Introduction
Menopause is a natural biological process that marks the end of a woman’s reproductive years. It is characterized by the cessation of menstrual periods and a decline in hormone production, particularly estrogen[1]. Menopausal symptoms can vary widely among women, with some experiencing mild symptoms and others experiencing more severe symptoms that significantly impact their quality of life[2]. The aim of this guide is to provide an overview of menopausal symptoms, potential causes, diagnostic steps, and possible interventions to help manage and alleviate these symptoms.
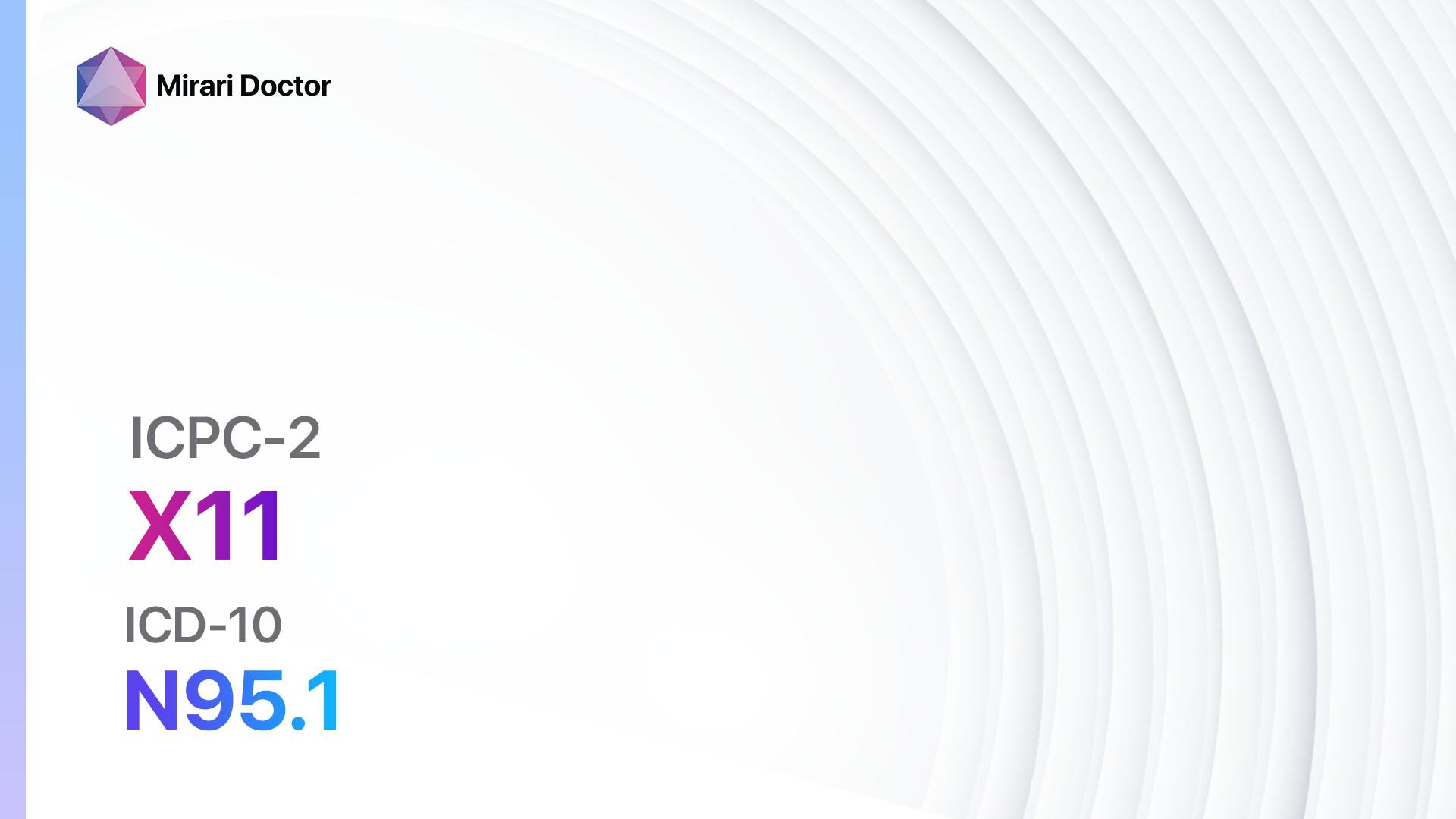
Codes
- ICPC-2 Code: X11 Menopausal symptom/complaint
- ICD-10 Code: N95.1 Menopausal and female climacteric states
Symptoms
- Hot flashes: Sudden feelings of warmth, often accompanied by flushing and sweating.
- Night sweats: Excessive sweating during sleep.
- Vaginal dryness: Thinning and inflammation of the vaginal walls, leading to discomfort during intercourse.
- Sleep disturbances: Insomnia or disrupted sleep patterns.
- Mood changes: Mood swings, irritability, and feelings of depression or anxiety.
- Fatigue: Persistent tiredness and lack of energy.
- Urinary problems: Increased frequency of urination or urinary incontinence.
- Joint and muscle pain: Aches and pains in the joints and muscles.
- Changes in sexual function: Decreased libido and difficulty achieving orgasm[3][4].
Causes
- Natural decline in hormone production: As women age, their ovaries produce less estrogen and progesterone, leading to menopausal symptoms.
- Surgical menopause: Menopause can occur abruptly if the ovaries are surgically removed.
- Chemotherapy or radiation therapy: These treatments can induce menopause in women of any age.
- Primary ovarian insufficiency: Some women experience menopause before the age of 40 due to the loss of ovarian function[5].
Diagnostic Steps
Medical History
- Gather information about the patient’s age, menstrual history, and any previous surgeries or medical treatments that may have induced menopause.
- Assess the severity and duration of menopausal symptoms.
- Identify any risk factors for complications associated with menopause, such as cardiovascular disease or osteoporosis.
- Evaluate the patient’s overall health and any pre-existing medical conditions that may influence treatment options[6].
Physical Examination
- Perform a general physical examination to assess overall health and identify any signs of underlying medical conditions.
- Evaluate the patient’s blood pressure, heart rate, and body mass index (BMI).
- Assess the health of the breasts and pelvic organs.
- Check for signs of osteoporosis, such as loss of height or kyphosis (hunchback)[7].
Laboratory Tests
- Follicle-stimulating hormone (FSH) level: Elevated FSH levels are indicative of menopause.
- Estradiol level: Low levels of estradiol support the diagnosis of menopause.
- Thyroid-stimulating hormone (TSH) level: Thyroid dysfunction can mimic menopausal symptoms, so it is important to rule out thyroid disorders.
- Lipid profile: Assessing cholesterol levels can help identify women at risk for cardiovascular disease.
- Bone density test: Dual-energy X-ray absorptiometry (DXA) scan can assess bone density and diagnose osteoporosis[8].
Diagnostic Imaging
- Transvaginal ultrasound: This imaging technique can evaluate the thickness of the endometrial lining and rule out other causes of abnormal bleeding.
- Mammogram: Recommended for women over the age of 50 to screen for breast cancer[9].
Other Tests
- Endometrial biopsy: If abnormal bleeding is present, an endometrial biopsy may be performed to rule out endometrial cancer.
- Genetic testing: In cases of premature menopause, genetic testing may be recommended to identify any underlying genetic causes[10].
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor symptoms and adjust treatment as needed.
- Provide education on lifestyle modifications, potential interventions, and the importance of regular health screenings.
- Encourage open communication and address any concerns or questions the patient may have[1][2].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Menopausal symptoms:
- Hormone replacement therapy (HRT):
- Cost: Varies depending on the specific formulation and insurance coverage.
- Contraindications: History of breast cancer, blood clots, or liver disease.
- Side effects: Breast tenderness, bloating, mood changes.
- Severe side effects: Increased risk of breast cancer, blood clots, stroke.
- Drug interactions: Certain medications may interact with HRT, so it is important to review the patient’s current medications.
- Warning: Long-term use of HRT may increase the risk of certain health conditions.
- Selective serotonin reuptake inhibitors (SSRIs):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Concurrent use of monoamine oxidase inhibitors (MAOIs).
- Side effects: Nausea, headache, sexual dysfunction.
- Severe side effects: Serotonin syndrome (rare).
- Drug interactions: MAOIs, other medications that increase serotonin levels.
- Warning: SSRIs may take several weeks to reach their full effect.
- Gabapentin:
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to gabapentin.
- Side effects: Dizziness, drowsiness, peripheral edema.
- Severe side effects: Suicidal thoughts (rare).
- Drug interactions: None of significant concern.
- Warning: Gabapentin may cause drowsiness or dizziness, so caution should be exercised when driving or operating machinery.
- Clonidine:
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to clonidine.
- Side effects: Dry mouth, drowsiness, constipation.
- Severe side effects: Hypotension, bradycardia.
- Drug interactions: None of significant concern.
- Warning: Clonidine should be tapered off gradually to avoid rebound hypertension.
- Ospemifene:
- Cost: Approximately $200-$300/month.
- Contraindications: History of estrogen-dependent cancer, unexplained vaginal bleeding.
- Side effects: Hot flashes, vaginal discharge, muscle spasms.
- Severe side effects: Increased risk of endometrial cancer, stroke.
- Drug interactions: CYP3A4 inhibitors, tamoxifen.
- Warning: Ospemifene may increase the risk of blood clots.
Alternative Drugs:
- Black cohosh: An herbal supplement that may help alleviate menopausal symptoms. Cost: $10-$30/month.
- Soy isoflavones: Plant-based compounds that have estrogen-like effects. Cost: $10-$30/month.
- Dong quai: An herb used in traditional Chinese medicine for menopausal symptoms. Cost: $10-$30/month.
- Evening primrose oil: An herbal supplement that may help with hot flashes and mood swings. Cost: $10-$30/month.
- Red clover: Another herbal supplement that may help reduce hot flashes. Cost: $10-$30/month.
Surgical Procedures:
- Hysterectomy: Surgical removal of the uterus. Cost: $10,000 to $20,000.
- Oophorectomy: Surgical removal of the ovaries. Cost: $10,000 to $20,000.
Lifestyle Interventions
- Regular exercise: Engaging in physical activity can help reduce menopausal symptoms, improve mood, and promote overall health. Cost: Varies depending on the chosen activity (e.g., gym membership, fitness classes).
- Healthy diet: Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health and alleviate menopausal symptoms. Cost: Varies depending on food choices and dietary preferences.
- Stress management techniques: Practicing relaxation techniques, such as deep breathing exercises, meditation, or yoga, can help reduce stress and improve overall well-being. Cost: Varies depending on the chosen technique (e.g., yoga classes, meditation apps).
- Adequate sleep: Establishing a regular sleep routine and creating a conducive sleep environment can help improve sleep quality and reduce sleep disturbances. Cost: Varies depending on the chosen sleep aids or interventions (e.g., comfortable bedding, sleep masks).
- Smoking cessation: Quitting smoking can improve overall health and reduce the risk of menopausal symptoms, such as hot flashes. Cost: Varies depending on the chosen smoking cessation method (e.g., nicotine replacement therapy, counseling).
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. It is recommended to consult with a healthcare professional for personalized advice and guidance regarding menopausal symptom management.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – X11 Menopausal symptom/complaint (ICD-10:N95.1)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Menopausal symptom/complaint effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Menopausal symptom/complaint. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Mayo Clinic. (2023). Menopause – Symptoms and causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/menopause/symptoms-causes/syc-20353397
- American College of Obstetricians and Gynecologists. (2023). The Menopause Years. Retrieved from https://www.acog.org/womens-health/faqs/the-menopause-years
- National Institute on Aging. (2023). What Is Menopause? Retrieved from https://www.nia.nih.gov/health/menopause/what-menopause
- InformedHealth.org. (2020). Overview: Menopause. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279311/
- Mayo Clinic. (2023). Perimenopause – Diagnosis and treatment. Retrieved from https://www.mayoclinic.org/diseases-conditions/perimenopause/diagnosis-treatment/drc-20354671
- American College of Obstetricians and Gynecologists. (2014). Management of Menopausal Symptoms. Retrieved from https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2014/01/management-of-menopausal-symptoms
- Mayo Clinic. (2023). Menopause – Diagnosis and treatment. Retrieved from https://www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401
- American College of Obstetricians and Gynecologists. (2023). Hormone Therapy for Menopause. Retrieved from https://www.acog.org/womens-health/faqs/hormone-therapy-for-menopause
- National Institute of Child Health and Human Development. (2023). Menopause. Retrieved from https://www.nichd.nih.gov/health/topics/menopause
- American College of Obstetricians and Gynecologists. (2023). ACOG Explains: Managing Menopause Symptoms. Retrieved from https://www.acog
Related articles
Made in USA