Introduction
Dementia is a progressive neurodegenerative disorder characterized by a decline in cognitive function, memory loss, and impaired daily functioning[1]. It is a significant condition that affects millions of individuals worldwide, leading to a substantial burden on patients, caregivers, and healthcare systems[2]. The aim of this guide is to provide a comprehensive overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for dementia.
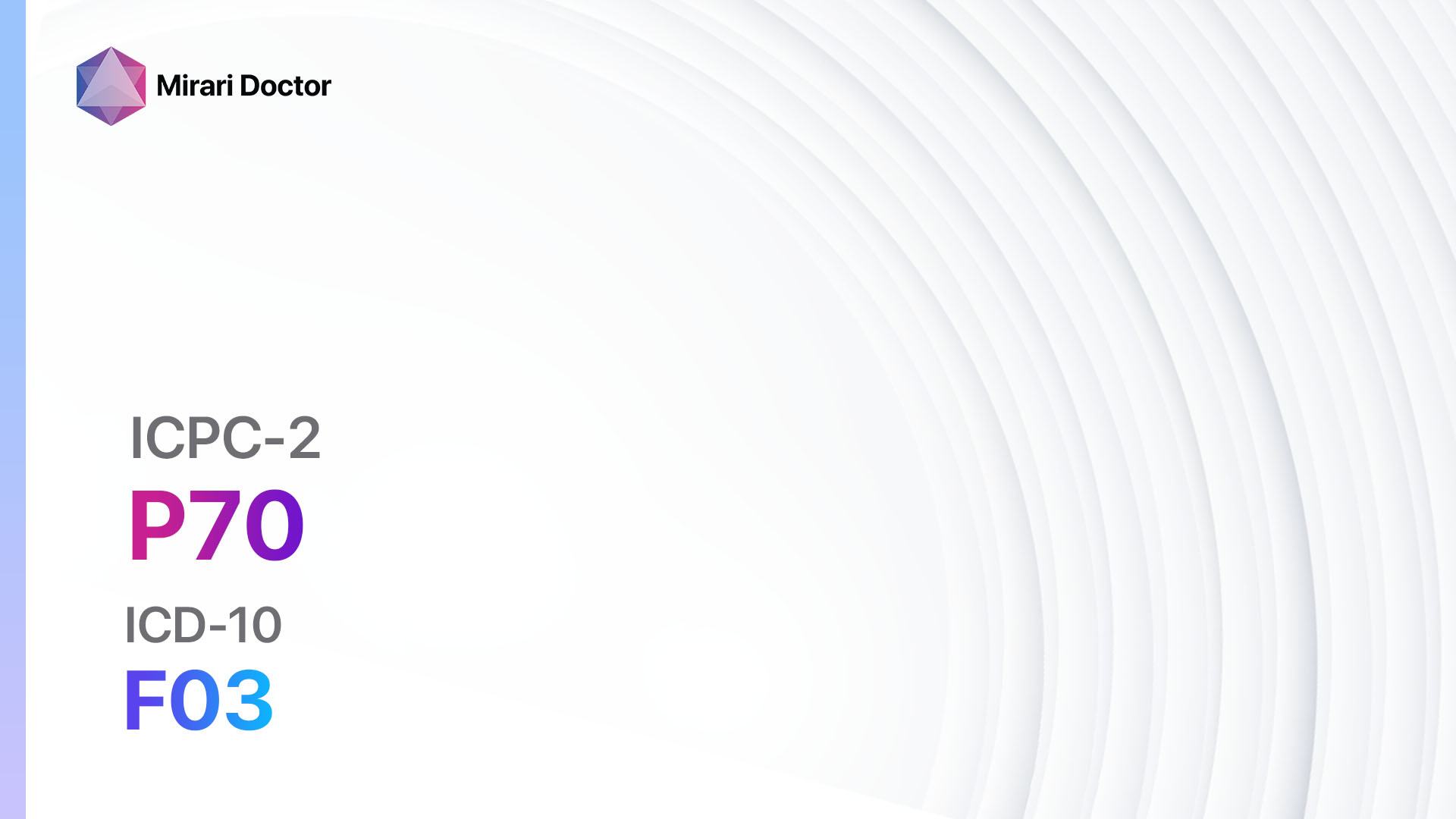
Codes
Symptoms
- Memory loss: Difficulty remembering recent events, names, or conversations[3].
- Difficulty with language: Struggling to find the right words or understand others[4].
- Impaired judgment and decision-making: Poor judgment and decision-making abilities[5].
- Impaired visual perception: Difficulty with spatial awareness and visual recognition[6].
- Changes in mood and behavior: Depression, anxiety, irritability, and agitation[7].
- Loss of initiative: Lack of motivation and withdrawal from social activities[8].
Causes
- Alzheimer’s disease: The most common cause of dementia, characterized by the accumulation of amyloid plaques and neurofibrillary tangles in the brain[9].
- Vascular dementia: Caused by reduced blood flow to the brain due to small strokes or other vascular conditions[10].
- Lewy body dementia: Characterized by the presence of abnormal protein deposits called Lewy bodies in the brain.
- Frontotemporal dementia: Involves the degeneration of the frontal and temporal lobes of the brain, leading to changes in behavior and personality.
- Mixed dementia: A combination of two or more types of dementia.
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, their duration, and progression.
- Identify any risk factors for dementia, such as age, family history, and cardiovascular disease.
- Assess the patient’s medical conditions, including hypertension, diabetes, and history of stroke.
- Evaluate the patient’s medications, as certain drugs can contribute to cognitive impairment.
Physical Examination
- Perform a thorough physical examination, including a neurological assessment.
- Look for signs of neurological abnormalities, such as muscle weakness or abnormal reflexes.
- Assess the patient’s gait and balance, as these can be affected in certain types of dementia.
- Check for signs of other medical conditions that may contribute to cognitive impairment, such as thyroid dysfunction or vitamin deficiencies.
Laboratory Tests
- Complete blood count (CBC): To rule out anemia or infections that may cause cognitive impairment.
- Thyroid function tests: To assess thyroid hormone levels, as abnormalities can contribute to cognitive decline.
- Vitamin B12 and folate levels: Deficiencies in these vitamins can lead to cognitive impairment.
- Liver and kidney function tests: To evaluate the overall health of the patient and rule out any underlying conditions.
- Lipid profile: To assess the patient’s cholesterol levels, as high cholesterol is a risk factor for vascular dementia.
Diagnostic Imaging
- Magnetic resonance imaging (MRI): To visualize the brain and identify any structural abnormalities or signs of atrophy.
- Computed tomography (CT) scan: To assess the brain for signs of stroke, tumors, or other abnormalities.
- Positron emission tomography (PET) scan: To detect changes in brain metabolism and identify areas of decreased activity.
- Single-photon emission computed tomography (SPECT) scan: To evaluate blood flow in the brain and identify areas of reduced perfusion.
Other Tests
- Neuropsychological testing: Assess cognitive function, memory, attention, and executive function.
- Genetic testing: Identify any genetic mutations associated with familial forms of dementia.
- Electroencephalogram (EEG): Evaluate brain wave patterns and detect any abnormalities.
- Cerebrospinal fluid analysis: Assess the levels of amyloid beta and tau proteins, which are associated with Alzheimer’s disease.
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the progression of symptoms and adjust treatment as needed.
- Provide education to the patient and their caregivers about the nature of dementia, available treatments, and strategies for managing symptoms.
- Offer support resources, such as support groups or counseling services, to help patients and caregivers cope with the challenges of dementia.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Dementia:
- Cholinesterase inhibitors (e.g., Donepezil, Rivastigmine, Galantamine):
- Cost: Donepezil – $10-$100/month, Rivastigmine – $10-$200/month, Galantamine – $10-$200/month.
- Contraindications: Hypersensitivity to the drug.
- Side effects: Nausea, vomiting, diarrhea, loss of appetite.
- Severe side effects: Bradycardia, syncope, seizures.
- Drug interactions: Anticholinergic drugs, NSAIDs.
- Warning: Regular monitoring of liver function may be required.
- Memantine:
- Cost: $10-$200/month.
- Contraindications: Hypersensitivity to the drug.
- Side effects: Dizziness, headache, constipation.
- Severe side effects: Hallucinations, seizures, Stevens-Johnson syndrome.
- Drug interactions: Sodium bicarbonate, carbonic anhydrase inhibitors.
- Warning: Dosage adjustment may be required in patients with renal impairment.
- Antidepressants (e.g., Sertraline, Citalopram):
- Cost: $10-$100/month.
- Contraindications: Hypersensitivity to the drug.
- Side effects: Nausea, dry mouth, drowsiness.
- Severe side effects: Suicidal thoughts, serotonin syndrome.
- Drug interactions: Monoamine oxidase inhibitors, other serotonergic drugs.
- Warning: Close monitoring for changes in mood or behavior is necessary.
- Antipsychotics (e.g., Risperidone, Quetiapine):
- Cost: $10-$200/month.
- Contraindications: Hypersensitivity to the drug, dementia-related psychosis.
- Side effects: Sedation, weight gain, extrapyramidal symptoms.
- Severe side effects: Neuroleptic malignant syndrome, tardive dyskinesia.
- Drug interactions: Other antipsychotics, anticholinergic drugs.
- Warning: Increased risk of mortality in elderly patients with dementia-related psychosis.
- Anxiolytics (e.g., Lorazepam, Alprazolam):
- Cost: $10-$100/month.
- Contraindications: Hypersensitivity to the drug, narrow-angle glaucoma.
- Side effects: Sedation, dizziness, confusion.
- Severe side effects: Respiratory depression, paradoxical reactions.
- Drug interactions: Other CNS depressants, opioids.
- Warning: Increased risk of falls and cognitive impairment in elderly patients.
Alternative Drugs:
- Ginkgo biloba: An herbal supplement that may improve cognitive function. Cost: $10-$30/month.
- Omega-3 fatty acids: Found in fish oil supplements, may have neuroprotective effects. Cost: $10-$30/month.
- Vitamin E: Antioxidant supplement that may slow the progression of dementia. Cost: $10-$30/month.
- Huperzine A: An herbal supplement that may improve memory and cognitive function. Cost: $10-$30/month.
- Curcumin: Found in turmeric, may have anti-inflammatory and neuroprotective effects. Cost: $10-$30/month.
Surgical Procedures:
- Deep brain stimulation (DBS): Involves the implantation of electrodes in the brain to stimulate specific regions and improve cognitive function. Cost: $50,000 to $100,000.
- Ventriculoperitoneal shunt: A surgical procedure to divert excess cerebrospinal fluid from the brain to the abdomen, reducing pressure and improving symptoms. Cost: $20,000 to $50,000.
Alternative Interventions
- Cognitive stimulation therapy: Structured activities and exercises to improve cognitive function. Cost: $50-$100 per session.
- Music therapy: Listening to or playing music to improve mood and cognitive function. Cost: $50-$100 per session.
- Art therapy: Engaging in artistic activities to promote self-expression and cognitive stimulation. Cost: $50-$100 per session.
- Pet therapy: Interacting with animals to reduce anxiety and improve overall well-being. Cost: Varies depending on the specific therapy provider.
- Mindfulness meditation: Practicing mindfulness techniques to reduce stress and improve cognitive function. Cost: $0-$50 per session.
Lifestyle Interventions
- Regular physical exercise: Engaging in aerobic exercise, such as walking or swimming, to improve cardiovascular health and cognitive function. Cost: $0-$100 per month.
- Healthy diet: Following a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to support brain health. Cost: Varies depending on food choices.
- Mental stimulation: Engaging in activities that challenge the brain, such as puzzles, reading, or learning a new skill. Cost: Varies depending on the activity.
- Social engagement: Maintaining social connections and participating in social activities to promote cognitive function. Cost: Varies depending on the activity.
- Adequate sleep: Ensuring sufficient sleep duration and quality to support brain health. Cost: $0.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. It is recommended to consult with healthcare professionals for accurate cost estimates and personalized treatment plans.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – P70 Dementia (ICD-10:F03)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 30 minutes approx. $5 USD, Evening: 30 minutes approx. $5 USD |
Total Morning: 60 minutes approx. $10 USD, Lunch: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD, |
Total Morning: 60 minutes approx. $10 USD, Lunch: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD, |
| Usual treatment for 7-60 days approx. $70 USD – $600 USD | Usual treatment for 6-8 weeks approx. $1,260 USD – $1,680 USD |
Usual treatment for 3-6 months approx. $2,700 USD – $5,400 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Dementia effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Dementia. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413-446. doi:10.1016/S0140-6736(20)30367-6
- World Health Organization. Dementia. Published September 21, 2020. Accessed April 12, 2023. https://www.who.int/news-room/fact-sheets/detail/dementia
- Jahn H. Memory loss in Alzheimer’s disease. Dialogues Clin Neurosci. 2013;15(4):445-454. doi:10.31887/DCNS.2013.15.4/hjahn
- Kirshner HS. Frontotemporal dementia and primary progressive aphasia, a review. Neuropsychiatr Dis Treat. 2014;10:1045-1055. Published 2014 Jun 17. doi:10.2147/NDT.S38821
- Gleichgerrcht E, Ibáñez A, Roca M, Torralva T, Manes F. Decision-making cognition in neurodegenerative diseases. Nat Rev Neurol. 2010;6(11):611-623. doi:10.1038/nrneurol.2010.148
- Possin KL. Visual spatial cognition in neurodegenerative disease. Neurocase. 2010;16(6):466-487. doi:10.1080/13554791003730600
- Lyketsos CG, Carrillo MC, Ryan JM, et al. Neuropsychiatric symptoms in Alzheimer’s disease. Alzheimers Dement. 2011;7(5):532-539. doi:10.1016/j.jalz.2011.05.2410
- Landes AM, Sperry SD, Strauss ME, Geldmacher DS. Apathy in Alzheimer’s disease. J Am Geriatr Soc. 2001;49(12):1700-1707. doi:10.1046/j.1532-5415.2001.49282.x
- Scheltens P, Blennow K, Breteler MM, et al. Alzheimer’s disease. Lancet. 2016;388(10043):505-517. doi:10.1016/S0140-6736(15)01124-1
- Iadecola C. The pathobiology of vascular dementia. Neuron. 2013;80(4):844-866. doi:10.1016/j.neuron.2013.10.008
Related articles
Made in USA