Introduction
Urinary retention is a condition characterized by the inability to empty the bladder completely. It can be caused by various factors, including nerve dysfunction, obstruction, or medication side effects[1]. This guide aims to provide a comprehensive overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for urinary retention.
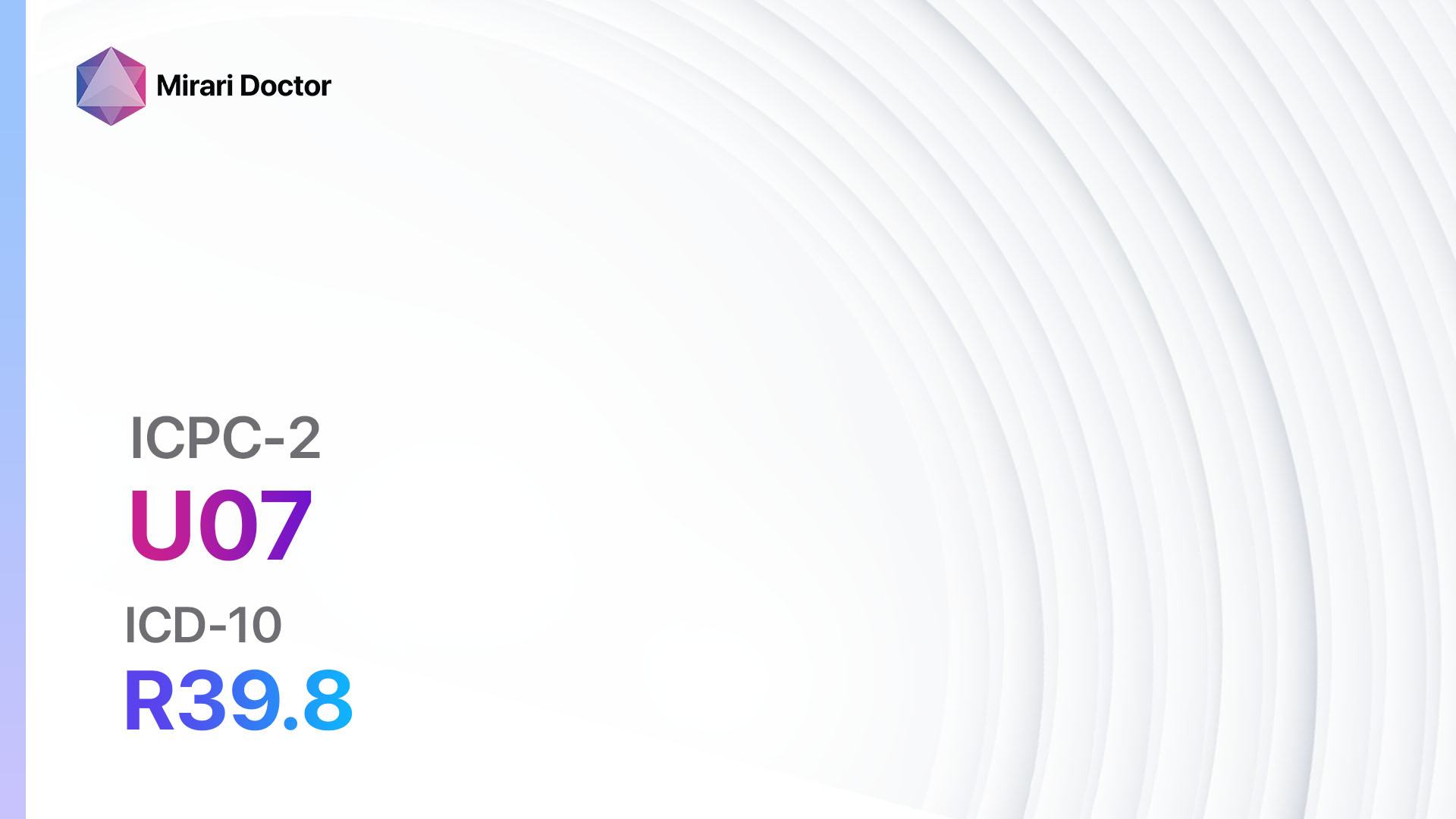
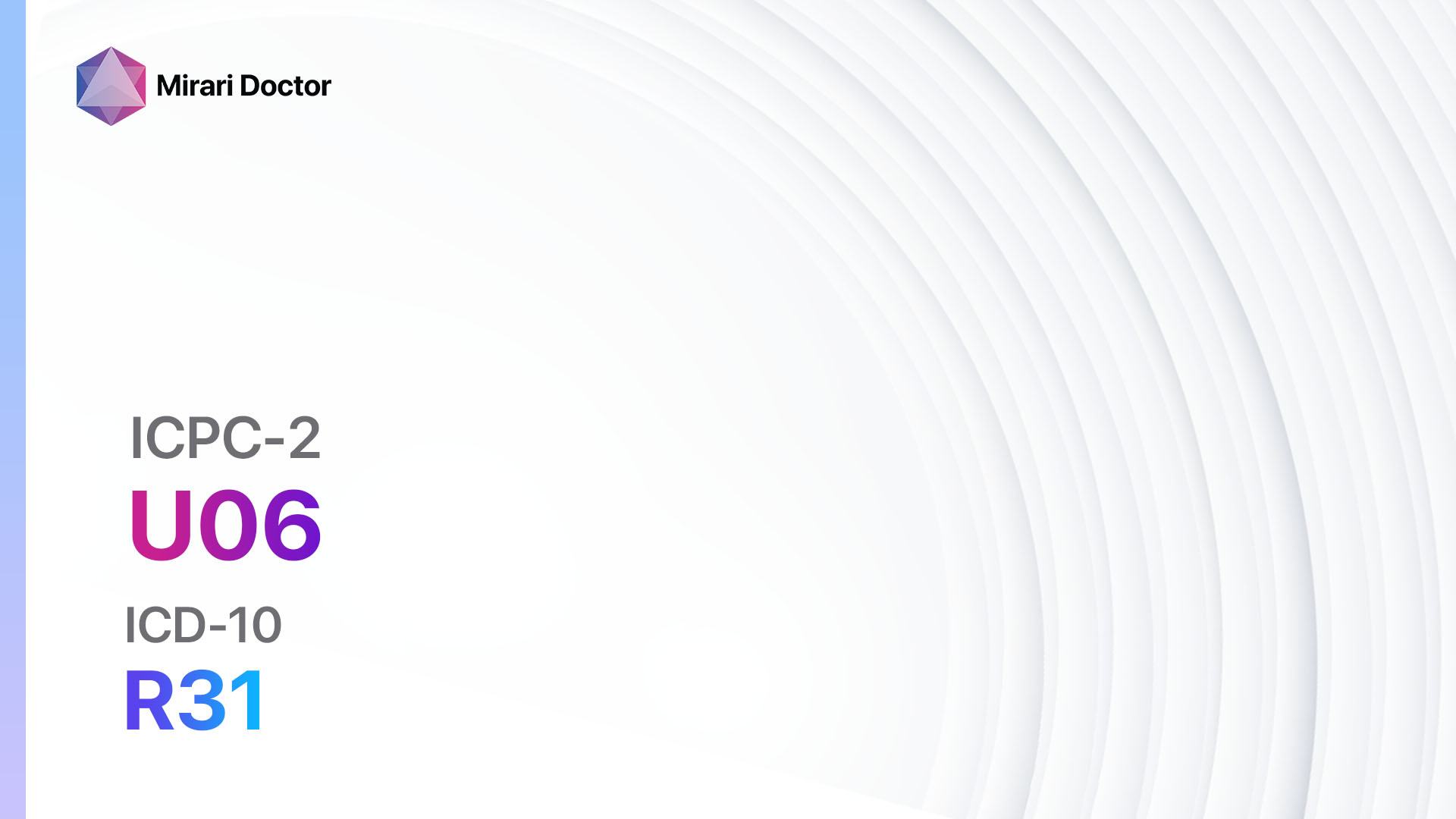
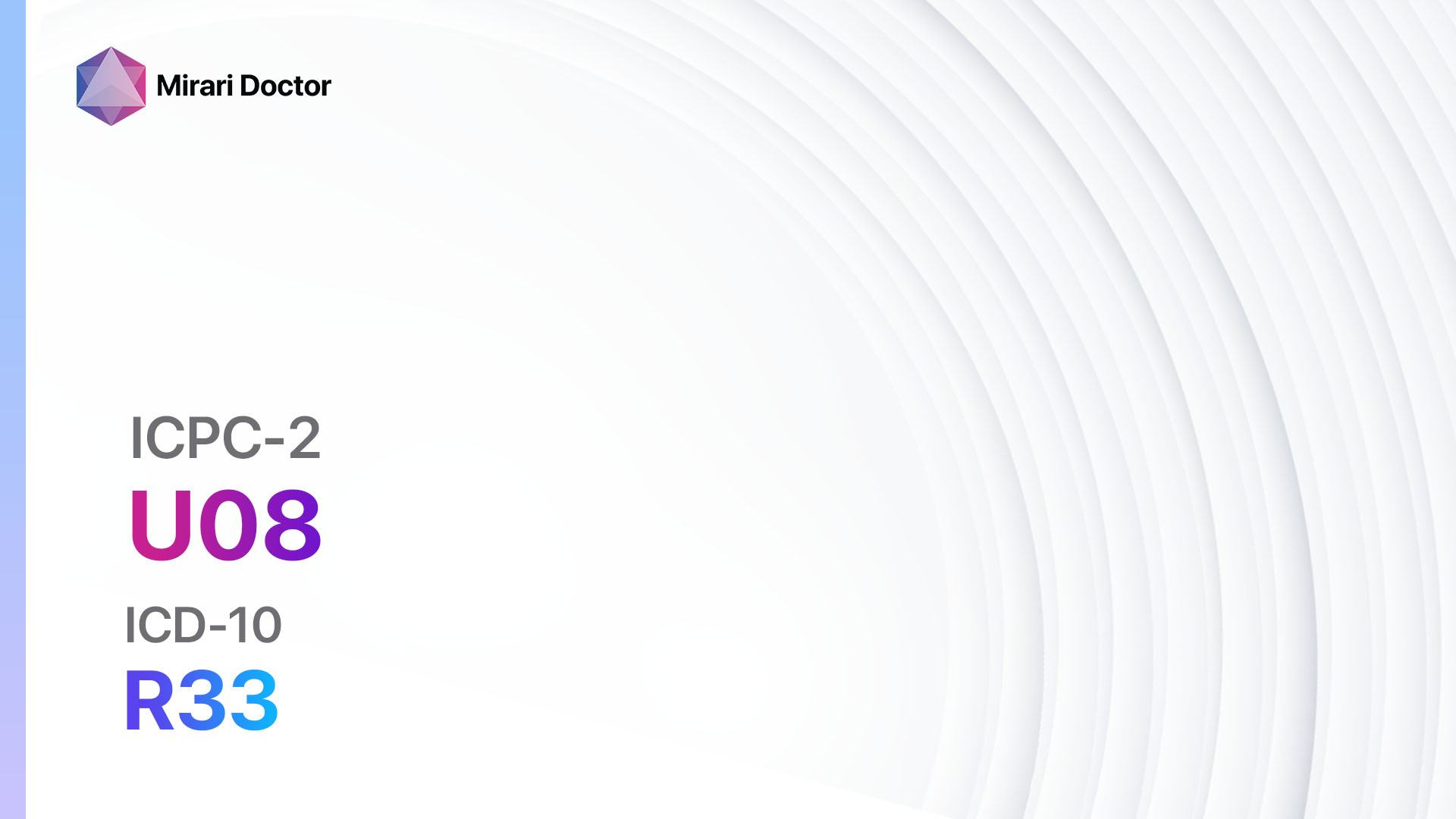
Codes
Symptoms
- Difficulty starting urination: Patients may experience difficulty initiating the flow of urine.
- Weak urine flow: The urine stream may be weak or intermittent.
- Incomplete emptying of the bladder: Patients may feel a persistent sensation of fullness or have the urge to urinate again shortly after voiding.
- Dribbling: Urine may continue to dribble out after urination has finished.
- Pain or discomfort: Some patients may experience pain or discomfort in the lower abdomen or pelvic area[2].
Causes
- Nerve dysfunction: Conditions such as multiple sclerosis, spinal cord injury, or nerve damage from surgery can disrupt the normal nerve signals that control bladder function.
- Obstruction: Enlarged prostate, bladder stones, or tumors can obstruct the flow of urine.
- Medication side effects: Certain medications, such as antihistamines, decongestants, or muscle relaxants, can interfere with bladder function[3].
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration and severity.
- Identify any risk factors, such as a history of nerve dysfunction or medication use.
- Assess the patient’s medical history for conditions that may contribute to urinary retention[4].
Physical Examination
- Perform a thorough physical examination, including a focused abdominal examination to assess for any signs of bladder distension.
- Evaluate the patient’s neurological function, including testing for sensation and reflexes in the lower extremities[5].
Laboratory Tests
- Urinalysis: Assess for the presence of infection or other abnormalities in the urine.
- Blood tests: Measure kidney function and assess for any underlying medical conditions, such as diabetes or electrolyte imbalances[6].
Diagnostic Imaging
- Ultrasound: Visualize the bladder and assess for any structural abnormalities or signs of obstruction.
- Cystoscopy: Insert a thin tube with a camera into the urethra and bladder to directly visualize the urinary tract and identify any obstructions or abnormalities[7].
Other Tests
- Urodynamic studies: Measure bladder pressure and flow rates to assess bladder function and identify any abnormalities.
- Post-void residual measurement: Measure the amount of urine left in the bladder after voiding to assess for incomplete emptying[8].
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the patient’s progress and adjust treatment as necessary.
- Provide education on self-catheterization techniques, if applicable.
- Discuss lifestyle modifications and interventions to manage urinary retention[9][10].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Urinary retention:
- Alpha-blockers (e.g., Tamsulosin, Terazosin):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to alpha-blockers.
- Side effects: Dizziness, low blood pressure.
- Severe side effects: Priapism (prolonged erection), fainting.
- Drug interactions: Other blood pressure medications.
- Warning: Take medication at bedtime to minimize dizziness.
- Anticholinergic medications (e.g., Oxybutynin, Tolterodine):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Glaucoma, urinary retention due to bladder outlet obstruction.
- Side effects: Dry mouth, constipation.
- Severe side effects: Urinary retention, confusion.
- Drug interactions: Other anticholinergic medications.
- Warning: Avoid activities requiring mental alertness due to potential drowsiness.
- 5-alpha reductase inhibitors (e.g., Finasteride):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to 5-alpha reductase inhibitors.
- Side effects: Decreased libido, erectile dysfunction.
- Severe side effects: Allergic reactions, breast tenderness.
- Drug interactions: None reported.
- Warning: May take several months to see the full effect.
- Mirabegron:
- Cost: $100-$200/month.
- Contraindications: Severe uncontrolled hypertension.
- Side effects: Increased blood pressure, headache.
- Severe side effects: Urinary retention, angioedema.
- Drug interactions: None reported.
- Warning: Monitor blood pressure regularly.
- Botulinum toxin injections (e.g., OnabotulinumtoxinA):
- Cost: $1000-$2000 per treatment.
- Contraindications: Urinary tract infection, allergy to botulinum toxin.
- Side effects: Urinary tract infection, urinary retention.
- Severe side effects: Allergic reactions, muscle weakness.
- Drug interactions: None reported.
- Warning: Requires repeated injections every few months.
Alternative Drugs:
- Desmopressin: A synthetic hormone that reduces urine production.
- Bethanechol: Stimulates bladder contractions to improve urine flow.
- Prostaglandin E1: Helps relax the smooth muscles of the bladder and urethra.
- Imipramine: A tricyclic antidepressant that can help relax the bladder muscles.
- Duloxetine: An antidepressant that can help improve bladder control.
Surgical Procedures:
- Transurethral resection of the prostate (TURP): Remove excess prostate tissue that is obstructing urine flow. Cost: $10,000-$20,000.
- Urethral dilation: Stretch the urethra to improve urine flow. Cost: $5,000-$10,000.
- Artificial urinary sphincter: Implant a device to control urine flow in cases of severe urinary incontinence. Cost: $15,000-$30,000.
Alternative Interventions
- Acupuncture: May help improve bladder function and reduce urinary retention. Cost: $60-$120 per session.
- Biofeedback: Teaches patients to control their pelvic muscles and improve bladder control. Cost: $100-$200 per session.
- Herbal supplements: Some herbs, such as saw palmetto or pumpkin seed extract, may have potential benefits for urinary symptoms. Cost: Varies depending on the specific supplement.
- Pelvic floor exercises: Strengthening the pelvic floor muscles can help improve bladder control. Cost: Free.
- Bladder training: A behavioral therapy technique to gradually increase the time between urination. Cost: Free.
Lifestyle Interventions
- Fluid management: Limiting fluid intake, especially before bedtime, can help reduce urinary frequency and urgency. Cost: Free.
- Avoiding bladder irritants: Certain foods and beverages, such as caffeine, alcohol, and spicy foods, can irritate the bladder and worsen urinary symptoms. Cost: Varies depending on dietary choices.
- Weight management: Maintaining a healthy weight can reduce pressure on the bladder and improve urinary control. Cost: Varies depending on individual weight management strategies.
- Scheduled voiding: Establishing a regular voiding schedule can help train the bladder and reduce urinary urgency. Cost: Free.
- Stress management: Stress can exacerbate urinary symptoms, so implementing stress-reduction techniques, such as meditation or yoga, may be beneficial. Cost: Varies depending on chosen stress management methods.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – U08 Urinary retention (ICD-10:R33)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 6 (Liver/Kidney Therapy) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 6 (Liver/Kidney Therapy)) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting:7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting:7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Urinary retention effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Urinary retention. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Selius, B. A., & Subedi, R. (2008). Urinary retention in adults: diagnosis and initial management. American Family Physician, 77(5), 643-650.
- Abrams, P., Cardozo, L., Fall, M., Griffiths, D., Rosier, P., Ulmsten, U., … & Wein, A. (2002). The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub‐committee of the International Continence Society. Neurourology and Urodynamics, 21(2), 167-178.
- Verhamme, K. M., Sturkenboom, M. C., Stricker, B. H., & Bosch, R. (2008). Drug-induced urinary retention. Drug Safety, 31(5), 373-388.
- Gratzke, C., Bachmann, A., Descazeaud, A., Drake, M. J., Madersbacher, S., Mamoulakis, C., … & Gravas, S. (2015). EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. European Urology, 67(6), 1099-1109.
- Chapple, C. R., & Milsom, I. (2012). Urinary incontinence and pelvic prolapse: epidemiology and pathophysiology. Campbell-Walsh Urology, 10, 1871-1895.
- Nitti, V. W. (2005). Pressure flow urodynamic studies: the gold standard for diagnosing bladder outlet obstruction. Reviews in Urology, 7(Suppl 6), S14.
- Dmochowski, R. R. (2005). Bladder outlet obstruction: etiology and evaluation. Reviews in Urology, 7(Suppl 6), S3.
- Abrams, P. (2006). New words for old: lower urinary tract symptoms for “prostatism”. BMJ, 308(6934), 929-930.
- Gormley, E. A., Lightner, D. J., Burgio, K. L., Chai, T. C., Clemens, J. Q., Culkin, D. J., … & Vasavada, S. P. (2012). Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. The Journal of Urology, 188(6 Suppl), 2455-2463.
- Irwin, D. E., Kopp, Z. S., Agatep, B., Milsom, I., & Abrams, P. (2011). Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU International, 108(7), 1132-1138.
Related articles
Made in USA