Introduction
Fear of sexually transmitted diseases (STDs) is a common concern among individuals who engage in sexual activity. This fear can stem from various factors, including lack of knowledge about STDs, misconceptions, or personal experiences[1]. It is important to address this fear and provide appropriate education and support to individuals to alleviate their concerns. This guide aims to provide a comprehensive approach to diagnosing and managing fear of STDs.
Codes
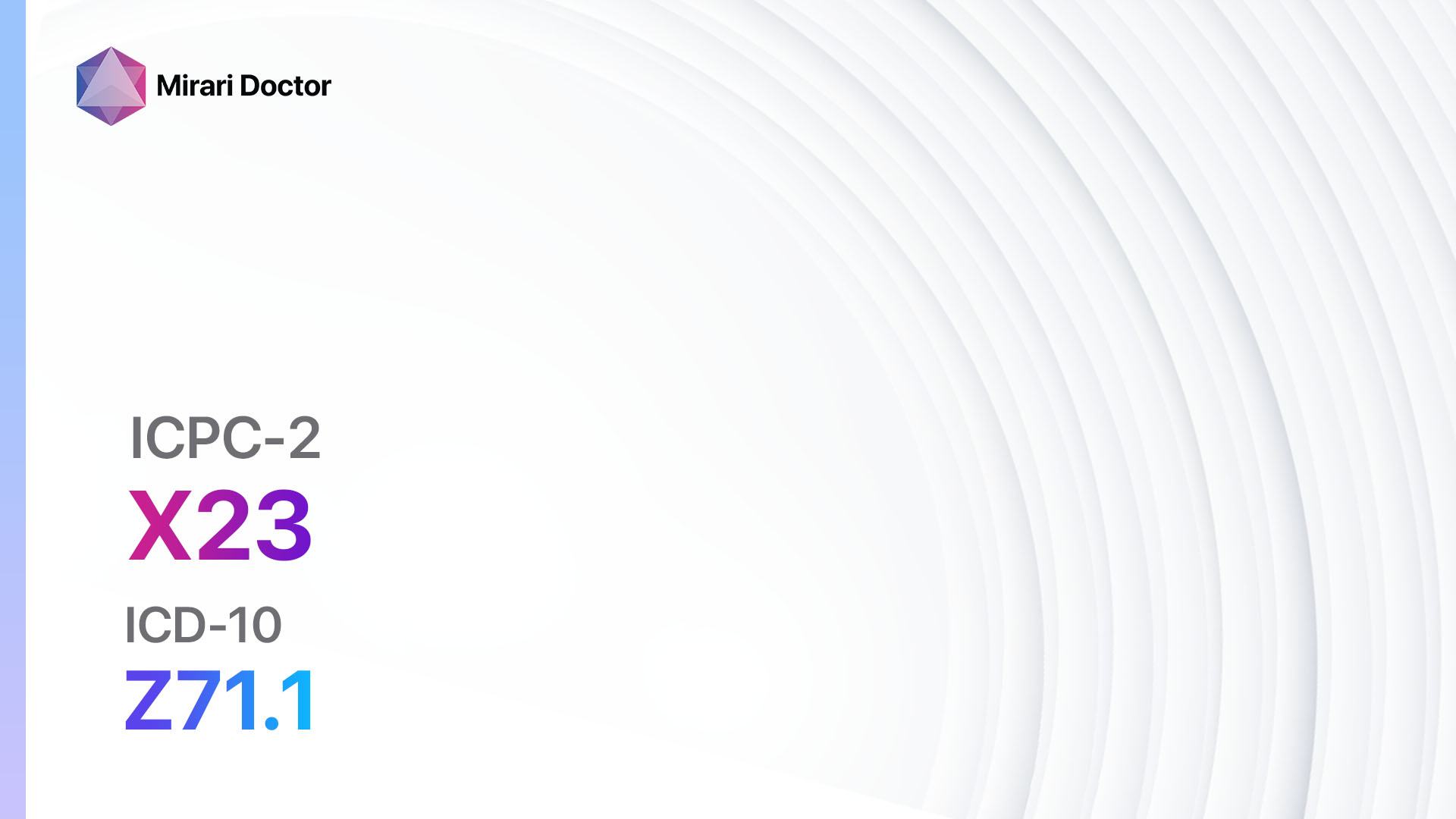
- ICPC-2 Code: X23 Fear sexually transmitted disease female
- ICD-10 Code: Z71.1 Person with feared complaint in whom no diagnosis is made
Symptoms
- Excessive worry or anxiety about contracting an STD
- Fear of engaging in sexual activity due to concerns about STD transmission
- Avoidance of sexual relationships or intimacy due to fear of STDs[2]
Causes
- Lack of knowledge or misinformation about STDs
- Previous personal experiences or encounters with STDs
- Cultural or societal beliefs and stigmas surrounding STDs
- Media portrayal of STDs and their consequences[3]
Diagnostic Steps
Medical History
- Conduct a thorough medical history to gather relevant information about the patient’s sexual activity, past experiences with STDs, and any risk factors for contracting STDs.
- Inquire about the patient’s knowledge and understanding of STDs to identify any misconceptions or gaps in knowledge.
- Assess the patient’s psychological well-being and any underlying anxiety or fear related to sexual activity and STDs[4].
Physical Examination
- Perform a physical examination to assess for any physical signs or symptoms of STDs, such as genital lesions, discharge, or inflammation.
- Evaluate the patient’s overall health and well-being to identify any underlying conditions or factors that may contribute to their fear of STDs[5].
Laboratory Tests
- Consider performing laboratory tests to rule out any existing STDs and provide reassurance to the patient.
- Common laboratory tests for STDs include:
- Blood tests for HIV, syphilis, and hepatitis B and C
- Urine tests for chlamydia and gonorrhea
- Swab tests for herpes and other genital infections[6]
Diagnostic Imaging
- Diagnostic imaging is not typically necessary for diagnosing fear of STDs. However, if the patient presents with physical symptoms suggestive of an STD, imaging modalities such as ultrasound or MRI may be used to visualize and assess the extent of any associated complications[7].
Other Tests
- In some cases, additional tests may be necessary based on the patient’s clinical presentation and specific concerns. These may include:
- Pap smear for cervical cancer screening
- HPV DNA testing for high-risk HPV strains
- Serologic tests for specific STDs, such as syphilis or herpes[8]
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the patient’s progress and address any ongoing concerns or questions.
- Provide comprehensive patient education about STDs, including transmission routes, prevention methods, and available treatment options.
- Offer counseling or referral to mental health professionals if necessary to address any underlying anxiety or fear related to STDs[9][10].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Fear of STDs:
- Selective Serotonin Reuptake Inhibitors (SSRIs) (e.g., Fluoxetine, Sertraline):
- Cost: Generic versions can be $3-$50/month.
- Contraindications: Hypersensitivity to SSRIs, concurrent use of MAO inhibitors.
- Side effects: Nausea, headache, sexual dysfunction.
- Severe side effects: Serotonin syndrome, suicidal thoughts.
- Drug interactions: MAO inhibitors, NSAIDs, other serotonergic drugs.
- Warning: May take several weeks to achieve full therapeutic effect.
- Benzodiazepines (e.g., Alprazolam, Lorazepam):
- Cost: Generic versions can be $4-$50/month.
- Contraindications: Acute narrow-angle glaucoma, concurrent use of opioids.
- Side effects: Drowsiness, dizziness, confusion.
- Severe side effects: Respiratory depression, dependence.
- Drug interactions: Opioids, alcohol, other CNS depressants.
- Warning: Risk of dependence and withdrawal symptoms with long-term use.
- Beta-blockers (e.g., Propranolol, Atenolol):
- Cost: Generic versions can be $4-$30/month.
- Contraindications: Severe bradycardia, heart block, uncontrolled heart failure.
- Side effects: Fatigue, dizziness, bradycardia.
- Severe side effects: Bronchospasm, heart block.
- Drug interactions: Calcium channel blockers, insulin.
- Warning: Should not be abruptly stopped.
- Cognitive-Behavioral Therapy (CBT):
- Cost: Varies depending on the therapist and location. Typically ranges from $80-$200 per session.
- Contraindications: None.
- Side effects: None.
- Severe side effects: None.
- Drug interactions: None.
- Warning: Requires commitment and active participation from the patient.
- Group Therapy:
- Cost: Varies depending on the therapist and location. Typically ranges from $40-$100 per session.
- Contraindications: None.
- Side effects: None.
- Severe side effects: None.
- Drug interactions: None.
- Warning: Requires willingness to participate in a group setting.
Alternative Drugs:
- Antidepressants (e.g., Bupropion, Mirtazapine): Alternative options for individuals who do not respond to SSRIs or prefer non-SSRI medications.
- Anxiolytics (e.g., Buspirone, Hydroxyzine): Alternative options for individuals who do not respond to or cannot tolerate benzodiazepines.
Surgical Procedures:
- Surgical procedures are not typically indicated for the treatment of fear of STDs. However, in cases where fear of STDs is associated with physical symptoms or complications, surgical interventions may be necessary. These would be specific to the underlying condition and would require consultation with a specialist.
Alternative Interventions
- Counseling and Therapy: Various forms of therapy, such as cognitive-behavioral therapy (CBT), exposure therapy, or psychoeducation, can help individuals address and manage their fear of STDs. Cost: Varies depending on the therapist and location. Typically ranges from $80-$200 per session.
- Support Groups: Joining support groups or online communities can provide individuals with a safe space to share their concerns, experiences, and coping strategies. Cost: Varies depending on the group or platform. Some may be free, while others may require a membership fee.
- Education and Information: Providing individuals with accurate and comprehensive information about STDs, transmission routes, prevention methods, and available treatments can help alleviate their fears and empower them to make informed decisions. Cost: Varies depending on the source of information. Many reliable resources are available online for free.
- Mindfulness and Relaxation Techniques: Practicing mindfulness, deep breathing exercises, or other relaxation techniques can help individuals manage anxiety and reduce fear related to STDs. Cost: Free or minimal cost for instructional materials or classes.
- Sexual Health Education Programs: Participating in sexual health education programs or workshops can enhance individuals’ knowledge and understanding of STDs, reducing fear and promoting healthy sexual behaviors. Cost: Varies depending on the program or workshop. Some may be free, while others may require a fee for enrollment.
Lifestyle Interventions
- Safer Sex Practices: Encouraging individuals to practice safer sex, such as using condoms consistently and correctly, can help reduce the risk of contracting STDs and alleviate fear. Cost: Varies depending on the cost of condoms or other barrier methods.
- Regular STD Testing: Regularly getting tested for STDs can provide individuals with reassurance about their sexual health status and help detect any infections early. Cost: Varies depending on the testing facility and type of tests performed. Some clinics offer free or low-cost testing.
- Open Communication: Promoting open and honest communication about sexual health and STDs with sexual partners can help alleviate fear and build trust. Cost: Free.
- Healthy Lifestyle Choices: Encouraging individuals to maintain a healthy lifestyle, including regular exercise, a balanced diet, and adequate sleep, can support overall well-being and reduce anxiety related to STDs. Cost: Varies depending on personal choices and preferences.
- Avoidance of High-Risk Behaviors: Educating individuals about high-risk sexual behaviors, such as unprotected sex or multiple sexual partners, and promoting abstinence or monogamy can help reduce the risk of contracting STDs and alleviate fear. Cost: Free.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. Additionally, the choice of interventions should be tailored to the individual’s specific needs and preferences, and consultation with a healthcare professional is recommended for personalized guidance.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – X23 Fear sexually transmitted disease female (ICD-10:Z71.1)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Fear sexually transmitted disease (f) effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Fear sexually transmitted disease (f). If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Centers for Disease Control and Prevention. (2021). Sexually Transmitted Diseases (STDs). Retrieved from https://www.cdc.gov/std/
- American Sexual Health Association. (n.d.). STDs/STIs. Retrieved from https://www.ashasexualhealth.org/stdsstis/
- World Health Organization. (2019). Sexually transmitted infections (STIs). Retrieved from https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)
- Planned Parenthood. (n.d.). STDs. Retrieved from https://www.plannedparenthood.org/learn/stds-hiv-safer-sex
- Mayo Clinic. (2021). Sexually transmitted diseases (STDs). Retrieved from https://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/symptoms-causes/syc-20351240
- National Institutes of Health. (2020). Sexually Transmitted Diseases. Retrieved from https://www.niaid.nih.gov/diseases-conditions/sexually-transmitted-diseases
- American College of Obstetricians and Gynecologists. (2021). Sexually Transmitted Infections (STIs). Retrieved from https://www.acog.org/womens-health/faqs/sexually-transmitted-infections
- U.S. Department of Health & Human Services. (n.d.). Sexually Transmitted Diseases. Retrieved from https://www.hhs.gov/programs/topic-sites/sexually-transmitted-diseases/index.html
- National Health Service. (2021). Sexually transmitted infections (STIs). Retrieved from https://www.nhs.uk/conditions/sexually-transmitted-infections-stis/
- American Academy of Family Physicians. (2020). Sexually Transmitted Infections. Retrieved from https://familydoctor.org/condition/sexually-transmitted-infections-stis/
Related articles
Made in USA