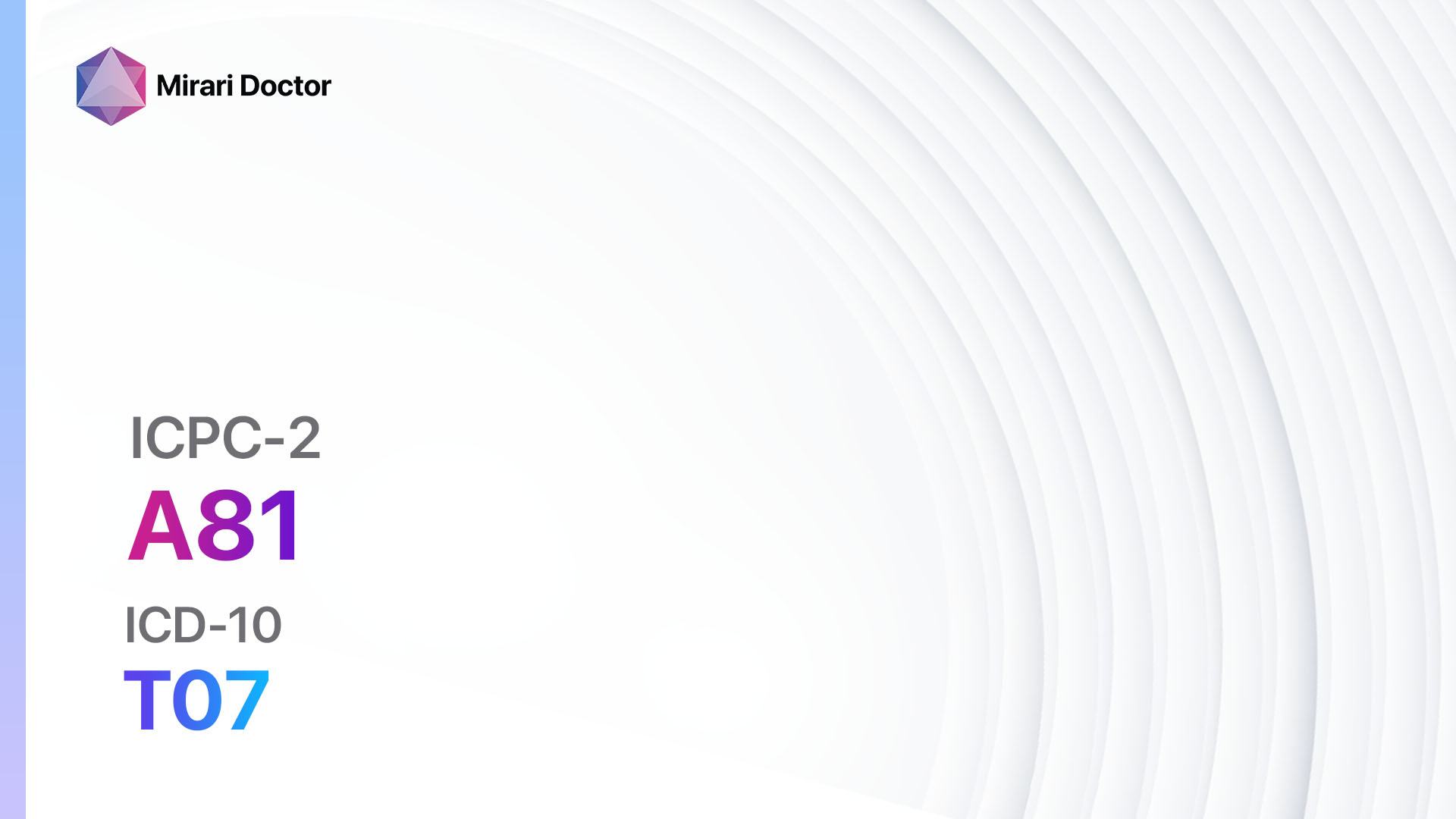
Codes
Symptoms
- Unexplained weight loss: Significant and unintentional weight loss without any known cause[2]
- Fatigue: Persistent tiredness and lack of energy[3].
- Changes in the skin: New moles, changes in the size, shape, or color of existing moles, or the appearance of sores that do not heal[4].
- Persistent pain: Unexplained and persistent pain that does not go away[5]
- Changes in bowel or bladder habits: Changes in bowel movements, such as diarrhea or constipation, or changes in bladder function, such as frequent urination or blood in the urine[6].
- Difficulty swallowing: Persistent difficulty or pain while swallowing[7].
- Persistent cough: A cough that lasts for an extended period, especially if accompanied by blood[8].
- Changes in the breast: Changes in the size, shape, or appearance of the breast, nipple discharge, or skin changes on the breast[9].
- Abnormal bleeding: Unexplained bleeding, such as bleeding between periods, after menopause, or from the rectum[10].
- Difficulty breathing: Persistent shortness of breath or wheezing.
Causes
- Genetic factors: Inherited gene mutations that increase the risk of developing certain types of cancer, such as BRCA1 and BRCA2 mutations for breast and ovarian cancer.
- Environmental factors: Exposure to carcinogens, such as tobacco smoke, asbestos, radiation, certain chemicals, and pollutants.
- Lifestyle factors: Unhealthy habits, including smoking, excessive alcohol consumption, poor diet, lack of physical activity, and obesity.
- Age: The risk of developing cancer increases with age.
- Family history: Having a close relative, such as a parent or sibling, who has had cancer.
- Previous cancer history: A history of certain types of cancer increases the risk of developing other types.
- Chronic infections: Infections caused by certain viruses, bacteria, or parasites, such as human papillomavirus (HPV), hepatitis B and C, and Helicobacter pylori.
Diagnostic Steps
Medical History
- Gather information about the patient’s personal and family medical history, including any previous cancer diagnoses.
- Assess the patient’s lifestyle habits, including smoking, alcohol consumption, diet, and physical activity.
- Identify any known risk factors, such as exposure to carcinogens or chronic infections.
- Evaluate the presence of symptoms associated with malignancy.
Physical Examination
- Perform a thorough physical examination, focusing on specific signs or findings indicative of cancer, such as lumps, skin changes, enlarged lymph nodes, or abnormal masses.
- Conduct a breast examination for any abnormalities or changes.
- Examine the oral cavity for signs of oral cancer, such as ulcers or white or red patches.
- Assess the abdomen for any masses or organ enlargement.
- Evaluate the skin for any suspicious moles or lesions.
Laboratory Tests
- Complete blood count (CBC): To assess for any abnormalities, such as anemia or abnormal white blood cell counts.
- Tumor markers: Blood tests to detect specific substances produced by cancer cells, such as prostate-specific antigen (PSA) for prostate cancer or CA-125 for ovarian cancer.
- Liver function tests: To evaluate liver health and detect any abnormalities that may indicate liver cancer.
- Kidney function tests: To assess kidney health and detect any abnormalities that may indicate kidney cancer.
- Human papillomavirus (HPV) testing: To detect the presence of high-risk HPV strains associated with cervical and other cancers.
- Genetic testing: In cases with a strong family history of cancer, genetic testing may be performed to identify specific gene mutations.
Diagnostic Imaging
- X-rays: To visualize and assess abnormalities in the bones, lungs, or other areas of the body.
- Ultrasound: To evaluate organs, such as the liver, kidneys, or reproductive organs, for any masses or abnormalities.
- Computed tomography (CT) scan: Provides detailed cross-sectional images of the body to detect tumors or abnormalities.
- Magnetic resonance imaging (MRI): Uses powerful magnets and radio waves to create detailed images of the body, particularly useful for assessing the brain, spine, and soft tissues.
- Positron emission tomography (PET) scan: A nuclear medicine imaging technique that uses a radioactive tracer to detect areas of increased metabolic activity, often indicative of cancer.
Other Tests
- Biopsy: The removal of a small sample of tissue for examination under a microscope to determine if cancer cells are present.
- Endoscopy: The use of a flexible tube with a camera to visualize and obtain tissue samples from the digestive tract, respiratory system, or other organs.
- Pap smear: A test to detect abnormal cells in the cervix, which may indicate cervical cancer.
- Colonoscopy: A procedure to examine the colon and rectum for abnormalities or signs of colorectal cancer.
- Mammography: X-ray imaging of the breasts to detect early signs of breast cancer.
- Prostate-specific antigen (PSA) test: A blood test to measure the levels of PSA, a protein produced by the prostate gland, which may indicate prostate cancer.
Follow-up and Patient Education
- Provide patients with the necessary information about their diagnosis, including the type and stage of cancer, treatment options, and prognosis.
- Discuss the importance of regular follow-up appointments, screenings, and tests to monitor the progression of the disease and response to treatment.
- Educate patients about lifestyle modifications, such as smoking cessation, healthy diet, regular exercise, and sun protection, to reduce the risk of cancer or its recurrence.
- Offer emotional support and resources, such as support groups or counseling services, to help patients cope with the diagnosis and treatment process.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Risk factor for malignancy:
- Tamoxifen:
- Cost: $50-$200/month.
- Contraindications: History of blood clots, pregnancy, or breastfeeding.
- Side effects: Hot flashes, vaginal discharge, mood changes.
- Severe side effects: Increased risk of uterine cancer, blood clots.
- Drug interactions: Anticoagulants, selective serotonin reuptake inhibitors (SSRIs).
- Warning: Regular monitoring of liver function and blood clotting parameters required.
- Aromatase inhibitors (e.g., Anastrozole, Letrozole):
- Cost: $100-$500/month.
- Contraindications: Severe liver disease, pregnancy, or breastfeeding.
- Side effects: Joint pain, hot flashes, fatigue.
- Severe side effects: Osteoporosis, cardiovascular events.
- Drug interactions: Estrogen-containing medications, tamoxifen.
- Warning: Regular monitoring of bone density and liver function required.
- Immunotherapy (e.g., Pembrolizumab, Nivolumab):
- Cost: $10,000-$20,000/month.
- Contraindications: Severe autoimmune diseases, pregnancy, or breastfeeding.
- Side effects: Fatigue, skin rash, diarrhea.
- Severe side effects: Immune-related adverse events, organ damage.
- Drug interactions: None reported.
- Warning: Regular monitoring of immune function and potential side effects required.
- Chemotherapy (e.g., Paclitaxel, Doxorubicin):
- Cost: $3,000-$10,000/month.
- Contraindications: Severe bone marrow suppression, pregnancy, or breastfeeding.
- Side effects: Nausea, hair loss, fatigue.
- Severe side effects: Bone marrow suppression, organ damage.
- Drug interactions: Many potential interactions, depending on the specific chemotherapy agents used.
- Warning: Regular monitoring of blood counts and organ function required.
- Targeted therapy (e.g., Trastuzumab, Imatinib):
- Cost: $5,000-$15,000/month.
- Contraindications: Severe heart disease, pregnancy, or breastfeeding.
- Side effects: Fatigue, diarrhea, skin rash.
- Severe side effects: Cardiotoxicity, liver toxicity.
- Drug interactions: Many potential interactions, depending on the specific targeted therapy agents used.
- Warning: Regular monitoring of heart function and liver function required.
Alternative Drugs:
- Herbal supplements: Some herbal supplements, such as green tea extract or curcumin, may have potential benefits in reducing the risk of certain types of cancer. Cost: Varies depending on the specific supplement.
- Vitamin D: Adequate vitamin D levels have been associated with a reduced risk of certain cancers. Cost: $10-$30/month.
- Aspirin: Regular low-dose aspirin use has been shown to reduce the risk of colorectal cancer. Cost: <$10/month.
- Statins: Some studies suggest that statins may have a protective effect against certain types of cancer. Cost: Generic versions can be $3-$50/month.
- Metformin: This diabetes medication has been associated with a reduced risk of certain cancers. Cost: $10-$50/month.
Surgical Procedures:
- Prophylactic mastectomy: Removal of one or both breasts to reduce the risk of breast cancer in high-risk individuals. Cost: $10,000-$20,000.
- Prophylactic oophorectomy: Removal of the ovaries to reduce the risk of ovarian cancer in high-risk individuals. Cost: $10,000-$20,000.
- Colonoscopy with polyp removal: Removal of precancerous polyps during a colonoscopy to prevent the development of colorectal cancer. Cost: $1,000-$3,000.
- Hysterectomy: Removal of the uterus to reduce the risk of uterine cancer in high-risk individuals. Cost: $10,000-$20,000.
- Lung cancer screening: Low-dose CT scan for early detection of lung cancer in high-risk individuals, such as heavy smokers. Cost: $300-$500.
Alternative Interventions
- Acupuncture: May help manage cancer-related symptoms, such as pain, nausea, and fatigue. Cost: $60-$120 per session.
- Mind-body therapies: Techniques like meditation, yoga, and tai chi may help reduce stress and improve overall well-being. Cost: Varies depending on the specific therapy and location.
- Herbal supplements: Some herbal supplements, such as mistletoe extract or mushroom extracts, are used in complementary cancer care. Cost: Varies depending on the specific supplement.
- Massage therapy: Can provide relaxation, pain relief, and improved quality of life for cancer patients. Cost: $50-$100 per session.
- Dietary modifications: A healthy diet rich in fruits, vegetables, whole grains, and lean proteins may help reduce the risk of cancer. Cost: Varies depending on food choices and availability.
Lifestyle Interventions
- Smoking cessation: Quitting smoking is one of the most effective ways to reduce the risk of cancer. Cost: Varies depending on the chosen smoking cessation method.
- Healthy diet: Encourage a diet rich in fruits, vegetables, whole grains, and lean proteins while limiting processed foods, red meat, and sugary beverages. Cost: Varies depending on food choices and availability.
- Regular exercise: Engaging in regular physical activity can help reduce the risk of cancer and improve overall health. Cost: Varies depending on the chosen exercise program or gym membership.
- Sun protection: Encourage the use of sunscreen, protective clothing, and avoiding excessive sun exposure to reduce the risk of skin cancer
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – A21 Risk factor for malignancy (ICD-10:Z80)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD | Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, | Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890USD – $2,520 USD | Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD |
 |
|
Use the Mirari Cold Plasma device to treat Risk factor for malignancy effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Risk factor for malignancy. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the devic
- he device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Islami, F., Goding Sauer, A., Miller, K. D., Siegel, R. L., Fedewa, S. A., Jacobs, E. J., … & Jemal, A. (2018). Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA: a cancer journal for clinicians, 68(1), 31-54.
- Fearon, K., Strasser, F., Anker, S. D., Bosaeus, I., Bruera, E., Fainsinger, R. L., … & Baracos, V. E. (2011). Definition and classification of cancer cachexia: an international consensus. The lancet oncology, 12(5), 489-495.
- Bower, J. E. (2014). Cancer-related fatigue—mechanisms, risk factors, and treatments. Nature reviews Clinical oncology, 11(10), 597.
- Rigel, D. S., Russak, J., & Friedman, R. (2010). The evolution of melanoma diagnosis: 25 years beyond the ABCDs. CA: a cancer journal for clinicians, 60(5), 301-316.
- Falk, S., & Dickenson, A. H. (2014). Pain and nociception: mechanisms of cancer-induced bone pain. Journal of clinical oncology, 32(16), 1647.
- Stein, A., Voigt, W., & Jordan, K. (2010). Chemotherapy-induced diarrhea: pathophysiology, frequency and guideline-based management. Therapeutic advances in medical oncology, 2(1), 51-63.
- Gishen, F., & Tookman, A. (2013). Dysphagia in cancer. BMJ supportive & palliative care, 3(1), 72-76.
- Kvale, P. A. (2006). Chronic cough due to lung tumors: ACCP evidence-based clinical practice guidelines. Chest, 129(1), 147S-153S.
- Koo, M. M., von Wagner, C., Abel, G. A., McPhail, S., Rubin, G. P., & Lyratzopoulos, G. (2017). Typical and atypical presenting symptoms of breast cancer and their associations with diagnostic intervals: evidence from a national audit of cancer diagnosis. Cancer epidemiology, 48, 140-146.
- Tarney, C. M., & Han, J. (2014). Postcoital bleeding: a review on etiology, diagnosis, and management. Obstetrics and gynecology international, 2014.
Related articles
Made in USA