Introduction
Mental retardation, also known as intellectual disability, is a neurodevelopmental disorder characterized by significant limitations in intellectual functioning and adaptive behavior[1]. It is a lifelong condition that affects individuals from childhood and can have a profound impact on their daily functioning and quality of life[2]. The aim of this guide is to provide a comprehensive overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for mental retardation.
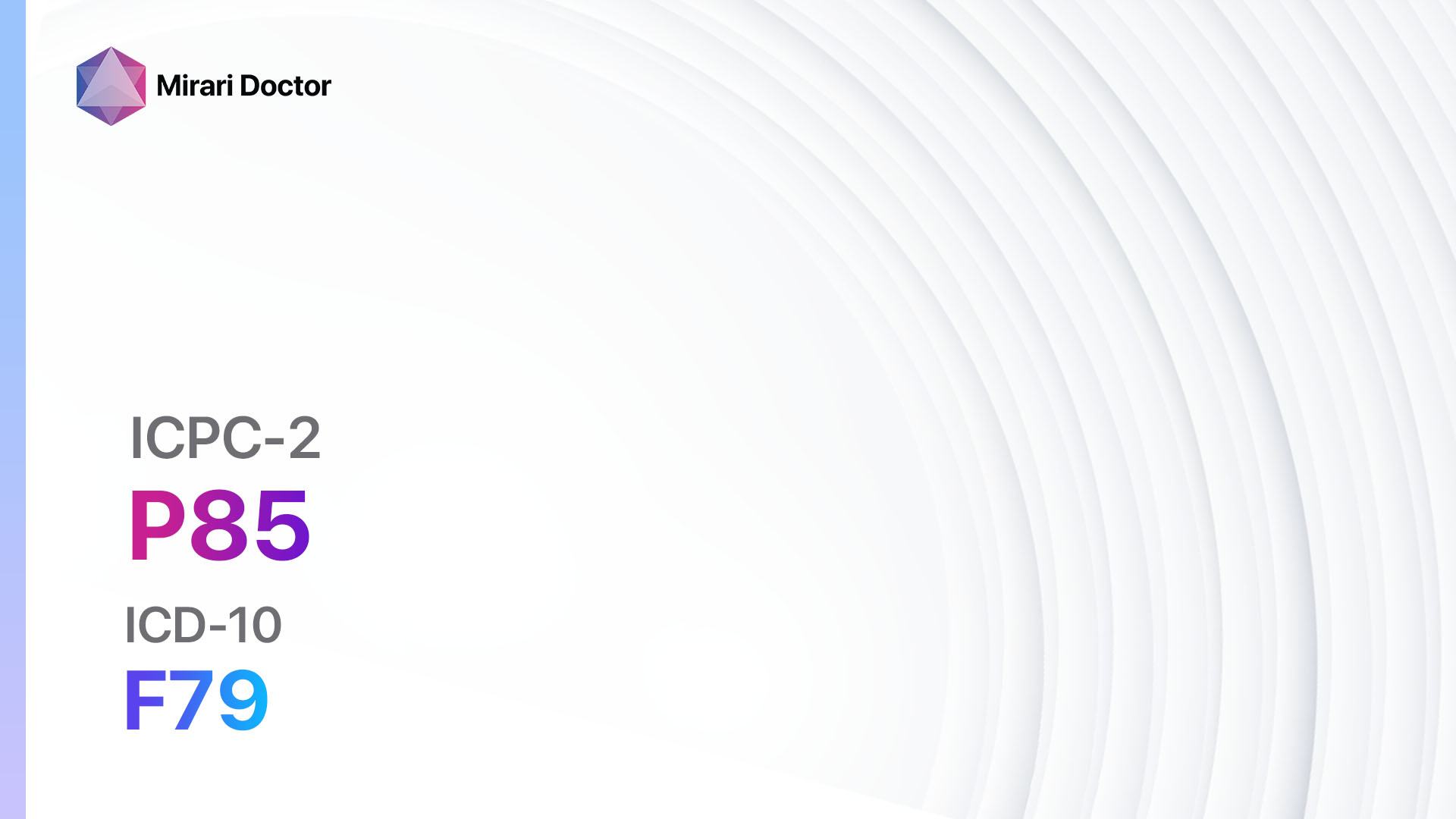
Codes
Symptoms
- Intellectual functioning: Individuals with mental retardation have below-average intellectual functioning, typically with an IQ score below 70[3].
- Adaptive behavior: They may have difficulties with adaptive behavior, including skills related to daily living, communication, socialization, and self-care[4].
- Onset in childhood: Symptoms of mental retardation are typically evident during childhood, with delays in reaching developmental milestones[5].
Causes
- Genetic factors: Mental retardation can be caused by genetic abnormalities, such as Down syndrome, Fragile X syndrome, or other chromosomal abnormalities[6].
- Prenatal factors: Exposure to certain infections, toxins, or drugs during pregnancy can increase the risk of mental retardation[7].
- Perinatal factors: Complications during childbirth, such as oxygen deprivation, can lead to mental retardation[8].
- Postnatal factors: Traumatic brain injury, infections, malnutrition, or exposure to toxins during early childhood can contribute to mental retardation[9].
Diagnostic Steps
Medical History
- Gather information about the patient’s developmental milestones, including any delays or abnormalities.
- Inquire about any family history of intellectual disability or genetic disorders.
- Assess the presence of any prenatal, perinatal, or postnatal factors that may have contributed to the development of mental retardation.
Physical Examination
- Perform a thorough physical examination to assess for any physical abnormalities or dysmorphic features associated with genetic disorders.
- Evaluate the patient’s overall health and identify any comorbid medical conditions that may be contributing to their symptoms.
Laboratory Tests
- Genetic testing: Conduct genetic testing, such as chromosomal analysis or DNA sequencing, to identify any genetic abnormalities associated with mental retardation[10].
- Metabolic screening: Perform metabolic screening tests to rule out any underlying metabolic disorders that may be causing or contributing to the patient’s symptoms.
- Blood tests: Order routine blood tests to assess the patient’s overall health and rule out any underlying medical conditions.
Diagnostic Imaging
- Brain imaging: Consider obtaining brain imaging studies, such as MRI or CT scans, to evaluate the structure and function of the brain and identify any abnormalities that may be associated with mental retardation.
Other Tests
- Developmental assessments: Administer standardized developmental assessments, such as the Bayley Scales of Infant and Toddler Development or the Wechsler Intelligence Scale for Children, to measure the patient’s intellectual functioning and identify any specific areas of impairment.
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the patient’s progress and provide ongoing support and guidance.
- Educate the patient and their family about the nature of mental retardation, available interventions, and strategies to optimize the individual’s functioning and quality of life.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Mental retardation:
- Stimulant medications (e.g., Methylphenidate, Amphetamine):
- Cost: Generic versions can range from $10 to $100 per month.
- Contraindications: History of heart problems, severe anxiety, or agitation.
- Side effects: Decreased appetite, insomnia, increased heart rate.
- Severe side effects: Psychosis, cardiovascular complications.
- Drug interactions: Monoamine oxidase inhibitors (MAOIs), certain antidepressants.
- Warning: Regular monitoring of blood pressure and heart rate is required.
- Antipsychotic medications (e.g., Risperidone, Aripiprazole):
- Cost: Generic versions can range from $10 to $200 per month.
- Contraindications: History of heart problems, liver disease, or seizures.
- Side effects: Weight gain, sedation, movement disorders.
- Severe side effects: Neuroleptic malignant syndrome, tardive dyskinesia.
- Drug interactions: Other antipsychotic medications, certain antidepressants.
- Warning: Regular monitoring of weight, blood pressure, and blood glucose levels is required.
- Antidepressant medications (e.g., Selective serotonin reuptake inhibitors – SSRIs):
- Cost: Generic versions can range from $10 to $50 per month.
- Contraindications: History of seizures, bipolar disorder, or liver disease.
- Side effects: Nausea, headache, sexual dysfunction.
- Severe side effects: Serotonin syndrome, suicidal thoughts.
- Drug interactions: Monoamine oxidase inhibitors (MAOIs), certain pain medications.
- Warning: Regular monitoring for changes in mood or behavior is required.
- Anxiolytic medications (e.g., Lorazepam, Alprazolam):
- Cost: Generic versions can range from $10 to $50 per month.
- Contraindications: History of substance abuse, sleep apnea, or respiratory depression.
- Side effects: Sedation, dizziness, confusion.
- Severe side effects: Respiratory depression, dependence.
- Drug interactions: Other sedatives, certain pain medications.
- Warning: Avoid abrupt discontinuation to prevent withdrawal symptoms.
- Mood stabilizer medications (e.g., Lithium, Valproate):
- Cost: Generic versions can range from $10 to $100 per month.
- Contraindications: History of kidney disease, severe liver disease, or pregnancy.
- Side effects: Tremor, weight gain, gastrointestinal disturbances.
- Severe side effects: Kidney damage, liver toxicity.
- Drug interactions: Other mood stabilizers, certain antipsychotic medications.
- Warning: Regular monitoring of kidney and liver function is required.
Alternative Drugs:
- Nootropic supplements (e.g., Omega-3 fatty acids, Bacopa monnieri): May have potential cognitive-enhancing effects. Cost: Varies depending on the specific supplement.
- Antioxidant supplements (e.g., Vitamin E, Coenzyme Q10): May help protect against oxidative stress and improve cognitive function. Cost: Varies depending on the specific supplement.
- GABAergic supplements (e.g., GABA, L-Theanine): May have calming effects and help reduce anxiety. Cost: Varies depending on the specific supplement.
- Herbal supplements (e.g., Ginkgo biloba, Panax ginseng): May have potential cognitive-enhancing effects. Cost: Varies depending on the specific supplement.
- Melatonin: May help regulate sleep patterns and improve sleep quality. Cost: Generic versions can range from $5 to $20 per month.
Surgical Procedures:
- There are no surgical procedures specifically indicated for the treatment of mental retardation. However, certain surgical interventions may be considered for the management of associated conditions or complications, such as epilepsy or severe behavioral disturbances.
Alternative Interventions
- Behavioral therapy: Applied Behavior Analysis (ABA) therapy is a widely used intervention for individuals with mental retardation. It focuses on teaching adaptive skills and reducing maladaptive behaviors. Cost: $50-$100 per hour.
- Speech therapy: Helps individuals with communication difficulties improve their speech and language skills. Cost: $50-$150 per hour.
- Occupational therapy: Aims to improve fine motor skills, self-care abilities, and overall independence. Cost: $50-$150 per hour.
- Social skills training: Helps individuals develop appropriate social skills and improve their ability to interact with others. Cost: $50-$100 per hour.
- Special education programs: Specialized educational programs tailored to the individual’s needs can provide structured learning environments and support. Cost: Varies depending on the specific program and location.
Lifestyle Interventions
- Structured daily routine: Establishing a structured daily routine can help individuals with mental retardation feel more organized and secure.
- Physical exercise: Regular physical exercise can improve overall health, cognitive function, and mood.
- Nutritional support: A well-balanced diet rich in nutrients, vitamins, and minerals is essential for optimal brain function and overall health.
- Social support: Encouraging social interactions and providing a supportive environment can enhance the individual’s social skills and overall well-being.
- Cognitive stimulation: Engaging in activities that stimulate cognitive function, such as puzzles, reading, or learning new skills, can help improve cognitive abilities.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – P85 Mental retardation (ICD-10:F79)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 30 minutes approx. $5 USD, Evening: 30 minutes approx. $5 USD |
Total Morning: 60 minutes approx. $10 USD, Lunch: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD, |
Total Morning: 60 minutes approx. $10 USD, Lunch: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD, |
| Usual treatment for 7-60 days approx. $70 USD – $600 USD | Usual treatment for 6-8 weeks approx. $1,260 USD – $1,680 USD |
Usual treatment for 3-6 months approx. $2,700 USD – $5,400 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Mental retardation effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Mental retardation. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
- Boat, T. F., Wu, J. T., Committee to Evaluate the Supplemental Security Income Disability Program for Children with Mental Disorders, Board on the Health of Select Populations, Institute of Medicine, … The National Academies of Sciences, Engineering, and Medicine. (2015). Mental Disorders and Disabilities Among Low-Income Children. National Academies Press (US).
- Schalock, R. L., Borthwick-Duffy, S. A., Bradley, V. J., Buntinx, W. H. E., Coulter, D. L., Craig, E. M., Gomez, S. C., Lachapelle, Y., Luckasson, R., Reeve, A., Shogren, K. A., Snell, M. E., Spreat, S., Tassé, M. J., Thompson, J. R., Verdugo-Alonso, M. A., Wehmeyer, M. L., & Yeager, M. H. (2010). Intellectual disability: Definition, classification, and systems of supports (11th ed.). American Association on Intellectual and Developmental Disabilities.
- Tassé, M. J., Schalock, R. L., Balboni, G., Bersani, H., Jr, Borthwick-Duffy, S. A., Spreat, S., Thissen, D., Widaman, K. F., & Zhang, D. (2012). The construct of adaptive behavior: its conceptualization, measurement, and use in the field of intellectual disability. American journal on intellectual and developmental disabilities, 117(4), 291–303. https://doi.org/10.1352/1944-7558-117.4.291
- Shevell, M., Ashwal, S., Donley, D., Flint, J., Gingold, M., Hirtz, D., Majnemer, A., Noetzel, M., Sheth, R. D., & Quality Standards Subcommittee of the American Academy of Neurology; Practice Committee of the Child Neurology Society (2003). Practice parameter: evaluation of the child with global developmental delay: report of the Quality Standards Subcommittee of the American Academy of Neurology and The Practice Committee of the Child Neurology Society. Neurology, 60(3), 367–380. https://doi.org/10.1212/01.wnl.0000031431.81555.16
- Moeschler, J. B., Shevell, M., & Committee on Genetics (2014). Comprehensive evaluation of the child with intellectual disability or global developmental delays. Pediatrics, 134(3), e903–e918. https://doi.org/10.1542/peds.2014-1839
- Ornoy, A., Weinstein-Fudim, L., & Ergaz, Z. (2015). Prenatal factors associated with autism spectrum disorder (ASD). Reproductive toxicology (Elmsford, N.Y.), 56, 155–169. https://doi.org/10.1016/j.reprotox.2015.05.007
- Schieve, L. A., Tian, L. H., Rankin, K., Kogan, M. D., Yeargin-Allsopp, M., Visser, S., & Rosenberg, D. (2016). Population impact of preterm birth and low birth weight on developmental disabilities in US children. Annals of epidemiology, 26(4), 267–274. https://doi.org/10.1016/j.annepidem.2016.02.012
- van Karnebeek, C. D., Jansweijer, M. C., Leenders, A. G., Offringa, M., & Hennekam, R. C. (2005). Diagnostic investigations in individuals with mental retardation: a systematic literature review of their usefulness. European journal of human genetics : EJHG, 13(1), 6–25. https://doi.org/10.1038/sj.ejhg.5201279
- Michelson, D. J., Shevell, M. I., Sherr, E. H., Moeschler, J. B., Gropman, A. L., & Ashwal, S. (2011). Evidence report: Genetic and metabolic testing on children with global developmental delay: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology, 77(17), 1629–1635. https://doi.org/10.1212/WNL.0b013e3182345896
Related articles
Made in USA