Introduction
Hyperkinetic disorder, also known as attention-deficit/hyperactivity disorder (ADHD), is a neurodevelopmental disorder characterized by persistent patterns of inattention, hyperactivity, and impulsivity that interfere with daily functioning and development[1]. It is a common condition that affects both children and adults, and if left untreated, can have significant impacts on academic, occupational, and social functioning[2]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of hyperkinetic disorder.
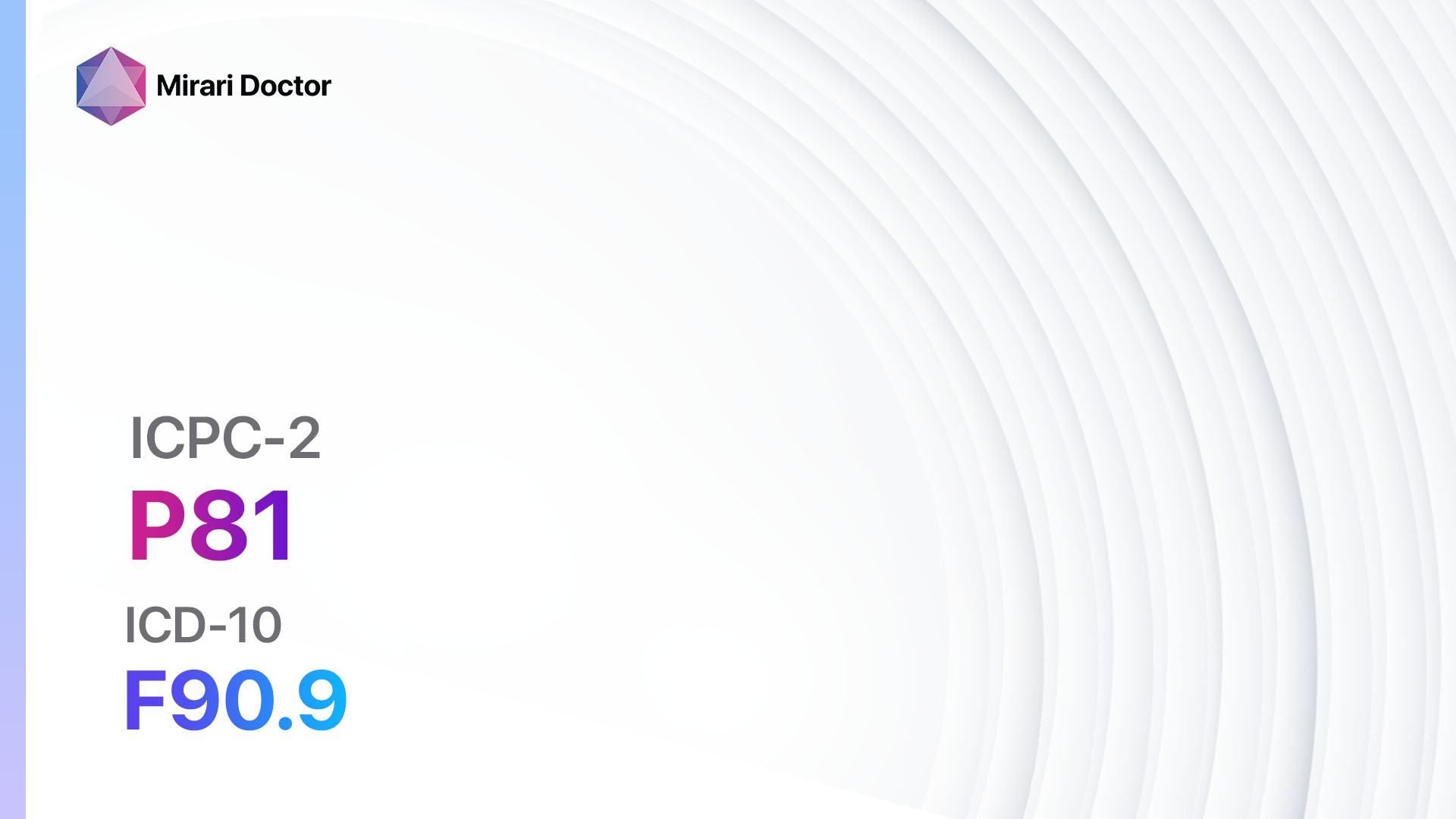
Codes
Symptoms
- Inattention: Difficulty sustaining attention, easily distracted, forgetfulness, difficulty organizing tasks[3].
- Hyperactivity: Excessive fidgeting, difficulty staying seated, excessive talking, difficulty engaging in quiet activities[3].
- Impulsivity: Acting without thinking, interrupting others, difficulty waiting for turns[3].
Causes
- Genetic factors: Hyperkinetic disorder has a strong genetic component, with heritability estimates ranging from 70-80%[4].
- Neurobiological factors: Imbalances in neurotransmitters, such as dopamine and norepinephrine, have been implicated in the development of hyperkinetic disorder[5][6].
- Environmental factors: Prenatal exposure to tobacco smoke, alcohol, or illicit drugs, as well as low birth weight and lead exposure, have been associated with an increased risk of developing hyperkinetic disorder[7][8].
Diagnostic Steps
Medical History
- Obtain a detailed medical history, including information about the patient’s developmental milestones, academic performance, and behavioral problems[9].
- Inquire about the presence of symptoms of inattention, hyperactivity, and impulsivity in different settings (e.g., home, school, work)[9].
- Assess for the presence of comorbid conditions, such as anxiety, depression, and learning disabilities[10].
Physical Examination
- Perform a thorough physical examination to rule out any underlying medical conditions that may be contributing to the symptoms[9].
- Assess for any physical signs associated with hyperkinetic disorder, such as restlessness, excessive movement, or difficulty sitting still[9].
Laboratory Tests
- There are no specific laboratory tests for the diagnosis of hyperkinetic disorder[9].
- However, blood tests may be performed to rule out other medical conditions that may mimic the symptoms of hyperkinetic disorder, such as thyroid dysfunction or iron deficiency[9].
Diagnostic Imaging
- Diagnostic imaging is not routinely used in the diagnosis of hyperkinetic disorder[9].
- However, brain imaging studies, such as MRI or CT scans, may be considered in cases where there is a suspicion of an underlying structural abnormality or neurological disorder[9].
Other Tests
- Additional tests, such as neuropsychological testing or behavioral rating scales, may be used to assess the severity of symptoms and functional impairment associated with hyperkinetic disorder.
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the patient’s response to treatment and adjust the management plan as needed[9].
- Provide education to the patient and their family about hyperkinetic disorder, including its symptoms, treatment options, and strategies for managing symptoms in daily life[9]
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Hyperkinetic disorder:
- Methylphenidate (e.g., Ritalin, Concerta):
- Cost: $30-$200/month.
- Contraindications: Hypersensitivity to methylphenidate, glaucoma, severe anxiety.
- Side effects: Decreased appetite, insomnia, headache.
- Severe side effects: Increased heart rate, high blood pressure, psychiatric symptoms.
- Drug interactions: Monoamine oxidase inhibitors (MAOIs), antihypertensive medications.
- Warning: Regular monitoring of blood pressure and heart rate required.
- Amphetamine (e.g., Adderall, Vyvanse):
- Cost: $30-$200/month.
- Contraindications: Hypersensitivity to amphetamines, advanced arteriosclerosis, hyperthyroidism.
- Side effects: Decreased appetite, dry mouth, irritability.
- Severe side effects: Increased heart rate, high blood pressure, psychiatric symptoms.
- Drug interactions: MAOIs, antihypertensive medications.
- Warning: Regular monitoring of blood pressure and heart rate required.
- Atomoxetine (e.g., Strattera):
- Cost: $100-$300/month.
- Contraindications: Hypersensitivity to atomoxetine, narrow-angle glaucoma, concurrent use of MAOIs.
- Side effects: Upset stomach, decreased appetite, fatigue.
- Severe side effects: Increased heart rate, high blood pressure, liver injury.
- Drug interactions: MAOIs, antihypertensive medications.
- Warning: Regular monitoring of blood pressure and heart rate required.
- Guanfacine (e.g., Intuniv):
- Cost: $100-$300/month.
- Contraindications: Hypersensitivity to guanfacine, severe bradycardia, hypotension.
- Side effects: Drowsiness, fatigue, dry mouth.
- Severe side effects: Low blood pressure, slow heart rate, psychiatric symptoms.
- Drug interactions: Antihypertensive medications, CNS depressants.
- Warning: Regular monitoring of blood pressure and heart rate required.
- Clonidine (e.g., Catapres):
- Cost: $30-$100/month.
- Contraindications: Hypersensitivity to clonidine, severe bradycardia, hypotension.
- Side effects: Drowsiness, dry mouth, constipation.
- Severe side effects: Low blood pressure, slow heart rate, psychiatric symptoms.
- Drug interactions: Antihypertensive medications, CNS depressants.
- Warning: Regular monitoring of blood pressure and heart rate required.
Alternative Drugs:
- Bupropion: An antidepressant that may be used off-label for the treatment of hyperkinetic disorder.
- Guanfacine extended-release: A long-acting formulation of guanfacine that may be used as an alternative to immediate-release guanfacine.
- Desipramine: A tricyclic antidepressant that may be used off-label for the treatment of hyperkinetic disorder.
- Modafinil: A wakefulness-promoting agent that may be used off-label for the treatment of hyperkinetic disorder.
- Pemoline: A stimulant medication that may be used as an alternative to methylphenidate or amphetamine.
Behavioral Interventions:
- Behavioral therapy: Individual or group therapy sessions that focus on teaching patients skills to manage their symptoms and improve their functioning.
- Parent training: Education and support for parents to learn strategies for managing their child’s behavior and promoting positive interactions.
- School-based interventions: Collaboration with teachers and school staff to develop individualized education plans (IEPs) and accommodations to support the child’s learning and behavior in the classroom.
Alternative Interventions
- Neurofeedback: A form of biofeedback that uses real-time displays of brain activity to teach patients self-regulation techniques. Cost: $75-$150 per session.
- Mindfulness meditation: Training in mindfulness techniques to improve attention and reduce impulsivity. Cost: Varies depending on the specific program or instructor.
- Exercise therapy: Regular physical activity has been shown to improve symptoms of hyperkinetic disorder. Cost: Varies depending on the type of exercise and access to facilities.
- Dietary modifications: Some studies suggest that certain dietary changes, such as eliminating artificial food colorings or increasing omega-3 fatty acids, may have a positive impact on symptoms. Cost: Varies depending on the specific dietary modifications.
- Cognitive training: Computer-based programs that target cognitive skills, such as working memory and attention, may help improve symptoms. Cost: Varies depending on the specific program or software.
Lifestyle Interventions
- Establish a structured routine: Consistent daily schedules and routines can help individuals with hyperkinetic disorder manage their time and tasks more effectively.
- Create an organized environment: Minimize distractions and create a clutter-free workspace or living area to promote focus and concentration.
- Break tasks into smaller steps: Breaking down larger tasks into smaller, manageable steps can help individuals with hyperkinetic disorder stay organized and complete tasks more efficiently.
- Use visual aids and reminders: Visual schedules, checklists, and reminders can help individuals with hyperkinetic disorder stay on track and remember important tasks or appointments.
- Encourage regular exercise and physical activity: Engaging in regular physical activity can help reduce hyperactivity and improve overall well-being.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – P81 Hyperkinetic disorder (ICD-10:F90.9)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning:30minutesapprox.$5USD, Evening:30minutesapprox.$5USD | Total Morning:60minutesapprox.$10USD, Lunch:60minutesapprox. $10 USD, Evening:60minutesapprox. $10 USD, | Total Morning:60minutesapprox.$10USD, Lunch:60minutesapprox. $10 USD, Evening:60minutesapprox. $10 USD, |
| Usualtreatmentfor7-60daysapprox.$70USD–$600USD | Usualtreatmentfor6-8weeksapprox.$1,260USD–$1,680USD | Usualtreatmentfor3-6monthsapprox.$2,700USD–$5,400USD |
 |
|
Use the Mirari Cold Plasma device to treat Hyperkinetic disorder effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Hyperkinetic disorder. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington, VA: American Psychiatric Publishing; 2013.
- Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016 Mar 19;387(10024):1240-1250. doi: 10.1016/S0140-6736(15)00238-X.
- National Institute for Health and Care Excellence. Attention deficit hyperactivity disorder: diagnosis and management. NICE guideline [NG87]. 2018 Mar 14.
- Faraone SV, Larsson H. Genetics of attention deficit hyperactivity disorder. Mol Psychiatry. 2019 Apr;24(4):562-575. doi: 10.1038/s41380-018-0070-0.
- Sharma A, Couture J. A review of the pathophysiology, etiology, and treatment of attention-deficit hyperactivity disorder (ADHD). Ann Pharmacother. 2014 Feb;48(2):209-25. doi: 10.1177/1060028013510699.
- Tripp G, Wickens JR. Neurobiology of ADHD. Neuropharmacology. 2009 Dec;57(7-8):579-89. doi: 10.1016/j.neuropharm.2009.07.026.
- Froehlich TE, Anixt JS, Loe IM, Chirdkiatgumchai V, Kuan L, Gilman RC. Update on environmental risk factors for attention-deficit/hyperactivity disorder. Curr Psychiatry Rep. 2011 Oct;13(5):333-44. doi: 10.1007/s11920-011-0221-3.
- Sciberras E, Mulraney M, Silva D, Coghill D. Prenatal Risk Factors and the Etiology of ADHD-Review of Existing Evidence. Curr Psychiatry Rep. 2017 Jan;19(1):1. doi: 10.1007/s11920-017-0753-2.
- Wolraich ML, Hagan JF Jr, Allan C, et al. Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. Pediatrics. 2019 Oct;144(4):e20192528. doi: 10.1542/peds.2019-2528.
- Reale L, Bartoli B, Cartabia M, et al. Comorbidity prevalence and treatment outcome in children and adolescents with ADHD. Eur Child Adolesc Psychiatry. 2017 Dec;26(12):1443-1457. doi: 10.1007/s00787-017-1005-z.
Related articles
Made in USA