Introduction
Benign neoplasm of the breast in females refers to the presence of non-cancerous growths or tumors in the breast tissue[1]. While these tumors are not cancerous, they can still cause symptoms and may require medical intervention[2]. The aim of this guide is to provide a comprehensive overview of the diagnosis and possible interventions for benign neoplasm of the breast in females.
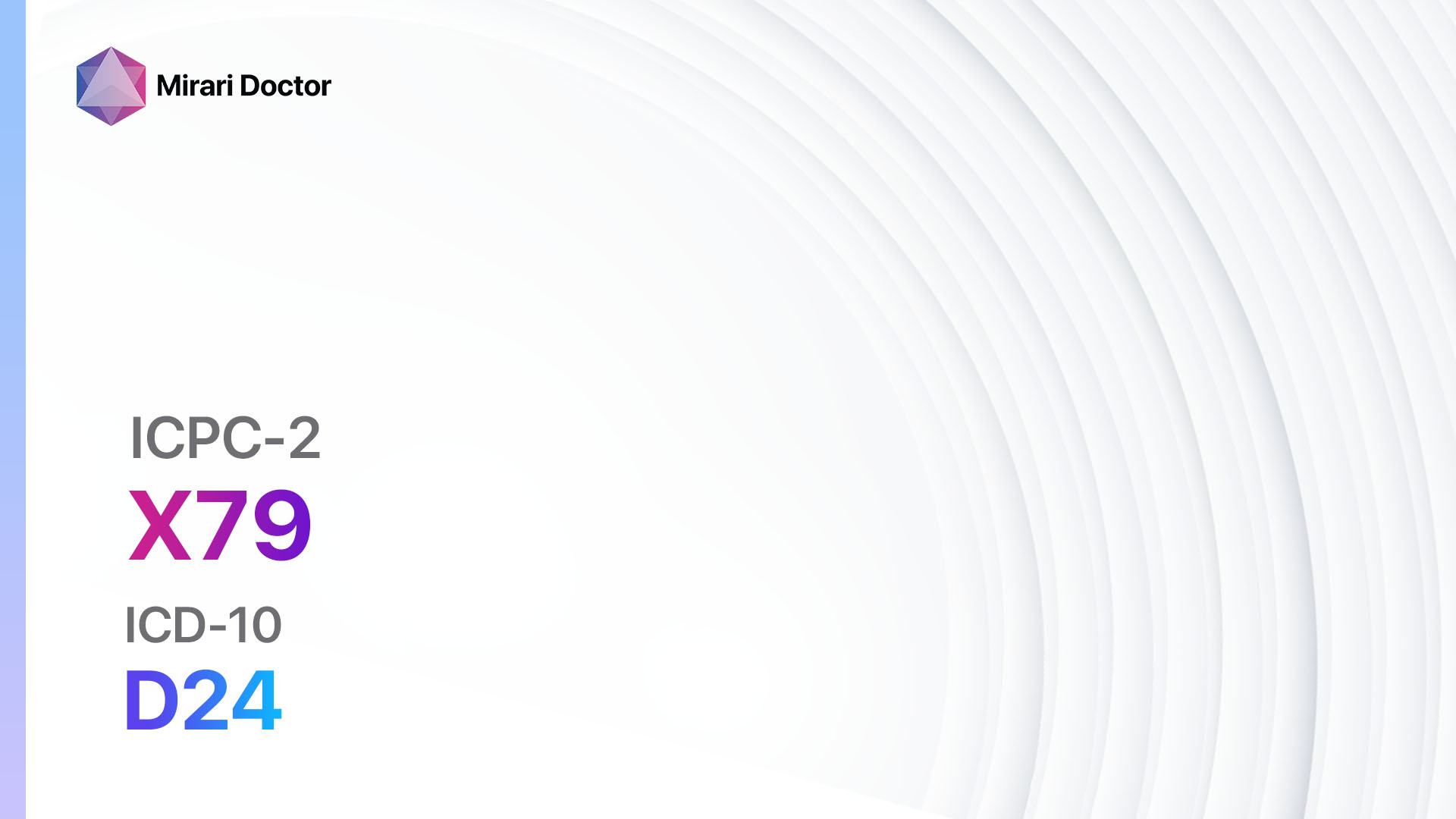
Codes
Symptoms
- Breast lump: A palpable lump or mass in the breast tissue[5].
- Breast pain: Discomfort or pain in the breast[5].
- Breast swelling: Swelling or enlargement of the breast[5].
- Changes in breast appearance: Changes in the size, shape, or texture of the breast[5].
- Nipple discharge: Discharge from the nipple, which may be clear, bloody, or of another color[5].
Causes
- Hormonal changes: Fluctuations in hormone levels, such as those that occur during the menstrual cycle or pregnancy, can contribute to the development of benign breast tumors[6].
- Hormone replacement therapy: The use of hormone replacement therapy, particularly estrogen and progesterone, may increase the risk of developing benign breast tumors[7].
- Family history: A family history of benign breast tumors or breast cancer may increase the risk of developing these tumors[8].
- Age: The risk of developing benign breast tumors increases with age, particularly after menopause[9].
Diagnostic Steps
Medical History
- Gather information about the patient’s risk factors, such as family history of breast tumors or breast cancer, hormonal changes, and use of hormone replacement therapy[10].
- Inquire about the patient’s symptoms, including the presence of breast lumps, breast pain, breast swelling, changes in breast appearance, and nipple discharge[10].
- Assess the patient’s overall health and medical conditions that may contribute to the development of benign breast tumors[10].
Physical Examination
- Perform a thorough physical examination of the breasts, including visual inspection and palpation[11].
- Look for any abnormalities in breast size, shape, or texture[11].
- Palpate the breasts to identify any lumps or masses[11].
- Examine the nipples for any discharge or changes in appearance[11].
Laboratory Tests
- Breast ultrasound: Uses sound waves to create images of the breast tissue and can help determine the nature of a breast lump or mass[12].
- Mammogram: An X-ray of the breast that can detect abnormalities, such as tumors or calcifications[13].
- Breast biopsy: Involves the removal of a small sample of breast tissue for further examination under a microscope to confirm the diagnosis of a benign breast tumor[14].
Diagnostic Imaging
- Breast MRI: Uses magnetic fields and radio waves to create detailed images of the breast tissue and can provide additional information about the nature of a breast tumor[15].
- Breast CT scan: A specialized X-ray technique that produces cross-sectional images of the breast tissue and can help evaluate the extent of a breast tumor[16].
- Breast PET scan: Involves the injection of a radioactive tracer into the bloodstream to detect areas of increased metabolic activity in the breast tissue[17].
Other Tests
- Genetic testing: In some cases, genetic testing may be recommended to assess the risk of developing breast tumors or cancer, particularly in individuals with a family history of these conditions[18].
- Hormone receptor testing: Determines whether the breast tumor cells have receptors for estrogen and progesterone, which can help guide treatment decisions[19].
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the progression of the benign breast tumor and assess for any changes in symptoms[20].
- Provide education to the patient about the nature of benign breast tumors, their management, and the importance of regular breast self-examinations and mammograms[20].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Benign neoplasm breast female:
- Tamoxifen[21]:
- Cost: $50-$200/month[22].
- Contraindications: History of blood clots, history of stroke, history of endometrial cancer[21].
- Side effects: Hot flashes, vaginal discharge, menstrual irregularities[21].
- Severe side effects: Increased risk of blood clots, increased risk of endometrial cancer[21].
- Drug interactions: Anticoagulants, selective serotonin reuptake inhibitors (SSRIs)[23].
- Warning: Regular monitoring of liver function and blood clotting parameters required[21].
- Danazol[24]:
- Cost: $100-$300/month[25].
- Contraindications: History of liver disease, history of breast cancer, history of blood clots[24].
- Side effects: Weight gain, acne, menstrual irregularities[24].
- Severe side effects: Liver damage, increased risk of blood clots[24].
- Drug interactions: Anticoagulants, cyclosporine[26].
- Warning: Regular monitoring of liver function and blood clotting parameters required[24].
- Bromocriptine[27]:
- Cost: $100-$200/month[28].
- Contraindications: History of heart disease, history of mental health disorders, history of liver disease[27].
- Side effects: Nausea, dizziness, fatigue[27].
- Severe side effects: Low blood pressure, hallucinations[27].
- Drug interactions: Antipsychotic medications, blood pressure medications[29].
- Warning: Regular monitoring of blood pressure and mental health required[27].
- Raloxifene[30]:
- Cost: $50-$150/month[31].
- Contraindications: History of blood clots, history of stroke, history of liver disease[30].
- Side effects: Hot flashes, leg cramps, increased risk of blood clots[30].
- Severe side effects: Increased risk of blood clots, increased risk of stroke[30].
- Drug interactions: Anticoagulants, hormone replacement therapy[32].
- Warning: Regular monitoring of liver function and blood clotting parameters required[30].
- Aromatase inhibitors (e.g., Anastrozole, Letrozole)[33]:
- Cost: $100-$300/month[34].
- Contraindications: History of liver disease, history of osteoporosis, history of heart disease[33].
- Side effects: Joint pain, hot flashes, fatigue[33].
- Severe side effects: Increased risk of osteoporosis, increased risk of heart disease[33].
- Drug interactions: Tamoxifen, estrogen-containing medications[35].
- Warning: Regular monitoring of bone density and liver function required[33].
Alternative Drugs:
- Progesterone cream: May help regulate hormone levels and reduce the growth of benign breast tumors. Cost: $20-$50/month[36].
- Vitamin E: An antioxidant that may have anti-inflammatory effects and help reduce breast pain. Cost: $10-$20/month[37].
- Green tea extract: Contains compounds that may have anti-cancer properties and help inhibit the growth of benign breast tumors. Cost: $10-$30/month[38].
- Curcumin: A compound found in turmeric that has anti-inflammatory and anti-cancer properties. Cost: $10-$30/month[39].
- DIM (diindolylmethane): A compound found in cruciferous vegetables that may help regulate hormone levels and reduce the growth of benign breast tumors. Cost: $20-$50/month[40].
Surgical Procedures:
- Lumpectomy: Involves the surgical removal of the benign breast tumor while preserving the surrounding breast tissue. Cost: $5,000-$15,000[41].
- Mastectomy: Involves the surgical removal of the entire breast to treat large or multiple benign breast tumors. Cost: $10,000-$30,000[41].
- Breast reconstruction: A surgical procedure performed after mastectomy to restore the shape and appearance of the breast. Cost: $5,000-$15,000[42].
Alternative Interventions
- Acupuncture: May help reduce breast pain and improve overall well-being. Cost: $60-$120 per session[43].
- Herbal supplements: Certain herbs, such as black cohosh and red clover, may have estrogen-like effects and help regulate hormone levels. Cost: Varies depending on the specific supplement[44].
- Dietary modifications: A diet rich in fruits, vegetables, and whole grains, and low in processed foods and saturated fats, may help reduce the growth of benign breast tumors. Cost: Varies depending on individual food choices[45].
- Stress reduction techniques: Practices such as yoga, meditation, and deep breathing exercises may help reduce stress levels and promote overall health. Cost: Varies depending on individual preferences and access to classes or resources[46].
- Regular exercise: Engaging in regular physical activity, such as walking, swimming, or cycling, can help maintain a healthy weight and reduce the risk of developing benign breast tumors. Cost: Varies depending on individual preferences and access to exercise facilities or equipment[47].
Lifestyle Interventions
- Maintain a healthy weight: Obesity and excess body fat can increase the risk of developing benign breast tumors. Cost: Varies depending on individual dietary choices and access to healthy food options[48].
- Limit alcohol consumption: Excessive alcohol consumption has been linked to an increased risk of developing benign breast tumors. Cost: Varies depending on individual alcohol consumption habits[49].
- Quit smoking: Smoking has been associated with an increased risk of developing benign breast tumors. Cost: Varies depending on individual smoking cessation methods[50].
- Practice breast self-examinations: Regularly examining the breasts for any changes or abnormalities can help detect benign breast tumors early. Cost: Free[51].
- Attend regular mammogram screenings: Mammograms can help detect benign breast tumors and other breast abnormalities. Cost: Varies depending on insurance coverage and healthcare provider[52].
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – X79 Benign neoplasm breast female (ICD-10:D24)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Benign neoplasm breast female effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Benign neoplasm breast female. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- American Cancer Society. (2023). Fibrosis and simple cysts in the breast. https://www.cancer.org/cancer/breast-cancer/non-cancerous-breast-conditions/fibrosis-and-simple-cysts-in-the-breast.html
- Mayo Clinic. (2023). Breast cysts. https://www.mayoclinic.org/diseases-conditions/breast-cysts/symptoms-causes/syc-20370284
- Risteys. (2023). ICPC-2 Code: X79 Benign neoplasm breast female. https://risteys.finregistry.fi/endpoints/CD2_BENIGN_BREAST
- World Health Organization. (2023). ICD-10 Code: D24 Benign neoplasm of breast. https://icd.who.int/browse10/2019/en#/D24
- National Health Service. (2023). Breast lumps. https://www.nhs.uk/conditions/breast-lump/
- Guray, M., & Sahin, A. A. (2006). Benign breast diseases: classification, diagnosis, and management. The Oncologist, 11(5), 435-449. https://doi.org/10.1634/theoncologist.11-5-435
- Collaborative Group on Hormonal Factors in Breast Cancer. (2019). Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. The Lancet, 394(10204), 1159-1168. https://doi.org/10.1016/S0140-6736(19)31709-X
- Hartmann, L. C., Sellers, T. A., Frost, M. H., Lingle, W. L., Degnim, A. C., Ghosh, K., … & Visscher, D. W. (2005). Benign breast disease and the risk of breast cancer. New England Journal of Medicine, 353(3), 229-237. https://doi.org/10.1056/NEJMoa044383
- Santen, R. J., & Mansel, R. (2005). Benign breast disorders. New England Journal of Medicine, 353(3), 275-285. https://doi.org/10.1056/NEJMra035692
- American College of Obstetricians and Gynecologists. (2021). Benign breast problems and conditions. https://www.acog.org/womens-health/faqs/benign-breast-problems-and-conditions
- Barton, M. B., Harris, R., & Fletcher, S. W. (1999). The rational clinical examination. Does this patient have breast cancer? The screening clinical breast examination: should it be done? How?. JAMA, 282(13), 1270-1280. https://doi.org/10.1001/jama.282.13.1270
- Berg, W. A., Blume, J. D., Cormack, J. B., Mendelson, E. B., Lehrer, D., Böhm-Vélez, M., … & Pisano, E. D. (2008). Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA, 299(18), 2151-2163. https://doi.org/10.1001/jama.299.18.2151
- Pisano, E. D., Gatsonis, C., Hendrick, E., Yaffe, M., Baum, J. K., Acharyya, S., … & Rebner, M. (2005). Diagnostic performance of digital versus film mammography for breast-cancer screening. New England Journal of Medicine, 353(17), 1773-1783. https://doi.org/10.1056/NEJMoa052911
- Bruening, W., Fontanarosa, J., Tipton, K., Treadwell, J. R., Launders, J., & Schoelles, K. (2010). Systematic review: comparative effectiveness of core-needle and open surgical biopsy to diagnose breast lesions. Annals of Internal Medicine, 152(1), 238-246. https://doi.org/10.7326/0003-4819-152-1-201001050-00190
- Warner, E., Plewes, D. B., Hill, K. A., Causer, P. A., Zubovits, J. T., Jong, R. A., … & Narod, S. A. (2004). Surveillance of BRCA1 and BRCA2 mutation carriers with magnetic resonance imaging, ultrasound, mammography, and clinical breast examination. JAMA, 292(11), 1317-1325. https://doi.org/10.1001/jama.292.11.1317
- Lindfors, K. K., Boone, J. M., Nelson, T. R., Yang, K., Kwan, A. L., & Miller, D. F. (2008). Dedicated breast CT: initial clinical experience. Radiology, 246(3), 725-733. https://doi.org/10.1148/radiol.2463070410
- Avril, N., Rosé, C. A., Schelling, M., Dose, J., Kuhn, W., Bense, S., … & Römer, W. (2000). Breast imaging with positron emission tomography and fluorine-18 fluorodeoxyglucose: use and limitations. Journal of Clinical Oncology, 18(20), 3495-3502. https://doi.org/10.1200/JCO.2000.18.20.3495
- Robson, M., & Offit, K. (2007). Clinical practice. Management of an inherited predisposition to breast cancer. New England Journal of Medicine, 357(2), 154-162. https://doi.org/10.1056/NEJMcp071286
- Hammond, M. E. H., Hayes, D. F., Dowsett, M., Allred, D. C., Hagerty, K. L., Badve, S., … & Wolff, A. C. (2010). American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. Journal of Clinical Oncology, 28(16), 2784-2795. https://doi.org/10.1200/JCO.2009.25.6529
- Morrow, M. (2000). The evaluation of common breast problems. American Family Physician, 61(8), 2371-2378. https://www.aafp.org/pubs/afp/issues/2000/0415/p2371.html
- National Institutes of Health. (2023). Tamoxifen. https://www.ncbi.nlm.nih.gov/books/NBK532905/
- GoodRx. (2023). Tamoxifen. https://www.goodrx.com/tamoxifen
- Stearns, V., Johnson, M. D., Rae, J. M., Morocho, A., Novielli, A., Bhargava, P., … & Flockhart, D. A. (2003). Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. Journal of the National Cancer Institute, 95(23), 1758-1764. https://doi.org/10.1093/jnci/djg108
- Drugs.com. (2023). Danazol. https://www.drugs.com/mtm/danazol.html
- GoodRx. (2023). Danazol. https://www.goodrx.com/danazol
- Micromedex. (2023). Danazol. IBM Watson Health.
- MedlinePlus. (2023). Bromocriptine. https://medlineplus.gov/druginfo/meds/a682079.html
- GoodRx. (2023). Bromocriptine. https://www.goodrx.com/bromocriptine
- Drugs.com. (2023). Bromocriptine Drug Interactions. https://www.drugs.com/drug-interactions/bromocriptine.html
- National Cancer Institute. (2023). Raloxifene Hydrochloride. https://www.cancer.gov/about-cancer/treatment/drugs/raloxifenehydrochloride
- GoodRx. (2023). Raloxifene. https://www.goodrx.com/raloxifene
- Micromedex. (2023). Raloxifene. IBM Watson Health.
- National Institutes of Health. (2023). Aromatase Inhibitors. https://www.ncbi.nlm.nih.gov/books/NBK557856/
- GoodRx. (2023). Anastrozole. https://www.goodrx.com/anastrozole
- Micromedex. (2023). Anastrozole. IBM Watson Health.
- Lee, A. J., Cai, M. X., Thomas, P. E., Conney, A. H., & Zhu, B. T. (2003). Characterization of the oxidative metabolites of 17β-estradiol and estrone formed by 15 selectively expressed human cytochrome P450 isoforms. Endocrinology, 144(8), 3382-3398. https://doi.org/10.1210/en.2003-0192
- Pruthi, S., Wahner-Roedler, D. L., Torkelson, C. J., Cha, S. S., Thicke, L. S., Hazelton, J. H., & Bauer, B. A. (2010). Vitamin E and evening primrose oil for management of cyclical mastalgia: a randomized pilot study. Alternative Medicine Review, 15(1), 59-67. https://pubmed.ncbi.nlm.nih.gov/20359269/
- Guo, Y., Zhi, F., Chen, P., Zhao, K., Xiang, H., Mao, Q., … & Zhang, X. (2017). Green tea and the risk of prostate cancer: A systematic review and meta-analysis. Medicine, 96(13), e6426. https://doi.org/10.1097/MD.0000000000006426
- Banik, U., Parasuraman, S., Adhikary, A. K., & Othman, N. H. (2017). Curcumin: the spicy modulator of breast carcinogenesis. Journal of Experimental & Clinical Cancer Research, 36(1), 98. https://doi.org/10.1186/s13046-017-0566-5
- Thomson, C. A., Chow, H. H. S., Wertheim, B. C., Roe, D. J., Stopeck, A., Maskarinec, G., … & Alberts, D. S. (2017). A randomized, placebo-controlled trial of diindolylmethane for breast cancer biomarker modulation in patients taking tamoxifen. Breast Cancer Research and Treatment, 165(1), 97-107. https://doi.org/10.1007/s10549-017-4292-7
- American Cancer Society. (2023). Surgery for Breast Cancer. https://www.cancer.org/cancer/breast-cancer/treatment/surgery-for-breast-cancer.html
- American Society of Plastic Surgeons. (2023). Breast Reconstruction. https://www.plasticsurgery.org/reconstructive-procedures/breast-reconstruction
- Chien, T. J., Liu, C. Y., & Fang, C. J. (2019). The effect of acupuncture in breast cancer-related lymphoedema (BCRL): A systematic review and meta-analysis. Integrative Cancer Therapies, 18, 1534735419866910. https://doi.org/10.1177/1534735419866910
- Fritz, H., Seely, D., McGowan, J., Skidmore, B., Fernandes, R., Kennedy, D. A., … & Fergusson, D. (2014). Black cohosh and breast cancer: a systematic review. Integrative Cancer Therapies, 13(1), 12-29. https://doi.org/10.1177/1534735413477191
- World Cancer Research Fund/American Institute for Cancer Research. (2018). Diet, Nutrition, Physical Activity and Cancer: a Global Perspective. Continuous Update Project Expert Report 2018. https://www.wcrf.org/diet-and-cancer/
- Cramer, H., Lauche, R., Klose, P., Lange, S., Langhorst, J., & Dobos, G. J. (2017). Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database of Systematic Reviews, 1(1), CD010802. https://doi.org/10.1002/14651858.CD010802.pub2
- Colditz, G. A., Bohlke, K., & Berkey, C. S. (2014). Breast cancer risk accumulation starts early: prevention must also. Breast Cancer Research and Treatment, 145(3), 567-579. https://doi.org/10.1007/s10549-014-2993-8
- Neuhouser, M. L., Aragaki, A. K., Prentice, R. L., Manson, J. E., Chlebowski, R., Carty, C. L., … & Anderson, G. L. (2015). Overweight, obesity, and postmenopausal invasive breast cancer risk: a secondary analysis of the Women’s Health Initiative randomized clinical trials. JAMA Oncology, 1(5), 611-621. https://doi.org/10.1001/jamaoncol.2015.1546
- Chen, W. Y., Rosner, B., Hankinson, S. E., Colditz, G. A., & Willett, W. C. (2011). Moderate alcohol consumption during adult life, drinking patterns, and breast cancer risk. JAMA, 306(17), 1884-1890. https://doi.org/10.1001/jama.2011.1590
- Gaudet, M. M., Gapstur, S. M., Sun, J., Diver, W. R., Hannan, L. M., & Thun, M. J. (2013). Active smoking and breast cancer risk: original cohort data and meta-analysis. Journal of the National Cancer Institute, 105(8), 515-525. https://doi.org/10.1093/jnci/djt023
- American Cancer Society. (2023). Breast Cancer Early Detection and Diagnosis. https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection.html
- U.S. Preventive Services Task Force. (2016). Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine, 164(4), 279-296. https://doi.org/10.7326/M15-2886
Related articles
Made in USA