Introduction
Schizophrenia is a chronic mental disorder characterized by abnormal social behavior, disorganized thinking, and hallucinations or delusions[1]. It affects approximately 1% of the population worldwide and can have a significant impact on the individual’s quality of life[2]. The aim of this guide is to provide an overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for schizophrenia.
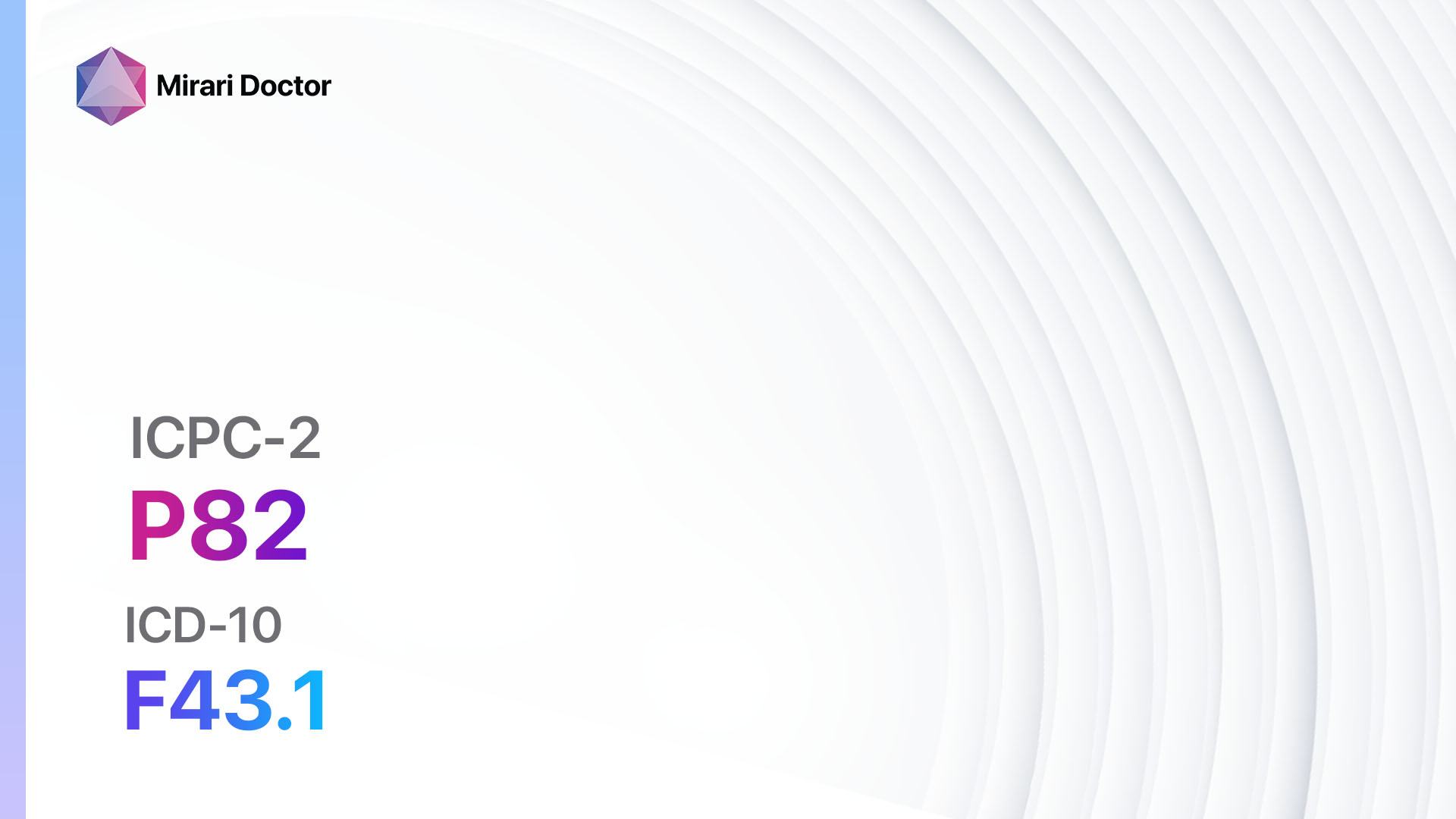
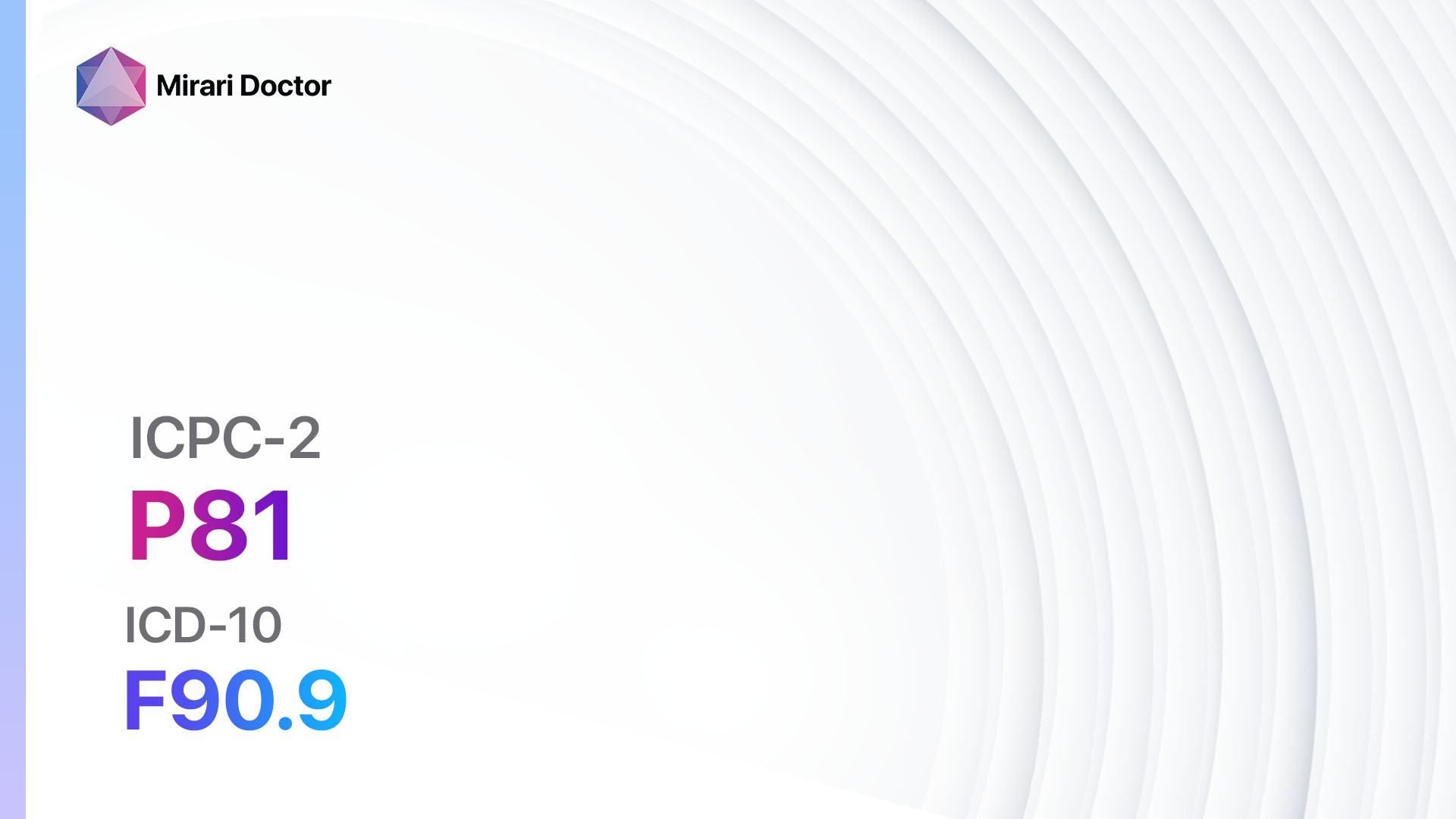
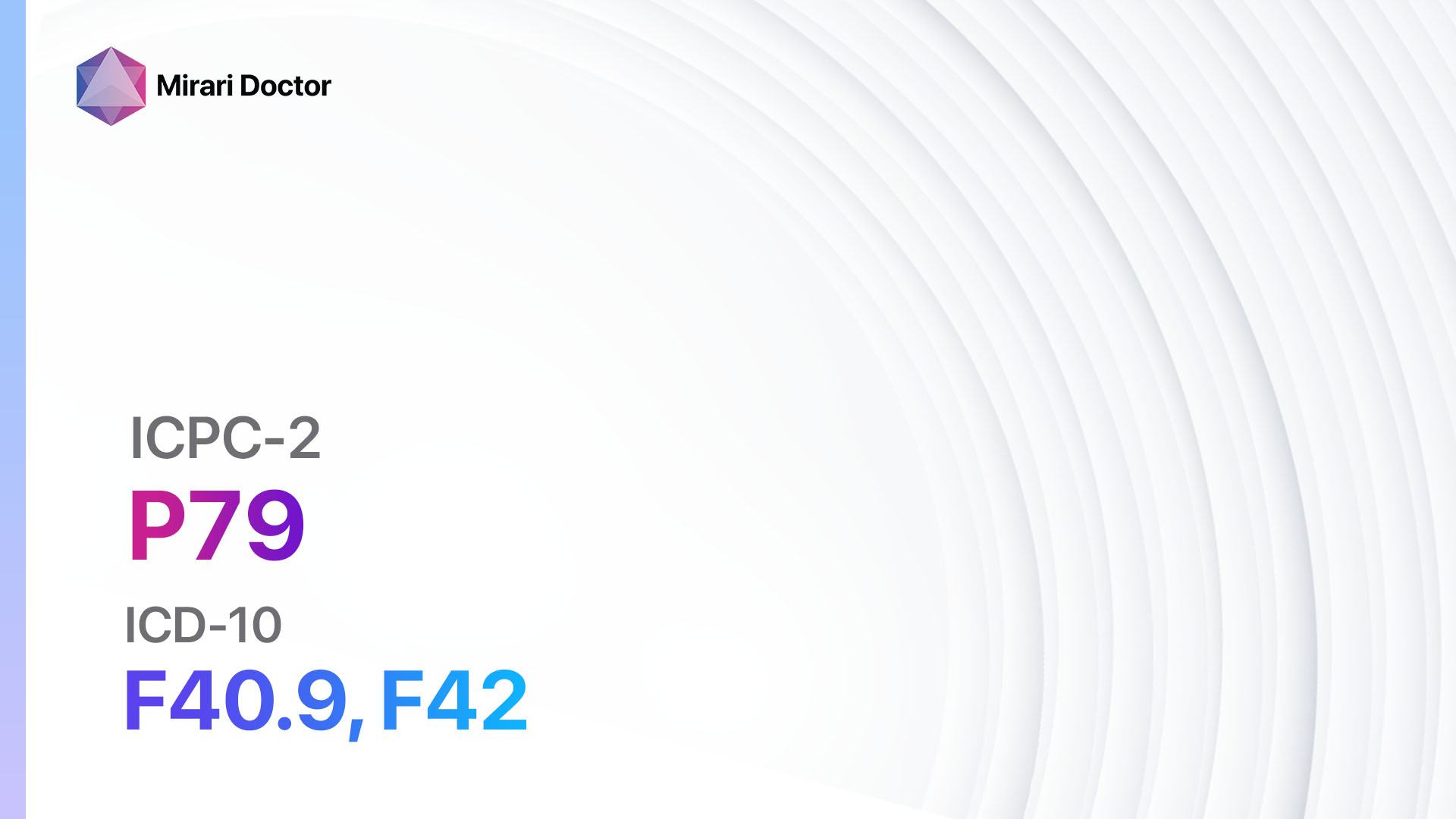
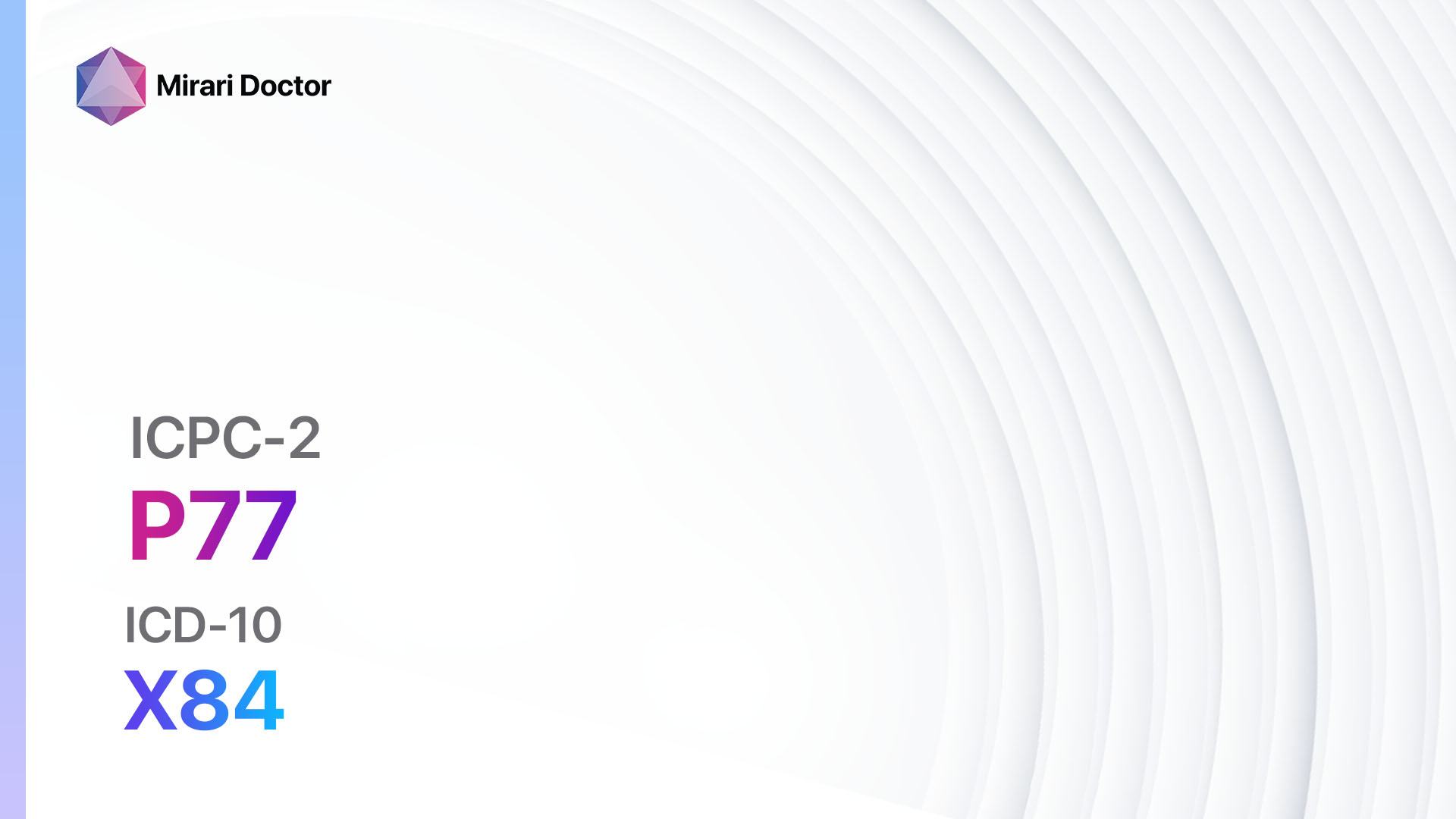
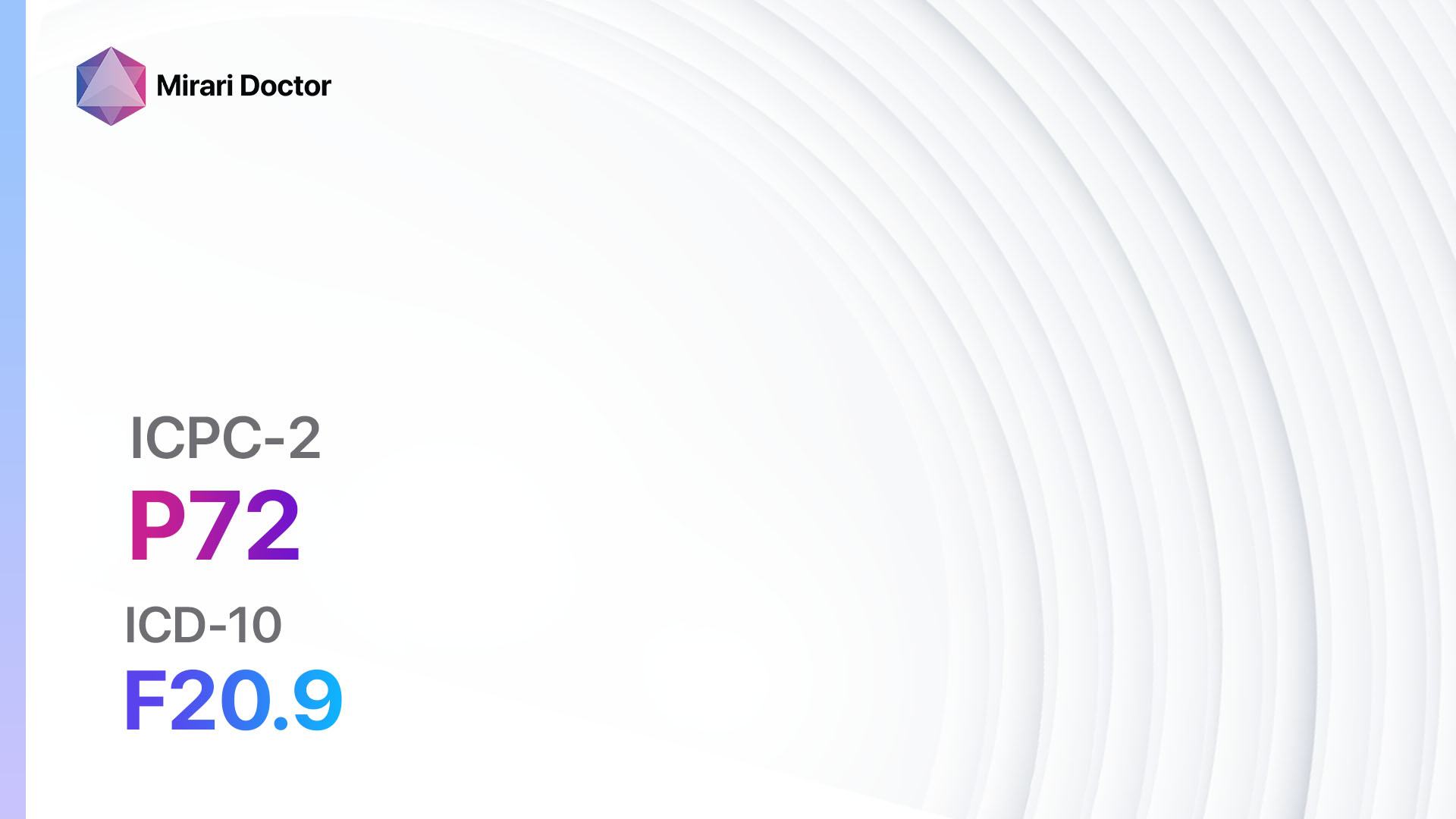
Codes
Symptoms
- Delusions: False beliefs that are not based in reality, such as believing that someone is trying to harm them or that they have special powers[3].
- Hallucinations: Seeing or hearing things that are not actually present, such as hearing voices or seeing imaginary people[4].
- Disorganized speech: Incoherent or illogical speech patterns that are difficult to understand[5].
- Disorganized behavior: Unpredictable or inappropriate behavior, such as dressing inappropriately for the weather or engaging in repetitive movements[6].
- Negative symptoms: Lack of motivation, decreased emotional expression, and reduced ability to experience pleasure[7].
Causes
- Genetic factors: Schizophrenia has been found to have a genetic component, with a higher risk in individuals who have a family history of the disorder[8].
- Environmental factors: Prenatal exposure to infections, complications during birth, and exposure to certain toxins or drugs during adolescence or early adulthood may increase the risk of developing schizophrenia[9].
- Neurochemical imbalances: Imbalances in certain neurotransmitters, such as dopamine and glutamate, may contribute to the development of schizophrenia[10].
- Brain abnormalities: Structural and functional abnormalities in the brain, particularly in the frontal cortex and limbic system, have been observed in individuals with schizophrenia.
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the onset, duration, and severity.
- Assess the patient’s family history of mental illness, particularly schizophrenia.
- Inquire about any history of substance abuse or exposure to toxins.
- Evaluate the patient’s social and occupational functioning.
Physical Examination
- Perform a general physical examination to rule out any underlying medical conditions that may be causing or contributing to the symptoms.
- Assess vital signs, including blood pressure, heart rate, and temperature.
- Evaluate neurological function, including coordination, reflexes, and sensory perception.
Laboratory Tests
- Blood tests: These may be used to rule out other medical conditions that can mimic the symptoms of schizophrenia, such as thyroid disorders or vitamin deficiencies.
- Drug screening: To identify any substance abuse that may be contributing to the symptoms.
- Genetic testing: Although not routinely done, genetic testing may be considered in certain cases to identify any specific genetic abnormalities associated with schizophrenia.
Diagnostic Imaging
- Magnetic Resonance Imaging (MRI): This imaging modality can help identify any structural abnormalities in the brain that may be associated with schizophrenia.
- Functional MRI (fMRI): This specialized MRI technique can assess brain activity and identify any functional abnormalities.
- Positron Emission Tomography (PET) scan: PET scans can measure brain activity and identify any abnormalities in neurotransmitter function.
Other Tests
- Neuropsychological testing: These tests can assess cognitive function, memory, attention, and executive function, which may be impaired in individuals with schizophrenia.
- Electroencephalogram (EEG): This test measures electrical activity in the brain and can help identify any abnormalities.
- Eye movement testing: Abnormal eye movements have been observed in individuals with schizophrenia and can be assessed using specialized eye-tracking technology.
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the patient’s symptoms and response to treatment.
- Provide education to the patient and their family about schizophrenia, including the nature of the disorder, treatment options, and strategies for managing symptoms.
- Encourage the patient to engage in support groups or therapy to help cope with the challenges of living with schizophrenia.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Schizophrenia:
- Risperidone:
- Cost: $10-$100/month.
- Contraindications: Hypersensitivity to risperidone, severe CNS depression.
- Side effects: Drowsiness, weight gain, extrapyramidal symptoms.
- Severe side effects: Neuroleptic malignant syndrome, tardive dyskinesia.
- Drug interactions: Other antipsychotic medications, CNS depressants.
- Warning: Regular monitoring of blood pressure and blood glucose levels required.
- Olanzapine:
- Cost: $10-$100/month.
- Contraindications: Hypersensitivity to olanzapine, severe CNS depression.
- Side effects: Weight gain, drowsiness, metabolic changes.
- Severe side effects: Neuroleptic malignant syndrome, tardive dyskinesia.
- Drug interactions: Other antipsychotic medications, CNS depressants.
- Warning: Regular monitoring of blood pressure and blood glucose levels required.
- Quetiapine:
- Cost: $10-$100/month.
- Contraindications: Hypersensitivity to quetiapine, severe CNS depression.
- Side effects: Drowsiness, dizziness, weight gain.
- Severe side effects: Neuroleptic malignant syndrome, tardive dyskinesia.
- Drug interactions: Other antipsychotic medications, CNS depressants.
- Warning: Regular monitoring of blood pressure and blood glucose levels required.
- Aripiprazole:
- Cost: $10-$100/month.
- Contraindications: Hypersensitivity to aripiprazole, severe CNS depression.
- Side effects: Restlessness, headache, nausea.
- Severe side effects: Neuroleptic malignant syndrome, tardive dyskinesia.
- Drug interactions: Other antipsychotic medications, CNS depressants.
- Warning: Regular monitoring of blood pressure and blood glucose levels required.
- Clozapine:
- Cost: $100-$500/month.
- Contraindications: Hypersensitivity to clozapine, severe CNS depression.
- Side effects: Drowsiness, weight gain, hypersalivation.
- Severe side effects: Agranulocytosis, myocarditis.
- Drug interactions: Other antipsychotic medications, CNS depressants.
- Warning: Regular monitoring of blood counts required.
Alternative Drugs:
- Ziprasidone: May be used as an alternative to the above medications.
- Lurasidone: May be used as an alternative to the above medications.
- Paliperidone: May be used as an alternative to the above medications.
- Asenapine: May be used as an alternative to the above medications.
- Iloperidone: May be used as an alternative to the above medications.
Psychosocial Interventions:
- Individual therapy: Cognitive-behavioral therapy (CBT) or supportive therapy can help individuals with schizophrenia manage their symptoms and improve their functioning.
- Family therapy: Involving the patient’s family in therapy can help improve communication, reduce stress, and enhance the patient’s support system.
- Social skills training: This type of therapy focuses on improving social and interpersonal skills, which can be impaired in individuals with schizophrenia.
- Vocational rehabilitation: Assisting individuals with schizophrenia in finding and maintaining employment can improve their overall functioning and quality of life.
- Assertive community treatment (ACT): This comprehensive approach involves a multidisciplinary team providing ongoing support and treatment to individuals with schizophrenia in their community.
Alternative Interventions
- Art therapy: Engaging in creative activities, such as painting or drawing, can provide a therapeutic outlet for individuals with schizophrenia. Cost: $20-$50 per session.
- Music therapy: Listening to or creating music can help reduce stress and improve mood in individuals with schizophrenia. Cost: $20-$50 per session.
- Yoga and meditation: These practices can help individuals with schizophrenia manage stress, improve concentration, and promote overall well-being. Cost: $10-$20 per session.
- Acupuncture: May help reduce symptoms of schizophrenia and improve overall well-being. Cost: $60-$120 per session.
- Herbal supplements: Some herbal supplements, such as St. John’s wort or passionflower, may have potential benefits for reducing anxiety or improving sleep. Cost: Varies depending on the specific supplement.
Lifestyle Interventions
- Regular exercise: Engaging in physical activity can help reduce symptoms of schizophrenia, improve mood, and enhance overall well-being. Cost: Varies depending on the chosen activity (e.g., gym membership, sports equipment).
- Healthy diet: Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall mental and physical health. Cost: Varies depending on food choices.
- Adequate sleep: Getting enough sleep is important for individuals with schizophrenia to help manage symptoms and improve overall functioning. Cost: Varies depending on sleep aids or therapies used.
- Stress management techniques: Learning and practicing stress management techniques, such as deep breathing exercises or mindfulness, can help individuals with schizophrenia cope with stress and reduce symptom severity. Cost: Varies depending on chosen techniques or therapies.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. It is recommended to consult with healthcare professionals for personalized treatment options and cost estimates.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – P72 Schizophrenia (ICD-10:F20.9)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 30 minutes approx. $5 USD, Evening: 30 minutes approx. $5 USD |
Total Morning: 60 minutes approx. $10 USD, Lunch: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD, |
Total Morning: 60 minutes approx. $10 USD, Lunch: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD, |
| Usual treatment for 7-60 days approx. $70 USD – $600 USD | Usual treatment for 6-8 weeks approx. $1,260 USD – $1,680 USD |
Usual treatment for 3-6 months approx. $2,700 USD – $5,400 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Schizophrenia effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Schizophrenia. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
- Charlson, F. J., Ferrari, A. J., Santomauro, D. F., Diminic, S., Stockings, E., Scott, J. G., McGrath, J. J., & Whiteford, H. A. (2018). Global Epidemiology and Burden of Schizophrenia: Findings From the Global Burden of Disease Study 2016. Schizophrenia Bulletin, 44(6), 1195–1203. https://doi.org/10.1093/schbul/sby058
- Tandon, R., Gaebel, W., Barch, D. M., Bustillo, J., Gur, R. E., Heckers, S., Malaspina, D., Owen, M. J., Schultz, S., Tsuang, M., Van Os, J., & Carpenter, W. (2013). Definition and description of schizophrenia in the DSM-5. Schizophrenia Research, 150(1), 3–10. https://doi.org/10.1016/j.schres.2013.05.028
- Waters, F., Collerton, D., Ffytche, D. H., Jardri, R., Pins, D., Dudley, R., Blom, J. D., Mosimann, U. P., Eperjesi, F., Ford, S., & Larøi, F. (2014). Visual hallucinations in the psychosis spectrum and comparative information from neurodegenerative disorders and eye disease. Schizophrenia Bulletin, 40(Suppl_4), S233–S245. https://doi.org/10.1093/schbul/sbu036
- Covington, M. A., He, C., Brown, C., Naçi, L., McClain, J. T., Fjordbak, B. S., Semple, J., & Brown, J. (2005). Schizophrenia and the structure of language: The linguist’s view. Schizophrenia Research, 77(1), 85–98. https://doi.org/10.1016/j.schres.2005.01.016
- Walther, S., & Strik, W. (2012). Motor Symptoms and Schizophrenia. Neuropsychobiology, 66(2), 77–92. https://doi.org/10.1159/000339456
- Kirkpatrick, B., Fenton, W. S., Carpenter, W. T., & Marder, S. R. (2006). The NIMH-MATRICS Consensus Statement on Negative Symptoms. Schizophrenia Bulletin, 32(2), 214–219. https://doi.org/10.1093/schbul/sbj053
- Sullivan, P. F., Kendler, K. S., & Neale, M. C. (2003). Schizophrenia as a Complex Trait: Evidence from a Meta-analysis of Twin Studies. Archives of General Psychiatry, 60(12), 1187. https://doi.org/10.1001/archpsyc.60.12.1187
- Brown, A. S. (2011). The environment and susceptibility to schizophrenia. Progress in Neurobiology, 93(1), 23–58. https://doi.org/10.1016/j.pneurobio.2010.09.003
- Howes, O. D., & Kapur, S. (2009). The Dopamine Hypothesis of Schizophrenia: Version III–The Final Common Pathway. Schizophrenia Bulletin, 35(3), 549–562. https://doi.org/10.1093/schbul/sbp006
Related articles
Made in USA