Introduction
Osteoporosis is a condition characterized by low bone density and increased risk of fractures. It is a significant health concern, especially among older individuals, as it can lead to pain, disability, and decreased quality of life.[1] The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of osteoporosis.
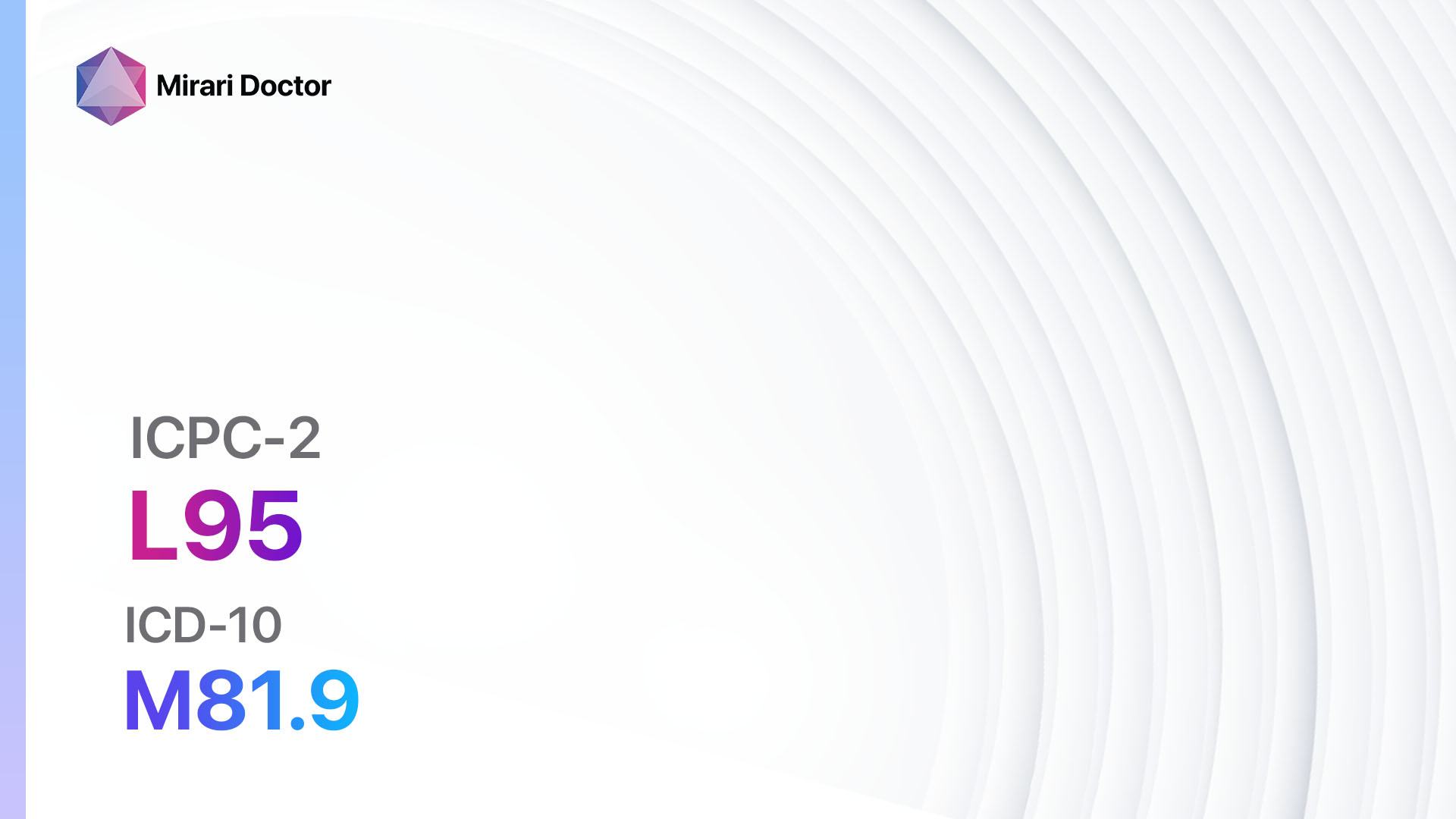
Codes
Symptoms
- Fractures: Osteoporosis increases the risk of fractures, especially in the spine, hip, and wrist.
- Back pain: Compression fractures in the spine can cause chronic back pain.
- Loss of height: Osteoporosis can lead to a gradual loss of height over time.
- Stooped posture: Compression fractures in the spine can result in a stooped posture.[3]
Causes
- Aging: Bone density naturally decreases with age, making older individuals more susceptible to osteoporosis.
- Hormonal changes: Decreased estrogen levels in women after menopause and decreased testosterone levels in men can contribute to bone loss.
- Lack of physical activity: Inactive individuals are at a higher risk of developing osteoporosis.
- Poor nutrition: Inadequate intake of calcium and vitamin D can weaken bones.
- Smoking and excessive alcohol consumption: These habits can negatively impact bone health.[4]
Diagnostic Steps
Medical History
- Gather information about the patient’s age, gender, and menopausal status (for women).
- Assess the patient’s risk factors for osteoporosis, such as family history, previous fractures, and medical conditions (e.g., rheumatoid arthritis, hyperthyroidism).
- Inquire about the patient’s lifestyle habits, including physical activity levels, smoking, and alcohol consumption.
- Evaluate the patient’s symptoms, such as fractures, back pain, loss of height, and stooped posture.[5]
Physical Examination
- Perform a thorough physical examination, paying attention to signs of osteoporosis, such as loss of height, stooped posture, and tenderness over the spine.
- Assess the patient’s overall musculoskeletal health, including joint mobility and muscle strength.[6]
Laboratory Tests
- Dual-energy X-ray absorptiometry (DXA): This is the gold standard test for diagnosing osteoporosis. It measures bone mineral density (BMD) and compares it to the average BMD of young adults.
- Blood tests: Measure levels of calcium, vitamin D, parathyroid hormone, and other markers of bone turnover.[7]
Diagnostic Imaging
- X-rays: Can detect fractures and evaluate the severity of osteoporosis.
- Quantitative ultrasound (QUS): Measures bone density using sound waves.
- CT scans: Provide detailed images of the spine and other bones.[8]
Other Tests
- Vertebral fracture assessment (VFA): A specialized X-ray technique that focuses on the spine to detect vertebral fractures.
- Bone turnover markers: Blood or urine tests that measure the rate of bone remodeling.[9]
Follow-up and Patient Education
- Schedule regular follow-up visits to monitor the patient’s response to treatment and adjust management strategies if necessary.
- Educate the patient about the importance of lifestyle modifications, such as regular weight-bearing exercise, a balanced diet rich in calcium and vitamin D, and smoking cessation.
- Provide information about the potential benefits and risks of pharmacological interventions.[10]
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Osteoporosis:
- Bisphosphonates (e.g., Alendronate, Risedronate, Ibandronate):
- Cost: Generic versions can be $10-$100/month.
- Contraindications: Hypersensitivity, severe kidney disease.
- Side effects: Upset stomach, heartburn, muscle pain.
- Severe side effects: Osteonecrosis of the jaw, atypical fractures.
- Drug interactions: Calcium supplements, antacids.
- Warning: Should be taken with a full glass of water on an empty stomach.
- Selective estrogen receptor modulators (SERMs) (e.g., Raloxifene):
- Cost: $50-$200/month.
- Contraindications: History of blood clots, pregnancy.
- Side effects: Hot flashes, leg cramps.
- Severe side effects: Increased risk of blood clots, stroke.
- Drug interactions: Warfarin, hormone replacement therapy.
- Warning: Regular monitoring of bone density and breast health is required.
- Calcitonin (e.g., Calcitonin salmon):
- Cost: $100-$300/month.
- Contraindications: Hypersensitivity, allergy to salmon.
- Side effects: Nasal irritation, flushing.
- Severe side effects: Allergic reactions, increased risk of cancer.
- Drug interactions: None reported.
- Warning: Long-term use may decrease effectiveness.
- Teriparatide:
- Cost: $3,000-$4,000/month.
- Contraindications: Paget’s disease, bone cancer.
- Side effects: Nausea, dizziness, leg cramps.
- Severe side effects: Increased risk of bone cancer.
- Drug interactions: None reported.
- Warning: Limited to a maximum of 2 years of treatment.
- Denosumab:
- Cost: $1,000-$1,500/month.
- Contraindications: Hypocalcemia, pregnancy.
- Side effects: Back pain, joint pain.
- Severe side effects: Increased risk of infections, skin reactions.
- Drug interactions: None reported.
- Warning: Regular monitoring of calcium levels is required.
Alternative Drugs:
- Hormone replacement therapy (HRT): Estrogen therapy can help prevent bone loss in postmenopausal women. Cost: $20-$100/month.
- Raloxifene: A SERM that can also be used for the prevention and treatment of breast cancer. Cost: $50-$200/month.
- Calcium and vitamin D supplements: Essential for maintaining bone health. Cost: $10-$50/month.
- Strontium ranelate: Stimulates bone formation and inhibits bone resorption. Cost: $100-$200/month.
- Parathyroid hormone analogs: An alternative to teriparatide for severe osteoporosis. Cost: $3,000-$4,000/month.
Surgical Procedures:
- Vertebroplasty and kyphoplasty: Minimally invasive procedures to stabilize fractured vertebrae. Cost: $10,000-$20,000.
- Spinal fusion surgery: Recommended for severe spinal deformities caused by osteoporosis. Cost: $50,000-$100,000.
Alternative Interventions
- Acupuncture: May help reduce pain and improve overall well-being. Cost: $60-$120 per session.
- Yoga: Can improve balance, flexibility, and strength. Cost: $10-$20 per class.
- Tai chi: A low-impact exercise that can improve balance and reduce the risk of falls. Cost: $10-$20 per class.
- Pilates: Focuses on core strength and flexibility. Cost: $10-$30 per class.
- Herbal supplements: Some herbs, such as red clover and black cohosh, may have potential benefits for bone health. Cost: Varies depending on the specific supplement.
Lifestyle Interventions
- Regular weight-bearing exercise: Walking, jogging, dancing, and weightlifting can help improve bone density. Cost: Varies depending on the chosen activity.
- Balanced diet rich in calcium and vitamin D: Include dairy products, leafy greens, and fortified foods in the diet. Cost: Varies depending on food choices.
- Smoking cessation: Quitting smoking can improve bone health and reduce the risk of fractures. Cost: Varies depending on the chosen smoking cessation method.
- Limit alcohol consumption: Excessive alcohol intake can negatively impact bone health. Cost: Varies depending on alcohol consumption habits.
- Fall prevention strategies: Remove hazards at home, use assistive devices, and improve lighting to reduce the risk of falls. Cost: Varies depending on necessary modifications.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – L95 Osteoporosis (ICD-10:M81.9)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 9 (Arthritis) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 9 (Arthritis) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 9 (Arthritis) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Osteoporosis effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Osteoporosis. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Sözen T, Özışık L, Başaran NC. An overview and management of osteoporosis. Eur J Rheumatol. 2017;4(1):46-56.
- World Health Organization. ICD-10 Version:2019. Accessed June 24, 2024. https://icd.who.int/browse10/2019/en
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. Osteoporosis: Causes & Symptoms. Accessed June 24, 2024.
- Mayo Clinic. Osteoporosis – Symptoms and causes. Accessed June 24, 2024. https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
- Aibar-Almazán A, et al. Current Status of the Diagnosis and Management of Osteoporosis. Int J Environ Res Public Health. 2022;19(16):10049.
- National Center for Biotechnology Information. Osteoporosis: Clinical Evaluation. Accessed June 24, 2024.
- Lewiecki EM, et al. Osteoporosis diagnosis and screening. UpToDate. Accessed June 24, 2024.
- Kanis JA, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019;30(1):3-44.
- Cosman F, et al. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25(10):2359-81.
- National Institutes of Health. Osteoporosis: Diagnosis, Treatment, and Steps to Take. Accessed June 24, 2024. https://www.niams.nih.gov/health-topics/osteoporosis/diagnosis-treatment-and-steps-to-take
Related articles
Made in USA