Introduction
Fainting, also known as syncope, is a temporary loss of consciousness due to a lack of blood flow to the brain. It can be caused by various factors and can have significant implications for the individual’s health and well-being.[1][2]The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnostic steps and possible interventions for fainting/syncope.
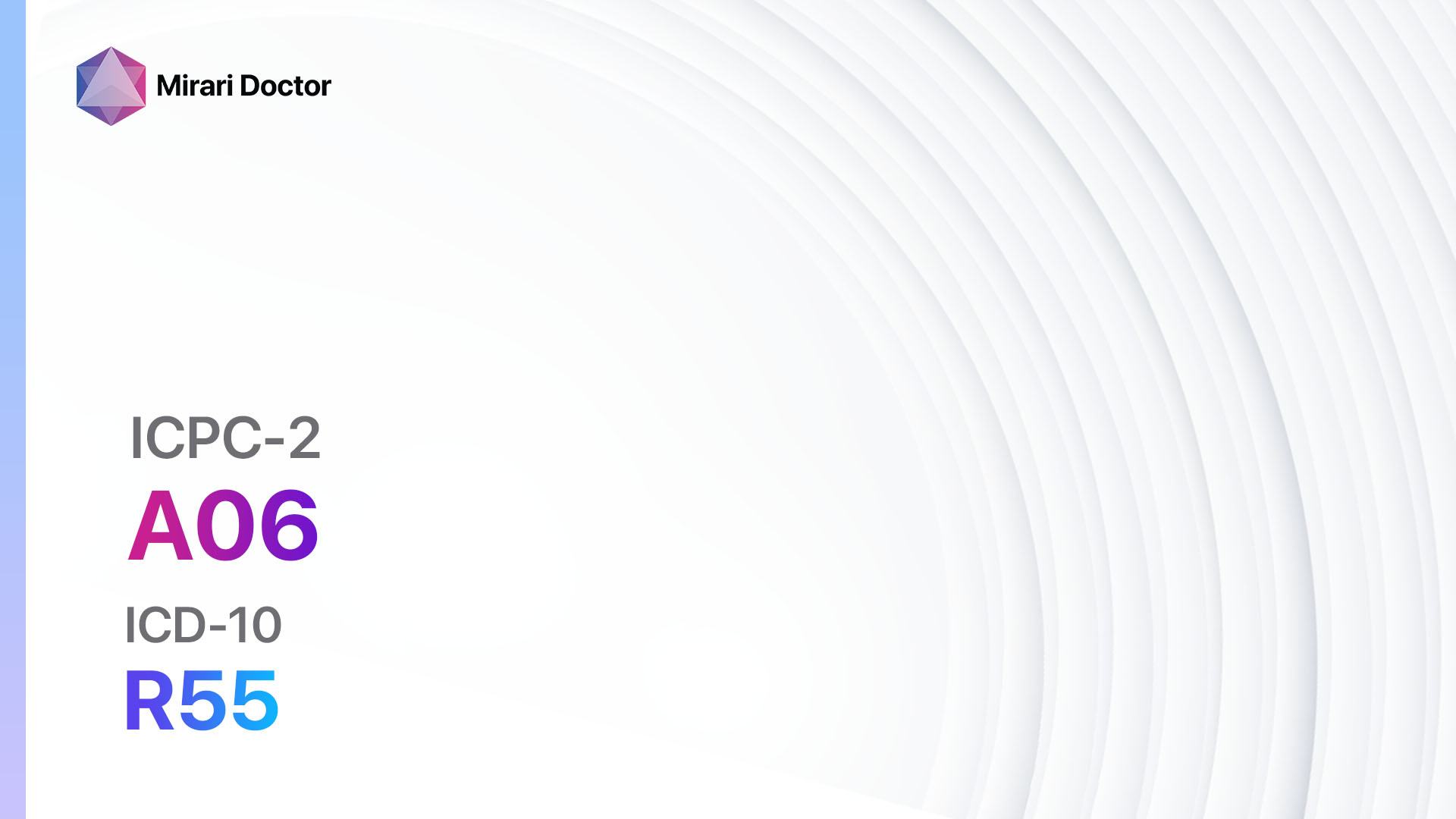
Codes
Symptoms
- Dizziness: Feeling lightheaded or unsteady.[5]
- Blurred vision: Difficulty seeing clearly.[6]
- Nausea: Feeling sick to the stomach.[7]
- Sweating: Excessive sweating.[8]
- Pale skin: Skin appears pale or clammy.[9]
- Loss of consciousness: Temporary loss of consciousness, usually lasting for a few seconds to a few minutes.[10]
Causes
- Vasovagal syncope: Triggered by emotional stress, pain, or the sight of blood.
- Orthostatic hypotension: A sudden drop in blood pressure when standing up.
- Cardiac syncope: Caused by an underlying heart condition, such as arrhythmias or structural abnormalities.
- Neurologic syncope: Due to neurological conditions, such as seizures or migraines.
- Medications: Certain medications can cause fainting as a side effect.
- Other factors: Dehydration, overheating, or prolonged standing.
Diagnostic Steps
Medical History
- Gather information about the patient’s fainting episodes, including frequency, duration, and triggers.
- Identify any underlying medical conditions, such as heart disease, diabetes, or neurological disorders.
- Assess the patient’s medication history, including any medications that may contribute to fainting.
- Inquire about family history of fainting or related conditions.
Physical Examination
- Measure blood pressure in different positions (lying down, sitting, standing) to assess for orthostatic hypotension.
- Check heart rate and rhythm to identify any abnormalities.
- Examine the skin for signs of dehydration or poor circulation.
- Evaluate neurological function, including reflexes and coordination.
Laboratory Tests
- Complete blood count (CBC): To check for anemia or infection.
- Electrolyte panel: To assess for imbalances that may contribute to fainting.
- Glucose level: To rule out hypoglycemia as a cause of fainting.
- Thyroid function tests: To evaluate thyroid function, as abnormalities can lead to fainting.
- Drug screen: To identify any substances that may be causing or contributing to fainting.
Diagnostic Imaging
- Electrocardiogram (ECG): To assess the electrical activity of the heart and identify any arrhythmias.
- Echocardiogram: To evaluate the structure and function of the heart.
- Holter monitor: A portable device that records the heart’s electrical activity over a period of time.
- Tilt table test: Measures changes in heart rate and blood pressure while the patient is tilted at different angles.
Other Tests
- Electrophysiological study: Invasive procedure to evaluate the electrical conduction system of the heart.
- Head-up tilt test: Similar to the tilt table test, but specifically focuses on changes in blood pressure and heart rate.
- Event monitor: A portable device that records the heart’s electrical activity when the patient experiences symptoms.
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the patient’s progress and adjust treatment as needed.
- Educate the patient about potential triggers and how to prevent fainting episodes.
- Provide information on lifestyle modifications and interventions to manage fainting.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Fainting/Syncope:
- Fludrocortisone:
- Cost: $10-$50/month.
- Contraindications: Hypersensitivity to fludrocortisone, systemic fungal infections.
- Side effects: Fluid retention, high blood pressure, low potassium levels.
- Severe side effects: Adrenal insufficiency, allergic reactions.
- Drug interactions: Nonsteroidal anti-inflammatory drugs (NSAIDs), potassium-sparing diuretics.
- Warning: Regular monitoring of blood pressure and electrolyte levels required.
- Midodrine:
- Cost: $30-$100/month.
- Contraindications: Severe organic heart disease, urinary retention.
- Side effects: Supine hypertension, piloerection (goosebumps), urinary urgency.
- Severe side effects: Hypertensive crisis, allergic reactions.
- Drug interactions: Beta-blockers, alpha-blockers.
- Warning: Regular monitoring of blood pressure required.
- Beta-blockers (e.g., Propranolol, Metoprolol):
- Cost: Generic versions are typically <$30/month.
- Contraindications: Severe bradycardia, heart block, uncontrolled heart failure.
- Side effects: Fatigue, dizziness, bradycardia.
- Severe side effects: Bronchospasm, heart block.
- Drug interactions: Calcium channel blockers, insulin.
- Warning: Should not be abruptly stopped.
- SSRIs (Selective Serotonin Reuptake Inhibitors) (e.g., Sertraline, Fluoxetine):
- Cost: Generic versions can be $3-$50/month.
- Contraindications: Hypersensitivity to SSRIs, concomitant use of MAO inhibitors.
- Side effects: Nausea, headache, sexual dysfunction.
- Severe side effects: Serotonin syndrome, suicidal thoughts.
- Drug interactions: MAO inhibitors, NSAIDs.
- Warning: Regular monitoring for changes in mood and behavior required.
- Disopyramide:
- Cost: $30-$100/month.
- Contraindications: Hypersensitivity to disopyramide, heart block, myasthenia gravis.
- Side effects: Dry mouth, urinary retention, constipation.
- Severe side effects: Ventricular arrhythmias, heart failure.
- Drug interactions: Anticholinergic drugs, beta-blockers.
- Warning: Regular monitoring of heart rhythm required.
Alternative Drugs:
- Fluoxetine: An SSRI that can help manage vasovagal syncope.
- Methylphenidate: A stimulant medication that may be used for neurocardiogenic syncope.
- Clonidine: A centrally acting alpha-2 agonist that can help regulate blood pressure.
- Droxidopa: A norepinephrine precursor that can be used for neurogenic orthostatic hypotension.
- Ivabradine: A medication that lowers heart rate and may be used for certain types of syncope.
Surgical Procedures:
- Pacemaker implantation: For patients with bradycardia or heart block.
- Cardiac ablation: A procedure to destroy abnormal heart tissue that may be causing arrhythmias.
- Implantable cardioverter-defibrillator (ICD) placement: For patients at high risk of life-threatening arrhythmias.
Alternative Interventions
- Acupuncture: May help improve blood flow and reduce symptoms of fainting. Cost: $60-$120 per session.
- Chelation therapy: Controversial treatment involving the administration of chelating agents to remove heavy metals from the body. Cost: $75-$150 per session.
- Biofeedback: A technique that teaches individuals to control certain bodily functions, such as heart rate and blood pressure. Cost: $50-$100 per session.
- Herbal supplements: Some herbs, such as ginkgo biloba and ginger, may have potential benefits for managing fainting. Cost: Varies depending on the specific supplement.
- Cognitive-behavioral therapy (CBT): A form of psychotherapy that helps individuals identify and change negative thought patterns and behaviors. Cost: $100-$200 per session.
Lifestyle Interventions
- Increase fluid and salt intake: Helps maintain blood volume and prevent orthostatic hypotension. Cost: Varies depending on dietary choices.
- Avoid triggers: Identify and avoid situations or activities that may lead to fainting episodes. Cost: None.
- Wear compression stockings: Helps improve blood flow and prevent blood pooling in the legs. Cost: $10-$50 per pair.
- Regular exercise: Improves cardiovascular fitness and can help regulate blood pressure. Cost: Varies depending on the chosen exercise program.
- Stress management techniques: Such as deep breathing exercises, meditation, or yoga. Cost: Varies depending on the chosen method.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. It is recommended to consult with a healthcare professional for personalized treatment options and cost estimates.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – A06 Fainting/syncope (ICD-10:R55)
| Mild | Moderate | Severe |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 7 (Immunotherapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 7 (Immunotherapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD | Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, | Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890USD – $2,520 USD | Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD |
 |
|
Use the Mirari Cold Plasma device to treat Fainting/syncope effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Fainting/syncope. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Syncope (Fainting) – Harvard Health. //www.health.harvard.edu/heart-health/syncope-fainting
- Syncope (Fainting) – American Heart Association. //www.heart.org/en/health-topics/arrhythmia/symptoms-diagnosis–monitoring-of-arrhythmia/syncope-fainting
- [ICPC-2 Code: A06 Fainting/syncope – RxReasoner. //www.rxreasoner.com/icpc2codes/A06
- [ICD-10 Code for Syncope and collapse R55 – AAPC. //www.aapc.com/codes/icd-10-codes/R55
- Dizziness and Vertigo – MedlinePlus. //medlineplus.gov/dizzinessandvertigo.html
- Blurred Vision – Mayo Clinic. //www.mayoclinic.org/diseases-conditions/blurred-vision/symptoms-causes/syc-20370753
- Nausea and Vomiting – CDC. //www.cdc.gov/ncbddd/vomitigandnausea/index.html
- Sweating – MedlinePlus. //medlineplus.gov/ency/article/003218.htm
- Pale Skin – MedlinePlus. //medlineplus.gov/ency/article/003217.htm
- Loss of Consciousness – MedlinePlus. //medlineplus.gov/ency/article/003200.htm
Related articles
Made in USA