Introduction
Fear of cancer of the urinary system is a common concern among individuals, as it can significantly impact their quality of life and mental well-being[1]. This guide aims to provide a comprehensive overview of the condition, including its symptoms, causes, diagnostic steps, possible interventions, and lifestyle modifications. By understanding the disease and its management options, patients can make informed decisions and alleviate their fears.
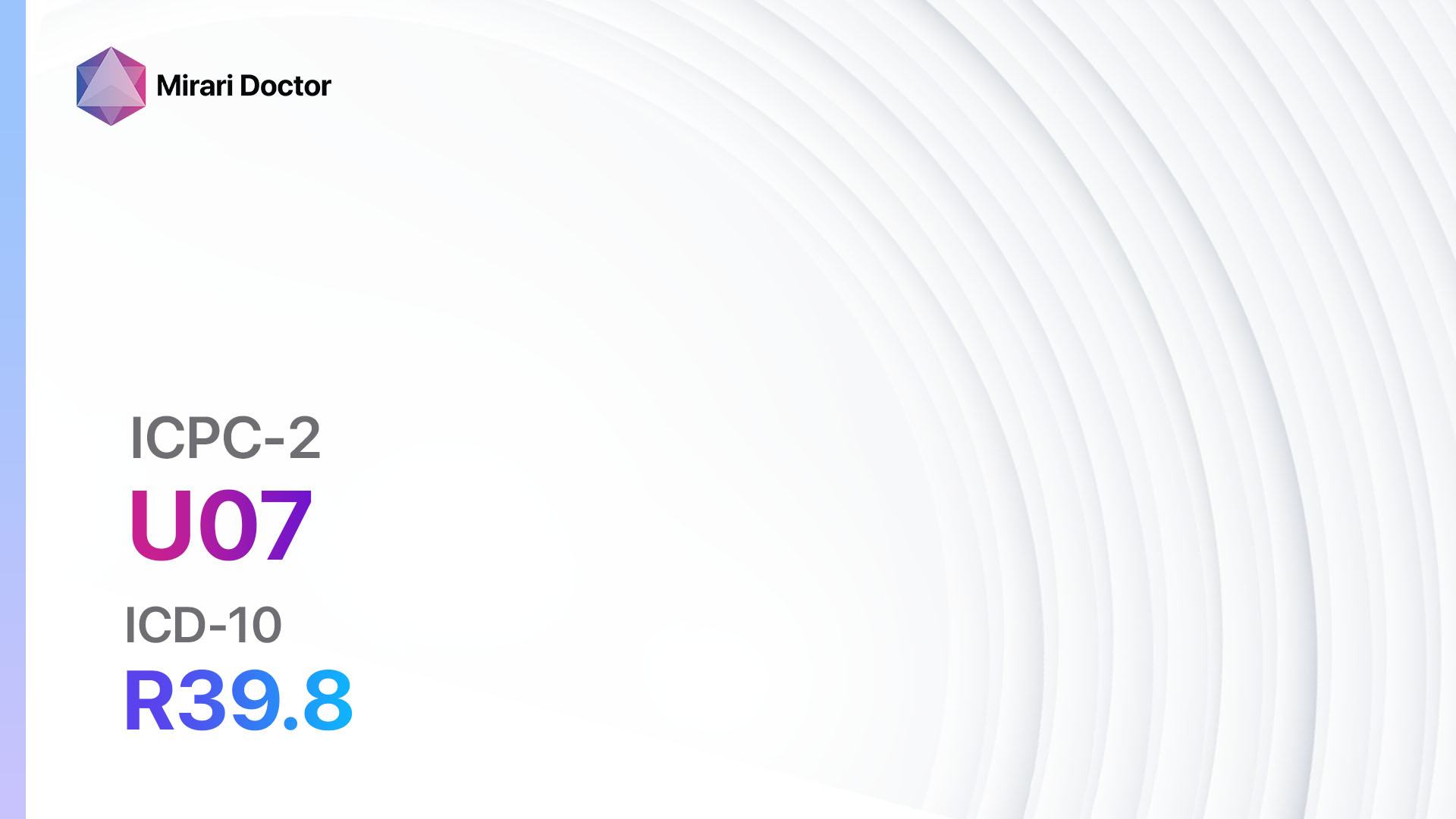
Codes
- ICPC-2 Code: U26 Fear of cancer of urinary system
- ICD-10 Code: Z71.1 Person with feared complaint in whom no diagnosis is made
Symptoms
- Blood in the urine (hematuria): This can be visible or microscopic[2].
- Frequent urination: The need to urinate more often than usual.
- Pain or discomfort during urination: This can include a burning sensation or pressure in the bladder or urethra.
- Lower back pain: Pain in the lower back or sides of the body.
- Pelvic pain: Pain in the lower abdomen or pelvis.
- Fatigue: Feeling tired or lacking energy.
- Unexplained weight loss: Losing weight without trying[3].
Causes
- Smoking: Smoking is a significant risk factor for developing urinary system cancers[4].
- Exposure to certain chemicals: Exposure to certain chemicals, such as those found in the workplace or in certain medications, may increase the risk of developing cancer.
- Chronic bladder inflammation: Conditions that cause chronic inflammation of the bladder, such as urinary tract infections or bladder stones, may increase the risk of developing cancer.
- Family history: Having a family history of urinary system cancers can increase the risk of developing the disease.
- Age: The risk of developing urinary system cancers increases with age[5].
Diagnostic Steps
Medical History
- Gather information about the patient’s risk factors, such as smoking history, exposure to chemicals, and family history of urinary system cancers.
- Assess the patient’s medical conditions, including any history of chronic bladder inflammation or other urinary system disorders.
- Inquire about the patient’s symptoms, including the presence of blood in the urine, frequent urination, pain or discomfort during urination, lower back pain, pelvic pain, fatigue, and unexplained weight loss[6].
Physical Examination
- Perform a thorough physical examination, including a general assessment of the patient’s overall health.
- Focus on specific signs or findings that may indicate the presence of urinary system cancers, such as palpable masses or tenderness in the abdomen or pelvis[7].
Laboratory Tests
- Urinalysis: Analyze a urine sample for the presence of blood, infection, or other abnormalities.
- Complete blood count (CBC): Assess the levels of different blood cells, which may indicate the presence of infection or anemia.
- Kidney function tests: Measure the levels of creatinine and blood urea nitrogen (BUN) to assess kidney function.
- Tumor markers: Measure the levels of specific proteins in the blood that may be elevated in the presence of urinary system cancers[8].
Diagnostic Imaging
- Ultrasound: Use high-frequency sound waves to create images of the urinary system, allowing for the visualization of any abnormalities.
- CT scan: Provide detailed cross-sectional images of the urinary system, helping to identify tumors or other abnormalities.
- MRI: Use powerful magnets and radio waves to create detailed images of the urinary system, providing information about the size and location of tumors.
- Cystoscopy: Insert a thin, flexible tube with a camera into the urethra and bladder to visualize the urinary system and collect tissue samples for further analysis[9].
Other Tests
- Biopsy: Collect a sample of tissue from the urinary system for laboratory analysis to confirm the presence of cancer.
- Genetic testing: Assess the presence of specific genetic mutations that may increase the risk of developing urinary system cancers[10].
Follow-up and Patient Education
- Provide patients with the results of their diagnostic tests and explain the implications.
- Offer counseling and support to address the patient’s fears and concerns.
- Educate patients about the importance of regular screenings and follow-up appointments to monitor their condition.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Fear of cancer of urinary system:
- Antianxiety medications (e.g., Alprazolam, Diazepam, Lorazepam):
- Cost: Generic versions can be $3-$50/month.
- Contraindications: Hypersensitivity to benzodiazepines, acute narrow-angle glaucoma.
- Side effects: Drowsiness, dizziness, confusion.
- Severe side effects: Respiratory depression, dependence.
- Drug interactions: Alcohol, opioids.
- Warning: May cause drowsiness, avoid driving or operating machinery.
- Selective serotonin reuptake inhibitors (SSRIs) (e.g., Fluoxetine, Sertraline, Escitalopram):
- Cost: Generic versions can be $3-$50/month.
- Contraindications: Hypersensitivity to SSRIs, concurrent use of monoamine oxidase inhibitors (MAOIs).
- Side effects: Nausea, headache, sexual dysfunction.
- Severe side effects: Serotonin syndrome, suicidal thoughts.
- Drug interactions: MAOIs, other serotonergic drugs.
- Warning: May increase the risk of suicidal thoughts, especially in children and young adults.
- Beta-blockers (e.g., Propranolol, Atenolol, Metoprolol):
- Cost: Generic versions can be \<$30/month.
- Contraindications: Severe bradycardia, heart block, uncontrolled heart failure.
- Side effects: Fatigue, dizziness, bradycardia.
- Severe side effects: Bronchospasm, heart block.
- Drug interactions: Calcium channel blockers, insulin.
- Warning: Should not be abruptly stopped.
- Antidepressants (e.g., Amitriptyline, Nortriptyline, Imipramine):
- Cost: Generic versions can be $3-$50/month.
- Contraindications: Hypersensitivity to tricyclic antidepressants, recent myocardial infarction.
- Side effects: Dry mouth, constipation, sedation.
- Severe side effects: Cardiac arrhythmias, seizures.
- Drug interactions: MAOIs, other serotonergic drugs.
- Warning: May cause drowsiness, avoid driving or operating machinery.
- Antipsychotics (e.g., Risperidone, Quetiapine, Olanzapine):
- Cost: Generic versions can be $3-$50/month.
- Contraindications: Hypersensitivity to antipsychotics, dementia-related psychosis.
- Side effects: Weight gain, sedation, extrapyramidal symptoms.
- Severe side effects: Neuroleptic malignant syndrome, tardive dyskinesia.
- Drug interactions: Other antipsychotics, drugs that prolong the QT interval.
- Warning: May cause drowsiness, avoid driving or operating machinery.
Alternative Drugs:
- Herbal supplements (e.g., Valerian root, Passionflower): Some herbal supplements may have calming effects and help alleviate anxiety. Cost: Varies depending on the specific supplement.
- Cognitive-behavioral therapy (CBT): A form of psychotherapy that helps individuals identify and change negative thought patterns and behaviors. Cost: $100-$200 per session.
- Support groups: Joining a support group can provide emotional support and a sense of community. Cost: Varies depending on the specific group.
Surgical Procedures
- Cystectomy: Surgical removal of all or part of the bladder. Cost: $30,000 to $100,000.
- Nephrectomy: Surgical removal of a kidney. Cost: $20,000 to $80,000.
- Partial nephrectomy: Surgical removal of part of a kidney. Cost: $15,000 to $60,000.
Radiation Therapy
- External beam radiation therapy: High-energy beams are directed at the tumor to destroy cancer cells. Cost: $10,000 to $50,000.
- Brachytherapy: Radioactive seeds or sources are placed directly into or near the tumor to deliver radiation. Cost: $20,000 to $60,000.
Chemotherapy
- Systemic chemotherapy: Medications are given orally or intravenously to kill cancer cells throughout the body. Cost: $3,000 to $10,000 per month.
- Intravesical chemotherapy: Medications are placed directly into the bladder through a catheter to kill cancer cells. Cost: $1,000 to $5,000 per treatment.
Immunotherapy
- Bacillus Calmette-Guérin (BCG) therapy: A weakened form of the tuberculosis bacterium is placed directly into the bladder to stimulate the immune system to attack cancer cells. Cost: $5,000 to $10,000 per treatment.
Targeted Therapy
- Tyrosine kinase inhibitors: Medications that target specific proteins involved in cancer cell growth and division. Cost: $5,000 to $15,000 per month.
Palliative Care
- Pain management: Medications and interventions to alleviate pain and improve quality of life. Cost: Varies depending on the specific treatment.
- Psychological support: Counseling and therapy to address emotional and psychological distress. Cost: $100-$200 per session.
Lifestyle Interventions
- Regular exercise: Engaging in regular physical activity can help reduce anxiety and improve overall well-being. Cost: Varies depending on the specific activity.
- Healthy diet: Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health. Cost: Varies depending on individual food choices.
- Stress management: Practicing stress-reducing techniques, such as meditation, deep breathing exercises, or yoga, can help alleviate anxiety. Cost: Varies depending on the specific technique.
- Support groups: Joining a support group can provide emotional support and a sense of community. Cost: Varies depending on the specific group.
- Mind-body therapies: Techniques such as acupuncture, massage therapy, or aromatherapy may help reduce anxiety and promote relaxation. Cost: Varies depending on the specific therapy.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. Patients should consult with their healthcare provider for specific cost information and to determine the most appropriate interventions for their individual needs.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – U26 Fear of cancer of urinary system (ICD-10:Z71.1)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 6 (Liver/Kidney Therapy) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting:7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting:7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Fear of cancer of urinary system effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Fear of cancer of urinary system. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Crist JV, Grunfeld EA. Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psychooncology. 2013;22(5):978-986.
- Grossfeld GD, Wolf JS Jr, Litwin MS, et al. Asymptomatic microscopic hematuria in adults: summary of the AUA best practice policy recommendations. Am Fam Physician. 2001;63(6):1145-1154.
- American Cancer Society. Signs and Symptoms of Bladder Cancer. Accessed April 15, 2023. https://www.cancer.org/cancer/bladder-cancer/detection-diagnosis-staging/signs-and-symptoms.html
- Freedman ND, Silverman DT, Hollenbeck AR, Schatzkin A, Abnet CC. Association between smoking and risk of bladder cancer among men and women. JAMA. 2011;306(7):737-745.
- Burger M, Catto JW, Dalbagni G, et al. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol. 2013;63(2):234-241.
- Babjuk M, Burger M, Compérat EM, et al. European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer (TaT1 and Carcinoma In Situ) – 2019 Update. Eur Urol. 2019;76(5):639-657.
- Lotan Y, Roehrborn CG. Sensitivity and specificity of commonly available bladder tumor markers versus cytology: results of a comprehensive literature review and meta-analyses. Urology. 2003;61(1):109-118.
- Lokeshwar VB, Habuchi T, Grossman HB, et al. Bladder tumor markers beyond cytology: International Consensus Panel on bladder tumor markers. Urology. 2005;66(6 Suppl 1):35-63.
- Witjes JA, Compérat E, Cowan NC, et al. EAU guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2013 guidelines. Eur Urol. 2014;65(4):778-792.
- Knowles MA, Hurst CD. Molecular biology of bladder cancer: new insights into pathogenesis and clinical diversity. Nat Rev Cancer. 2015;15(1):25-41.
Related articles
Made in USA