Introduction
Menstrual pain, also known as dysmenorrhea, is a common condition experienced by women during their menstrual cycle. It is characterized by cramping pain in the lower abdomen, which can range from mild to severe[1]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of menstrual pain.
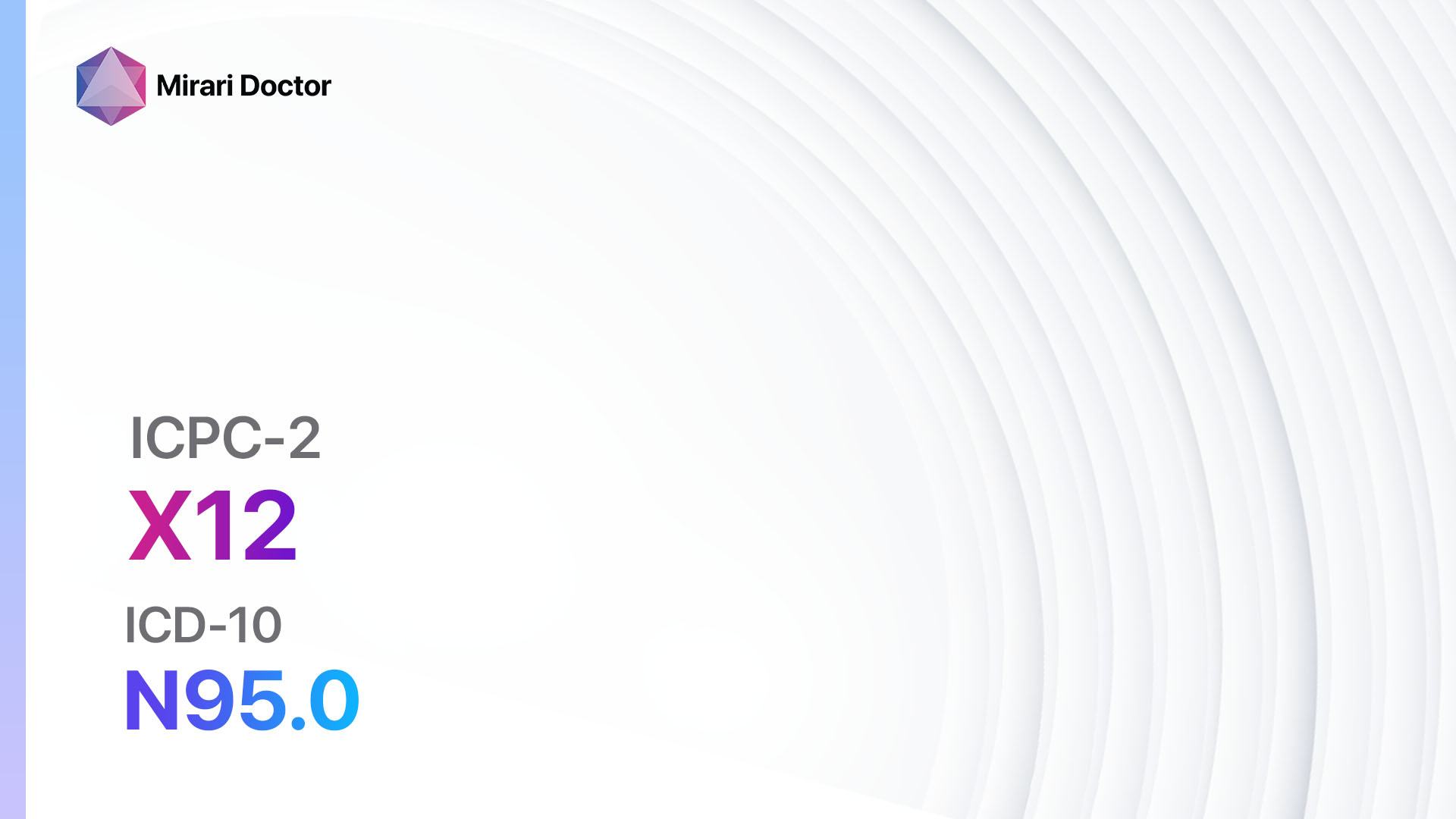
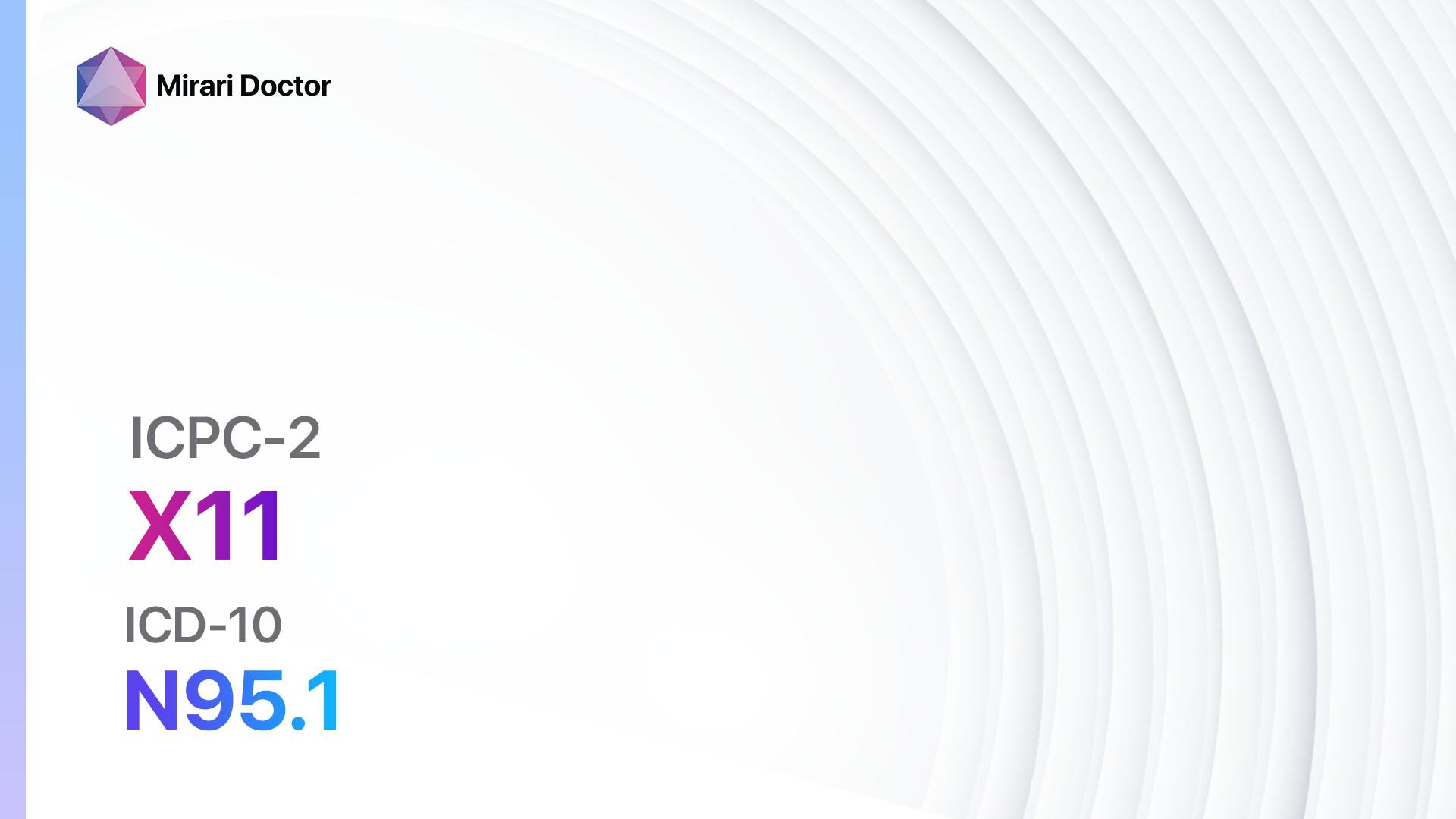
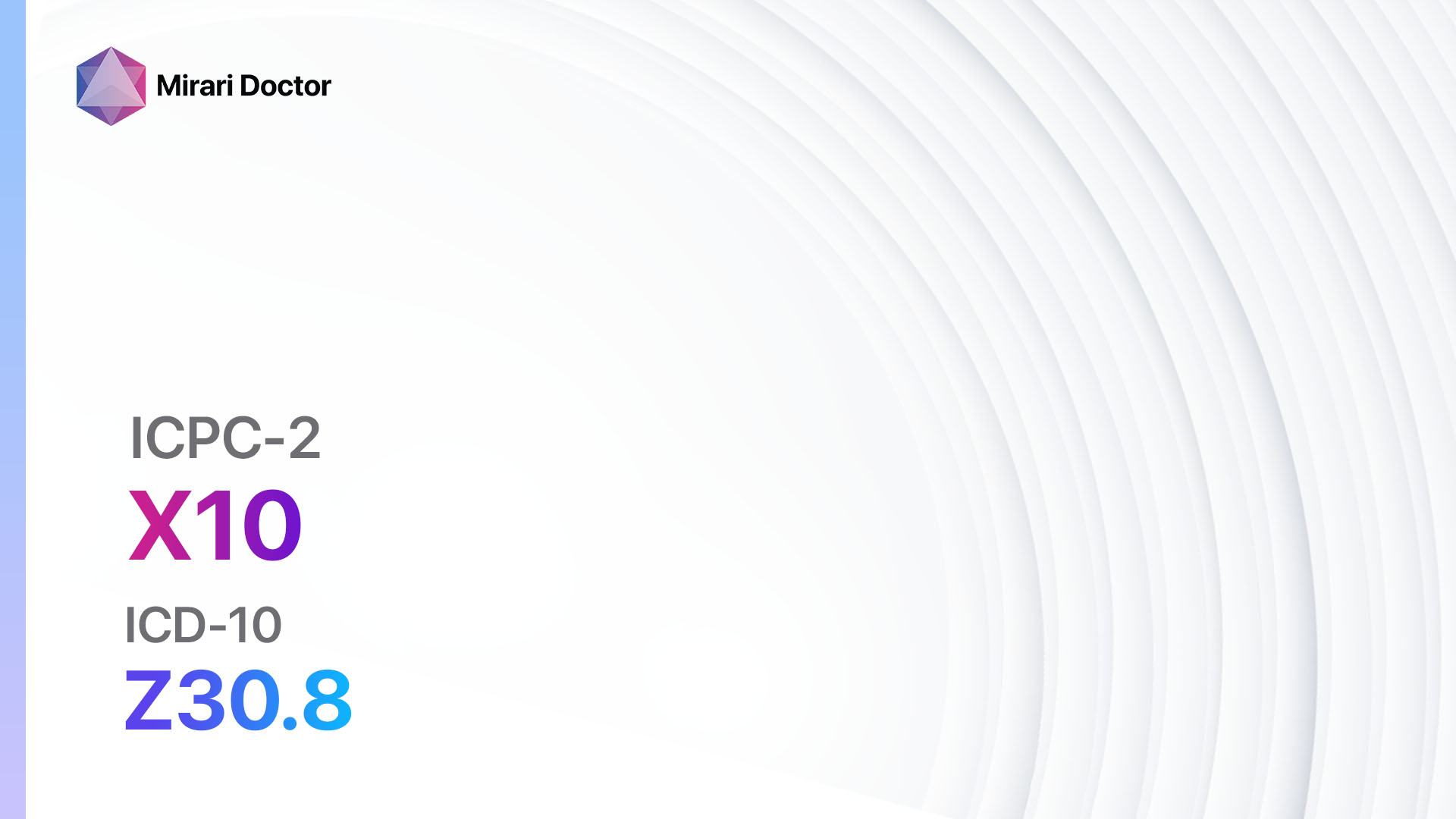
Codes
Symptoms
- Abdominal cramping: Women with menstrual pain often experience cramping pain in the lower abdomen.
- Back pain: Some women may also experience lower back pain during their menstrual cycle.
- Headaches: Headaches and migraines can be associated with menstrual pain.
- Nausea and vomiting: Some women may experience nausea and vomiting during their menstrual cycle.
- Fatigue: Fatigue and tiredness are common symptoms of menstrual pain[4].
Causes
- Prostaglandins: Increased levels of prostaglandins, hormone-like substances, can cause the uterus to contract, leading to menstrual pain.
- Hormonal imbalances: Imbalances in estrogen and progesterone levels can contribute to menstrual pain.
- Endometriosis: In some cases, menstrual pain may be caused by endometriosis, a condition where the tissue lining the uterus grows outside of it.
- Adenomyosis: Adenomyosis, a condition where the tissue lining the uterus grows into the muscular wall of the uterus, can also cause menstrual pain.
- Fibroids: Uterine fibroids, noncancerous growths in the uterus, can cause menstrual pain[5].
Diagnostic Steps
Medical History
- Gather information about the patient’s menstrual cycle, including the duration, regularity, and severity of menstrual pain.
- Ask about any associated symptoms, such as back pain, headaches, or nausea.
- Inquire about any previous diagnoses of conditions such as endometriosis or adenomyosis.
- Assess the impact of menstrual pain on the patient’s daily activities and quality of life[6].
Physical Examination
- Perform a pelvic examination to assess the size, shape, and position of the uterus.
- Check for any abnormalities, such as masses or tenderness, in the pelvic region.
- Evaluate the patient’s vital signs, including blood pressure and heart rate[7].
Laboratory Tests
- Complete blood count (CBC): A CBC can help identify any underlying infections or anemia.
- Urinalysis: A urinalysis can rule out urinary tract infections or other urinary abnormalities.
- Hormone levels: Measuring hormone levels, such as estrogen and progesterone, can help identify hormonal imbalances.
- Imaging studies: In some cases, imaging studies such as ultrasound or MRI may be necessary to evaluate the uterus and surrounding structures[8].
Other Tests
- Laparoscopy: If endometriosis or adenomyosis is suspected, a laparoscopy may be performed to visualize the pelvic organs and obtain tissue samples for further evaluation.
- Endometrial biopsy: An endometrial biopsy may be recommended to rule out other causes of menstrual pain, such as uterine cancer[9].
Follow-up and Patient Education
- Schedule a follow-up appointment to review the results of diagnostic tests and discuss treatment options.
- Provide the patient with educational materials about menstrual pain, including lifestyle modifications and self-care measures[10].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Menstrual pain:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., Ibuprofen, Naproxen):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: History of gastrointestinal bleeding, kidney disease.
- Side effects: Upset stomach, heartburn.
- Severe side effects: Stomach ulcers, kidney damage.
- Drug interactions: Blood thinners, certain antidepressants.
- Warning: Long-term use can increase the risk of cardiovascular events.
- Combined oral contraceptives:
- Cost: $20-$50/month.
- Contraindications: History of blood clots, certain types of cancer.
- Side effects: Nausea, breast tenderness.
- Severe side effects: Blood clots, stroke.
- Drug interactions: Certain antibiotics, anticonvulsants.
- Warning: Increased risk of cardiovascular events in smokers.
- Prostaglandin inhibitors (e.g., Mefenamic acid):
- Cost: $10-$30/month.
- Contraindications: Active peptic ulcer disease, severe liver disease.
- Side effects: Upset stomach, diarrhea.
- Severe side effects: Stomach bleeding, liver damage.
- Drug interactions: Blood thinners, certain antidepressants.
- Warning: May increase the risk of cardiovascular events.
- Antispasmodics (e.g., Hyoscine butylbromide):
- Cost: $10-$30/month.
- Contraindications: Glaucoma, myasthenia gravis.
- Side effects: Dry mouth, blurred vision.
- Severe side effects: Allergic reactions, difficulty urinating.
- Drug interactions: Other anticholinergic drugs.
- Warning: May cause drowsiness.
- Selective serotonin reuptake inhibitors (SSRIs) (e.g., Fluoxetine, Sertraline):
- Cost: $10-$50/month.
- Contraindications: Use of monoamine oxidase inhibitors (MAOIs), history of bipolar disorder.
- Side effects: Nausea, headache.
- Severe side effects: Serotonin syndrome, suicidal thoughts.
- Drug interactions: MAOIs, other antidepressants.
- Warning: May take several weeks to achieve full effect.
Alternative Drugs:
- Acetaminophen: Can be used as an alternative to NSAIDs for pain relief.
- Tranexamic acid: Reduces heavy menstrual bleeding and associated pain.
- Levonorgestrel intrauterine system: Provides long-term relief from menstrual pain and reduces menstrual bleeding.
- Gonadotropin-releasing hormone agonists: Suppresses ovarian function and reduces menstrual pain in severe cases.
- Danazol: A synthetic hormone that suppresses ovulation and reduces menstrual pain.
Surgical Procedures:
- Laparoscopic surgery: If endometriosis or adenomyosis is diagnosed, laparoscopic surgery may be performed to remove abnormal tissue and alleviate menstrual pain.
- Hysterectomy: In severe cases where other treatments have failed, a hysterectomy may be considered as a last resort to eliminate menstrual pain.
Alternative Interventions
- Heat therapy: Applying a heating pad or hot water bottle to the lower abdomen can help relieve menstrual pain. Cost: $10-$30.
- Exercise: Regular exercise, such as walking or yoga, can help reduce menstrual pain. Cost: Varies depending on the chosen activity.
- Relaxation techniques: Techniques such as deep breathing, meditation, or guided imagery can help manage pain and reduce stress. Cost: Free or minimal cost.
- Herbal supplements: Some herbal supplements, such as ginger or chamomile, may have anti-inflammatory properties and can help alleviate menstrual pain. Cost: Varies depending on the specific supplement.
- Acupuncture: Acupuncture may help reduce pain and improve blood flow. Cost: $60-$120 per session.
Lifestyle Interventions
- Healthy diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce inflammation and alleviate menstrual pain. Cost: Varies depending on food choices.
- Stress management: Engaging in stress-reducing activities, such as yoga, meditation, or deep breathing exercises, can help manage menstrual pain. Cost: Free or minimal cost.
- Adequate rest: Getting enough sleep and rest during the menstrual cycle can help reduce fatigue and alleviate pain. Cost: Free.
- Avoiding triggers: Avoiding triggers such as caffeine, alcohol, and smoking can help reduce menstrual pain. Cost: Varies depending on individual habits.
- Regular exercise: Engaging in regular physical activity can help reduce menstrual pain and improve overall well-being. Cost: Varies depending on the chosen activity.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – X02 Menstrual pain (ICD-10:N94.6)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Menstrual pain effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Menstrual pain. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- American College of Obstetricians and Gynecologists. (2015). Dysmenorrhea: Painful Periods. Retrieved from https://www.acog.org/womens-health/faqs/dysmenorrhea-painful-periods
- WONCA International Classification Committee. (2005). ICPC-2: International Classification of Primary Care. Oxford University Press.
- World Health Organization. (2019). ICD-10: International Statistical Classification of Diseases and Related Health Problems, 10th Revision.
- Ju, H., Jones, M., & Mishra, G. (2014). The prevalence and risk factors of dysmenorrhea. Epidemiologic Reviews, 36(1), 104-113.
- Iacovides, S., Avidon, I., & Baker, F. C. (2015). What we know about primary dysmenorrhea today: a critical review. Human Reproduction Update, 21(6), 762-778.
- Burnett, M., & Lemyre, M. (2017). No. 345-Primary Dysmenorrhea Consensus Guideline. Journal of Obstetrics and Gynaecology Canada, 39(7), 585-595.
- Osayande, A. S., & Mehulic, S. (2014). Diagnosis and initial management of dysmenorrhea. American Family Physician, 89(5), 341-346.
- Hsu, A. L., Khachikyan, I., & Stratton, P. (2010). Invasive and noninvasive methods for the diagnosis of endometriosis. Clinical Obstetrics and Gynecology, 53(2), 413-419.
- Banikarim, C., Chacko, M. R., & Kelder, S. H. (2000). Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Archives of Pediatrics & Adolescent Medicine, 154(12), 1226-1229.
- Proctor, M., & Farquhar, C. (2006). Diagnosis and management of dysmenorrhoea. BMJ, 332(7550), 1134-1138.
Related articles
Made in USA