Introduction
Urinary calculus, also known as kidney stones, is a common condition characterized by the formation of hard deposits in the urinary tract. These stones can cause severe pain and discomfort, and if left untreated, can lead to complications such as urinary tract infections and kidney damage[1]. The aim of this guide is to provide a comprehensive overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for urinary calculus.
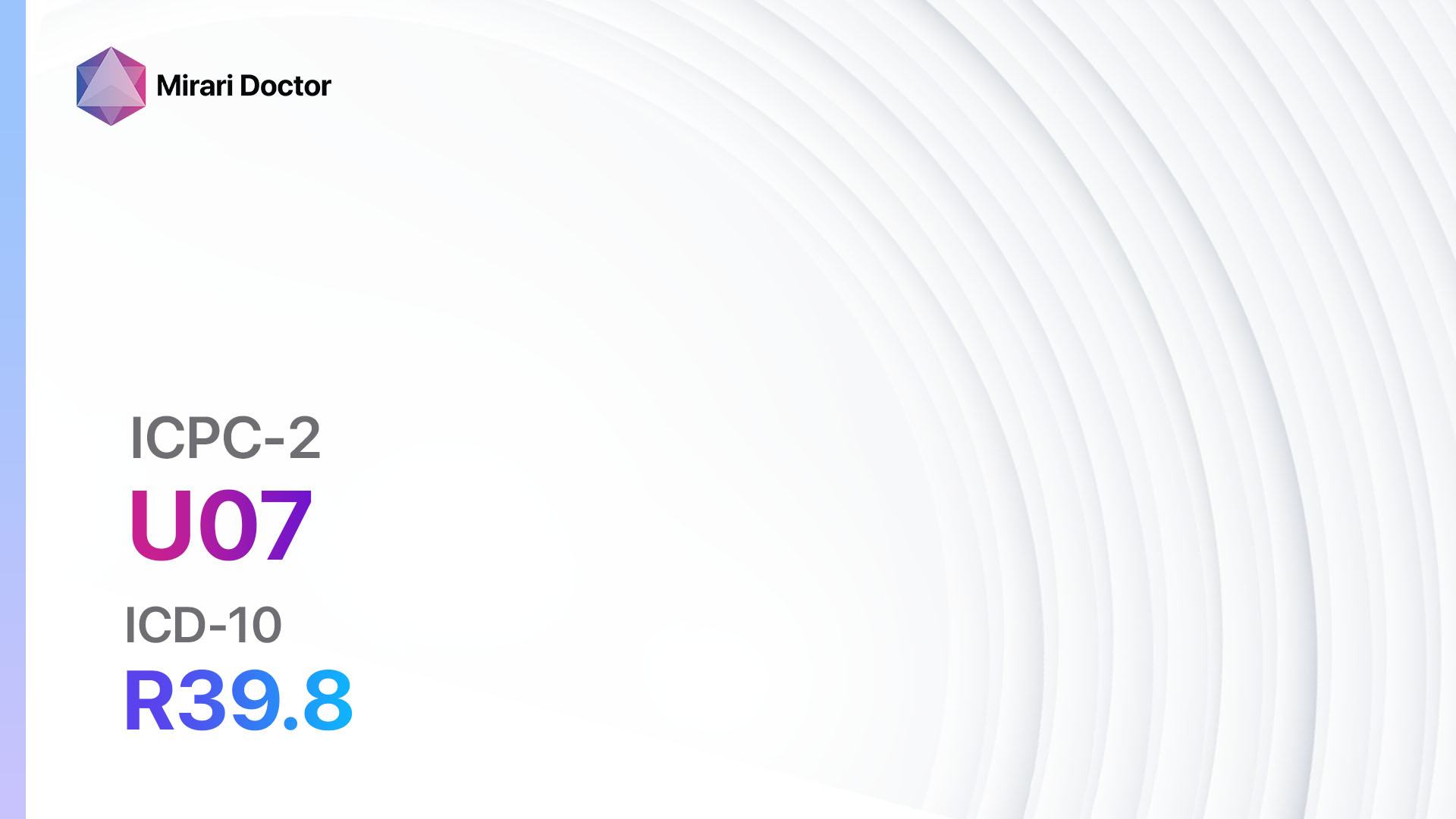
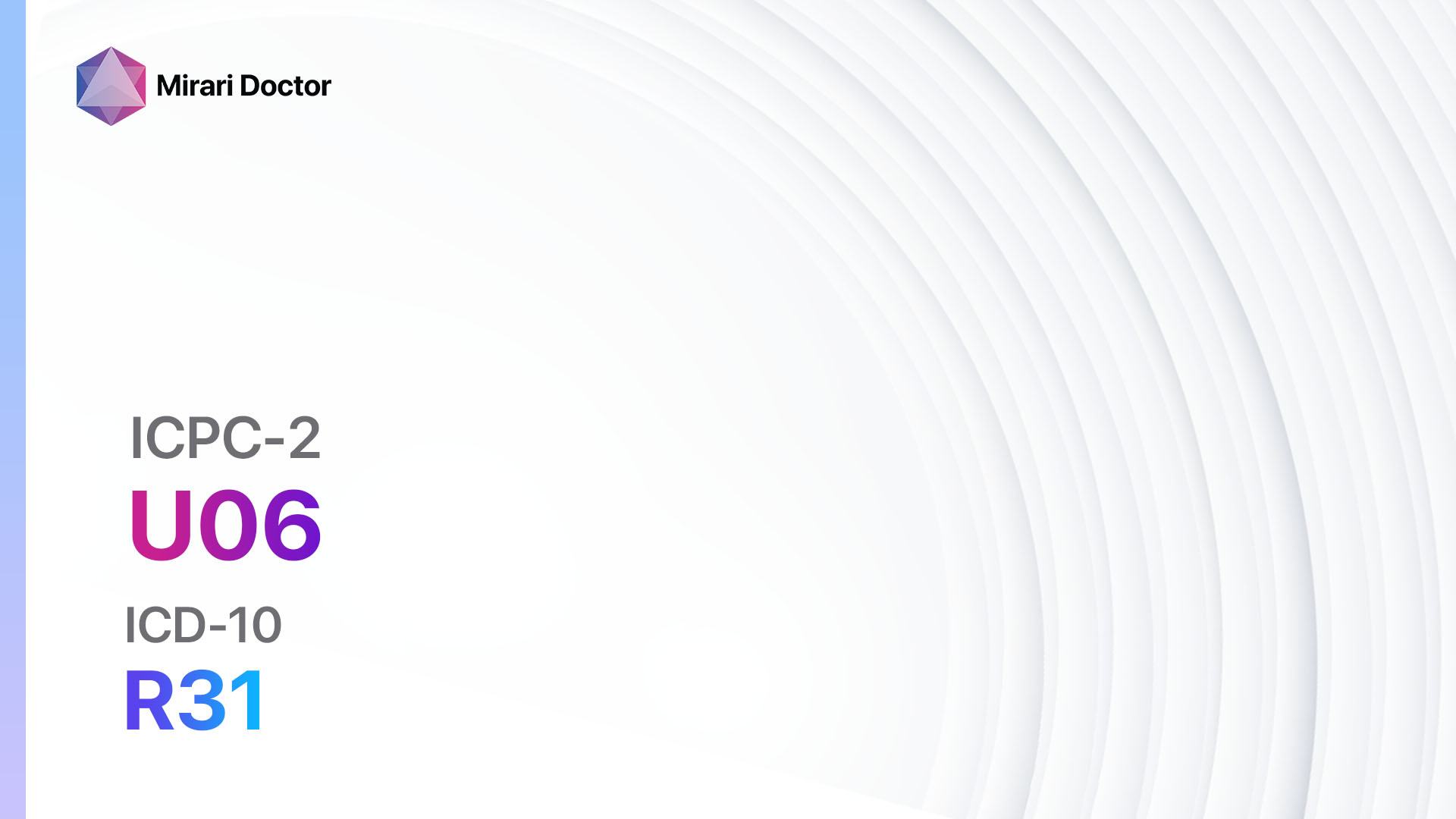
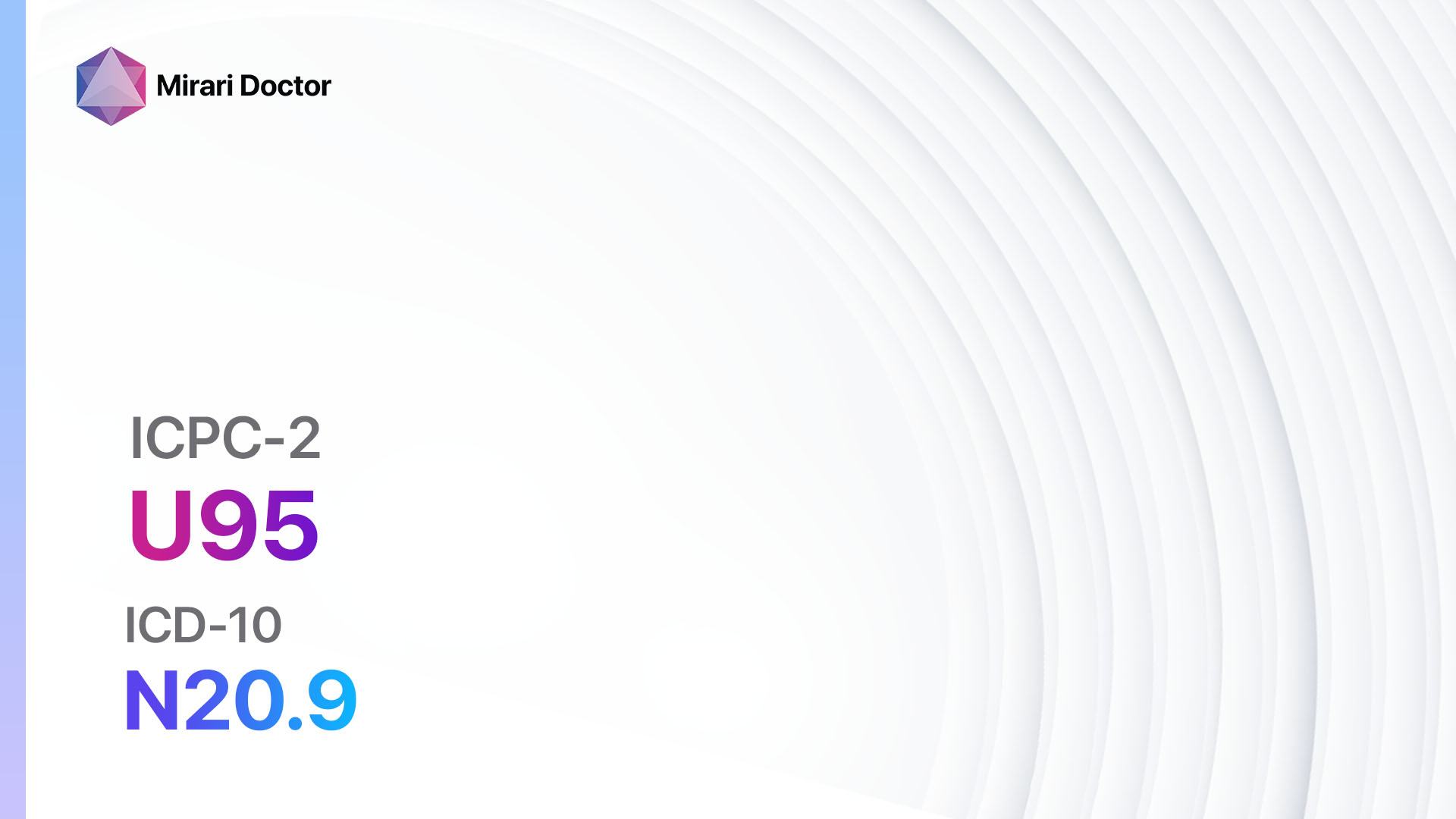
Codes
- ICPC-2 Code: U95 Urinary calculus
- ICD-10 Code: N20.9 Urinary calculus, unspecified[2]
Symptoms
- Severe pain in the back or side, below the ribs
- Pain that radiates to the lower abdomen and groin
- Blood in the urine
- Frequent urination
- Cloudy or foul-smelling urine
- Nausea and vomiting
- Fever and chills (if there is an infection)[3]
Causes
- Dehydration: Lack of fluid intake can lead to concentrated urine, increasing the risk of stone formation.
- Diet: Consuming a diet high in sodium, oxalate, and animal protein can increase the risk of developing kidney stones.
- Family history: Individuals with a family history of kidney stones are more likely to develop the condition.
- Medical conditions: Certain medical conditions such as urinary tract infections, gout, and certain metabolic disorders can increase the risk of stone formation.
- Certain medications: Some medications, such as diuretics and antacids containing calcium, can increase the risk of kidney stone formation[4].
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the location and severity of pain, presence of blood in the urine, and any previous history of kidney stones.
- Inquire about the patient’s medical history, including any underlying medical conditions or medications that may contribute to stone formation.
- Assess the patient’s lifestyle factors, such as diet and fluid intake[5].
Physical Examination
- Perform a thorough physical examination, including palpation of the abdomen to check for tenderness or swelling.
- Check for any signs of infection, such as fever or chills.
- Evaluate the patient’s overall hydration status[6].
Laboratory Tests
- Urinalysis: This test can detect the presence of blood, crystals, or infection in the urine.
- Complete blood count (CBC): A CBC can help identify signs of infection or inflammation.
- Blood chemistry panel: This panel can assess kidney function and evaluate levels of calcium, uric acid, and other substances that may contribute to stone formation.
- 24-hour urine collection: This test measures the levels of various substances in the urine over a 24-hour period, providing valuable information about the patient’s risk of stone formation[7].
Diagnostic Imaging
- X-ray: X-rays can detect the presence of kidney stones and help determine their size and location.
- Ultrasound: Ultrasound imaging can provide detailed images of the kidneys and urinary tract, helping to identify the presence of stones.
- CT scan: CT scans are highly accurate in detecting kidney stones and can provide detailed information about their size, location, and composition.
- Intravenous pyelogram (IVP): This imaging test involves injecting a contrast dye into the bloodstream to visualize the urinary tract and identify any abnormalities[8].
Other Tests
- Stone analysis: If a stone is passed or removed, it can be sent for analysis to determine its composition, which can help guide treatment and prevention strategies.
- Urodynamic studies: These tests evaluate the function of the urinary tract and can help identify any underlying issues that may contribute to stone formation[9].
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the patient’s progress and assess the effectiveness of interventions.
- Provide education on dietary modifications, fluid intake recommendations, and lifestyle changes to prevent future stone formation.
- Discuss the importance of regular follow-up and adherence to prescribed medications[10].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Urinary calculus:
- Alpha-blockers (e.g., Tamsulosin):
- Cost: $10-$50/month.
- Contraindications: Hypersensitivity to alpha-blockers.
- Side effects: Dizziness, low blood pressure.
- Severe side effects: Priapism (prolonged erection), allergic reactions.
- Drug interactions: Other medications that lower blood pressure.
- Warning: May cause drowsiness, avoid activities requiring mental alertness.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., Ibuprofen, Naproxen):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: Active peptic ulcer disease, history of gastrointestinal bleeding.
- Side effects: Upset stomach, heartburn.
- Severe side effects: Gastrointestinal bleeding, kidney damage.
- Drug interactions: Anticoagulants, other NSAIDs.
- Warning: Use with caution in patients with kidney disease or cardiovascular disease.
- Calcium channel blockers (e.g., Nifedipine):
- Cost: Generic versions can be $10-$30/month.
- Contraindications: Hypersensitivity to calcium channel blockers, severe hypotension.
- Side effects: Headache, dizziness.
- Severe side effects: Rapid heartbeat, swelling of the ankles.
- Drug interactions: Grapefruit juice, other blood pressure medications.
- Warning: Avoid sudden discontinuation, may cause rebound hypertension.
- Thiazide diuretics (e.g., Hydrochlorothiazide):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: Anuria (absence of urine production), hypersensitivity to thiazide diuretics.
- Side effects: Increased urination, electrolyte imbalances.
- Severe side effects: Low blood pressure, kidney dysfunction.
- Drug interactions: Lithium, other blood pressure medications.
- Warning: Monitor electrolyte levels regularly.
- Potassium citrate:
- Cost: $20-$100/month.
- Contraindications: Hyperkalemia (high blood potassium levels), severe renal impairment.
- Side effects: Upset stomach, diarrhea.
- Severe side effects: Metabolic alkalosis, muscle weakness.
- Drug interactions: Potassium-sparing diuretics, ACE inhibitors.
- Warning: Regular monitoring of kidney function and electrolyte levels required.
Alternative Drugs:
- Thiazide-like diuretics (e.g., Chlorthalidone): Similar to thiazide diuretics, but with a longer duration of action.
- Allopurinol: Used to reduce uric acid levels in the blood, which can help prevent certain types of kidney stones.
- Phosphate binders (e.g., Sevelamer): Used to reduce the absorption of dietary phosphate, which can help prevent the formation of calcium phosphate stones.
- Antibiotics: Prescribed if there is an associated urinary tract infection.
Surgical Procedures:
- Extracorporeal shock wave lithotripsy (ESWL): High-energy shock waves are used to break up kidney stones into smaller pieces that can be passed more easily. Cost: $10,000 to $20,000.
- Ureteroscopy: A thin tube with a camera is inserted into the ureter to locate and remove or break up the stone. Cost: $10,000 to $20,000.
- Percutaneous nephrolithotomy (PCNL): A small incision is made in the back to access the kidney and remove the stone. Cost: $15,000 to $30,000.
- Open surgery: In rare cases, open surgery may be necessary to remove large or complex stones. Cost: $20,000 to $40,000.
Alternative Interventions
- Acupuncture: May help relieve pain and promote relaxation. Cost: $60-$120 per session.
- Herbal remedies: Certain herbs, such as chanca piedra and hydrangea root, are believed to have diuretic and stone-dissolving properties. Cost: Varies depending on the specific herb and formulation.
- Dietary modifications: Increasing fluid intake, reducing sodium and oxalate intake, and consuming foods rich in citrate (such as lemons and oranges) may help prevent stone formation. Cost: Varies depending on individual food choices.
- Hydration therapy: Intravenous hydration with saline solution may help flush out small stones. Cost: $100-$300 per session.
- Extracorporeal magnetic innervation (ExMI): This non-invasive therapy uses pulsed magnetic fields to stimulate the nerves in the lower back, potentially helping to relax the ureter and facilitate stone passage. Cost: $100-$200 per session.
Lifestyle Interventions
- Increase fluid intake: Aim to drink at least 2-3 liters of water per day to help flush out the urinary system.
- Dietary modifications: Reduce sodium, oxalate, and animal protein intake. Increase consumption of fruits, vegetables, and whole grains.
- Weight management: Maintain a healthy weight to reduce the risk of stone formation.
- Regular exercise: Engage in regular physical activity to promote overall health and prevent stone formation.
- Avoid certain foods and beverages: Limit or avoid alcohol, caffeine, and sugary drinks, as they can contribute to stone formation.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. It is recommended to consult with a healthcare professional for personalized treatment options and cost estimates.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – U95 Urinary calculus (ICD-10:N20.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 6 (Liver/Kidney Therapy) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Urinary calculus effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Urinary calculus. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl. 2013;3:1-150.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems (ICD-10). 2019.
- Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO Clinical Practice Guideline for Glomerulonephritis. Kidney Int Suppl. 2012;2:139-274.
- Nicolaou N, et al. Genetic, environmental, and epigenetic factors involved in CAKUT. Nature Reviews Nephrology. 2015;11(12):720-731.
- Chevalier RL. Congenital Anomalies of the Kidneys and Urinary Tract. NeoReviews. 2019;20(5):e280-e289.
- Rabinowitz R. Bladder Anomalies. MSD Manual Professional Edition. 2023.
- Morey AF, et al. Urotrauma: AUA guideline. Journal of Urology. 2014;192(2):327-335.
- Summerton DJ, et al. EAU guidelines on iatrogenic trauma. European Urology. 2012;62(4):628-639.
- Lange-Sperandio B, et al. Congenital Anomalies of the Kidney and Urinary Tract: A Continuum of Care. Seminars in Nephrology. 2023;43(5):551-563.
- Stonebrook E, et al. Congenital Anomalies of the Kidney and Urinary Tract: A Clinical Review. Pediatric Nephrology. 2020;35(5):753-761.
Related articles
Made in USA