Introduction
Back syndrome without radiating pain, also known as non-specific back pain, is a common condition characterized by pain and discomfort in the back region[1]. It is a significant health issue that can affect individuals of all ages and can have a significant impact on their quality of life[2]. The aim of this guide is to provide healthcare professionals with a comprehensive clinical procedural guide for the diagnosis and management of back syndrome without radiating pain.
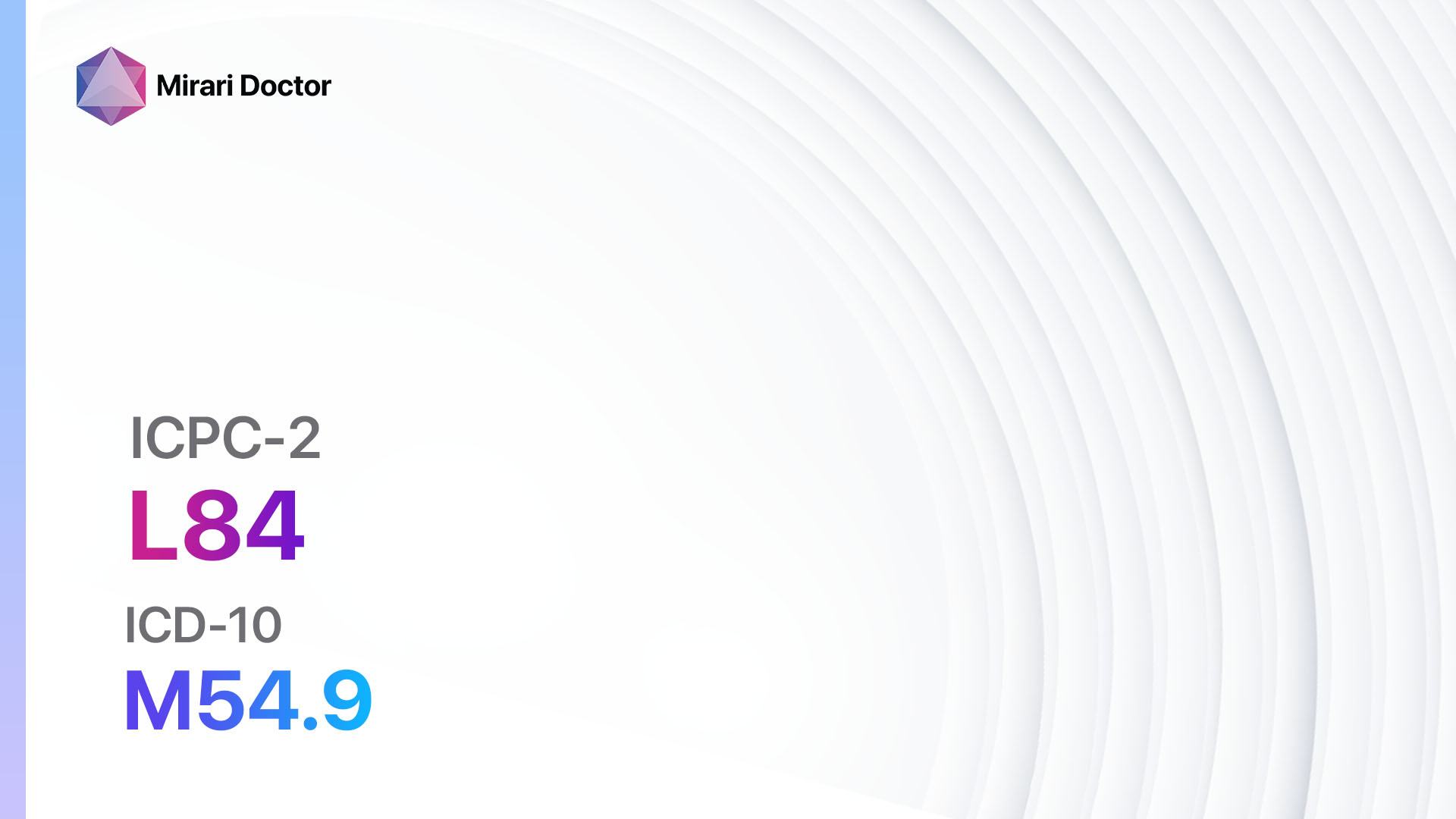
Codes
Symptoms
- Dull, aching pain in the back region[5]
- Stiffness and limited range of motion in the back[6]
- Muscle spasms in the back[7]
- Tenderness and sensitivity in the back muscles[8]
- Difficulty in maintaining proper posture[9]
- Pain worsens with movement or prolonged sitting or standing[10]
Causes
- Muscle strain or sprain due to overuse or improper lifting techniques
- Poor posture and body mechanics
- Sedentary lifestyle and lack of exercise
- Obesity and excess weight
- Stress and psychological factors
Diagnostic Steps
Medical History
- Gather information about the patient’s age, occupation, and lifestyle factors that may contribute to back pain.
- Ask about the onset, duration, and severity of the pain.
- Inquire about any previous injuries or medical conditions that may be related to the back pain.
- Assess the impact of the pain on the patient’s daily activities and quality of life.
Physical Examination
- Observe the patient’s posture and body mechanics during movement.
- Palpate the back muscles for tenderness and trigger points.
- Assess the range of motion of the spine and any limitations.
- Perform neurological examination to rule out any radiating pain or neurological deficits.
Laboratory Tests
- Routine blood tests to rule out any underlying medical conditions, such as infection or inflammation.
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) to assess for inflammation.
- Rheumatoid factor and antinuclear antibody (ANA) tests to rule out autoimmune conditions.
Diagnostic Imaging
- X-rays of the spine to assess for any structural abnormalities, such as fractures or degenerative changes.
- Magnetic resonance imaging (MRI) to visualize soft tissues, such as discs, ligaments, and nerves.
- Computed tomography (CT) scan to assess for bone abnormalities or spinal stenosis.
Other Tests
- Electromyography (EMG) and nerve conduction studies (NCS) to evaluate nerve function and rule out any nerve compression or damage.
- Bone scan or positron emission tomography (PET) scan to assess for bone metastasis or tumors.
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the patient’s progress and adjust the treatment plan if necessary.
- Provide patient education on proper body mechanics, posture, and exercises to strengthen the back muscles.
- Encourage the patient to maintain a healthy lifestyle, including regular exercise, weight management, and stress reduction techniques.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Back syndrome without radiating pain:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., Ibuprofen, Naproxen):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: History of gastrointestinal bleeding, renal impairment.
- Side effects: Upset stomach, heartburn, dizziness.
- Severe side effects: Gastrointestinal bleeding, kidney damage.
- Drug interactions: Anticoagulants, corticosteroids.
- Warning: Prolonged use may increase the risk of cardiovascular events.
- Muscle relaxants (e.g., Cyclobenzaprine, Methocarbamol):
- Cost: Generic versions can be $4-$30/month.
- Contraindications: Glaucoma, urinary retention.
- Side effects: Drowsiness, dizziness, dry mouth.
- Severe side effects: Allergic reactions, liver toxicity.
- Drug interactions: Sedatives, alcohol.
- Warning: Avoid driving or operating heavy machinery while taking muscle relaxants.
- Acetaminophen:
- Cost: Generic versions can be $3-$10/month.
- Contraindications: Liver disease, alcoholism.
- Side effects: Rare at therapeutic doses.
- Severe side effects: Liver toxicity (with overdose).
- Drug interactions: Warfarin, alcohol.
- Warning: Avoid exceeding the recommended dosage to prevent liver damage.
- Topical analgesics (e.g., Capsaicin cream, Lidocaine patches):
- Cost: Varies depending on the specific product.
- Contraindications: Allergy to the active ingredient.
- Side effects: Local skin irritation, burning sensation.
- Severe side effects: Allergic reactions.
- Drug interactions: None significant.
- Warning: Wash hands thoroughly after applying topical analgesics.
- Antidepressants (e.g., Amitriptyline, Duloxetine):
- Cost: Generic versions can be $4-$30/month.
- Contraindications: Recent myocardial infarction, narrow-angle glaucoma.
- Side effects: Sedation, dry mouth, constipation.
- Severe side effects: Suicidal thoughts, serotonin syndrome.
- Drug interactions: Monoamine oxidase inhibitors (MAOIs), other serotonergic drugs.
- Warning: Monitor for signs of worsening depression or suicidal ideation.
Alternative Drugs:
- Gabapentin: An anticonvulsant that can help with neuropathic pain. Cost: $10-$50/month.
- Tramadol: A weak opioid analgesic that can be used for moderate to severe pain. Cost: $10-$50/month.
- Steroid injections: Intra-articular or epidural injections of corticosteroids for short-term pain relief. Cost: $100-$500 per injection.
- Capsaicin patches: Topical patches containing capsaicin for localized pain relief. Cost: $10-$50 per patch.
- Benzodiazepines: Can be used for short-term relief of muscle spasms. Cost: $4-$30/month.
Surgical Procedures:
- Surgery is generally not recommended for non-specific back pain without radiating pain. However, in cases where conservative treatments have failed and there is evidence of structural abnormalities, surgical interventions may be considered. Common surgical procedures include:
- Discectomy: Removal of a herniated disc that is causing nerve compression.
- Spinal fusion: Joining two or more vertebrae together to stabilize the spine.
- Artificial disc replacement: Replacement of a damaged disc with an artificial disc.
Alternative Interventions
- Chiropractic care: Manual manipulation of the spine to improve alignment and reduce pain. Cost: $30-$200 per session.
- Physical therapy: Targeted exercises and therapies to improve strength, flexibility, and posture. Cost: $50-$200 per session.
- Massage therapy: Manipulation of soft tissues to reduce muscle tension and improve circulation. Cost: $50-$150 per session.
- Acupuncture: Insertion of thin needles into specific points on the body to stimulate healing and pain relief. Cost: $60-$120 per session.
- Yoga and Pilates: Mind-body exercises that focus on strength, flexibility, and posture. Cost: Varies depending on the location and instructor.
Lifestyle Interventions
- Exercise: Regular physical activity, including aerobic exercises, strength training, and stretching, can help improve back pain. Cost: Varies depending on the location and type of exercise.
- Weight management: Maintaining a healthy weight can reduce the strain on the back muscles and joints. Cost: Varies depending on the chosen weight loss method.
- Posture correction: Practicing proper body mechanics and maintaining good posture can alleviate back pain. Cost: None.
- Ergonomic modifications: Making adjustments to workstations and seating arrangements to promote proper posture and reduce strain on the back. Cost: Varies depending on the modifications needed.
- Stress reduction techniques: Engaging in activities such as meditation, deep breathing exercises, and mindfulness can help reduce stress and tension in the back muscles. Cost: None.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – L84 Back syndrome w/o radiating pain (ICD-10:M54.9)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 9 (Arthritis) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 9 (Arthritis) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 9 (Arthritis) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning:30minutesapprox.$5USD, Evening:30minutesapprox.$5USD | Total Morning:60minutesapprox.$10USD, Lunch:60minutesapprox. $10 USD, Evening:60minutesapprox. $10 USD, | Total Morning:60minutesapprox.$10USD, Lunch:60minutesapprox. $10 USD, Evening:60minutesapprox. $10 USD, |
| Usualtreatmentfor7-60daysapprox.$70USD–$600USD | Usualtreatmentfor6-8weeksapprox.$1,260USD–$1,680USD | Usualtreatmentfor3-6monthsapprox.$2,700USD–$5,400USD |
 |
|
Use the Mirari Cold Plasma device to treat Back syndrome w/o radiating pain effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Back syndrome w/o radiating pain. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356-2367. doi:10.1016/S0140-6736(18)30480-X
- Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968-974. doi:10.1136/annrheumdis-2013-204428
- ICPC-2 – English. Accessed June 22, 2024.//www.who.int/standards/classifications/other-classifications/international-classification-of-primary-care
- ICD-10 Version:2019. Accessed June 22, 2024.//icd.who.int/browse10/2019/en#/M54.9
- Chou R. Low back pain (chronic). BMJ Clin Evid. 2010;2010:1116.
- Allegri M, Montella S, Salici F, et al. Mechanisms of low back pain: a guide for diagnosis and therapy. F1000Res. 2016;5:F1000 Faculty Rev-1530. Published 2016 Jun 28. doi:10.12688/f1000research.8105.2
- Casazza BA. Diagnosis and treatment of acute low back pain. Am Fam Physician. 2012;85(4):343-350.
- Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736-747. doi:10.1016/S0140-6736(16)30970-9
- Steffens D, Maher CG, Pereira LS, et al. Prevention of Low Back Pain: A Systematic Review and Meta-analysis. JAMA Intern Med. 2016;176(2):199-208. doi:10.1001/jamainternmed.2015.7431
- Will JS, Bury DC, Miller JA. Mechanical Low Back Pain. Am Fam Physician. 2018;98(7):421-428.
Related articles
Made in USA