Introduction
Eye/adnexa disease refers to a group of conditions that affect the eye and its surrounding structures. These conditions can range from minor irritations to serious infections or disorders.[1] This guide aims to provide an overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for eye/adnexa disease.
Codes
- ICPC-2 Code: F99 Eye/adnexa disease, other[2]
- ICD-10 Code: H57.9 Unspecified disorder of eye and adnexa[3]
Symptoms
- Eye redness: The eye appears red or bloodshot.[4]
- Eye pain: The eye may feel sore or painful.[4]
- Eye discharge: There may be discharge from the eye.[4]
- Blurred vision: Vision may be blurry or unclear.[4]
- Sensitivity to light: The eye may be sensitive to bright lights.[4]
- Itching or burning sensation: The eye may feel itchy or burning.[4]
- Swelling: The eye or the surrounding area may be swollen.[4]
Causes
- Allergies: Allergic reactions to substances such as pollen, dust, or pet dander can cause eye/adnexa disease.[5]
- Infections: Bacterial, viral, or fungal infections can lead to eye/adnexa disease.[5]
- Dry eyes: Insufficient tear production or poor tear quality can result in eye/adnexa disease.[5]
- Eye strain: Prolonged use of digital devices or reading in poor lighting conditions can strain the eyes.[5]
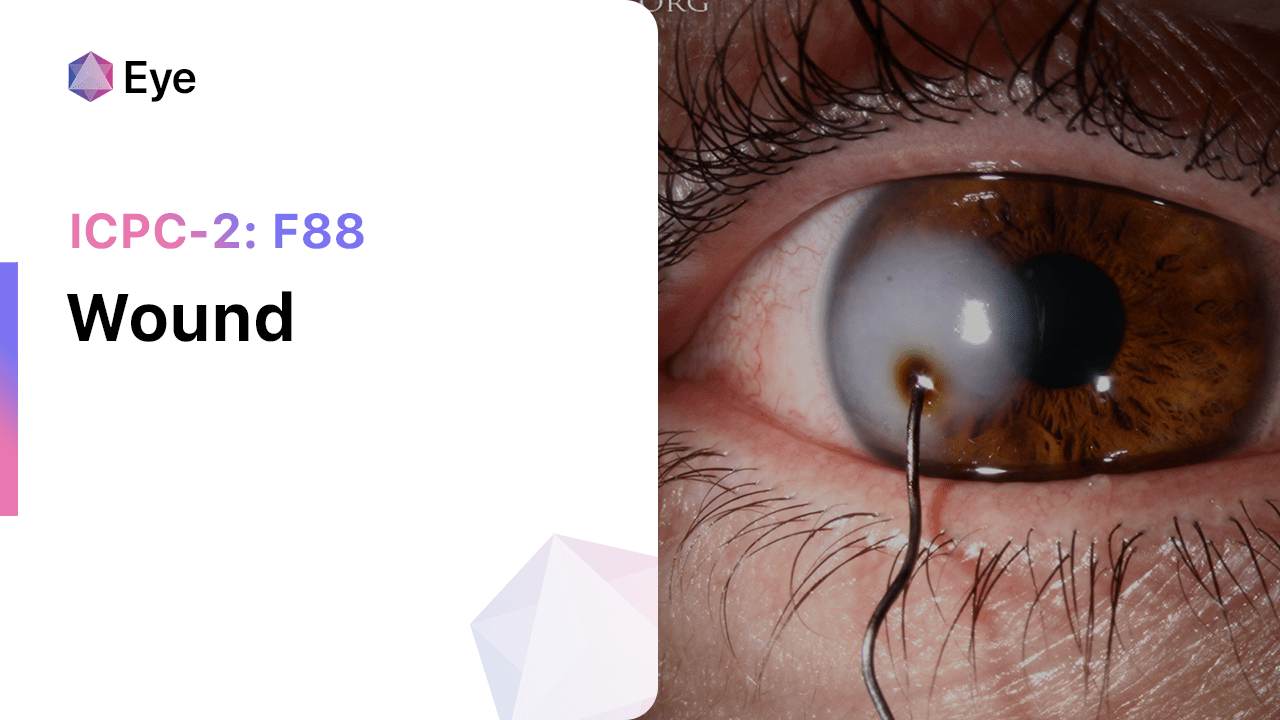
- Trauma: Injury or trauma to the eye or its surrounding structures can cause eye/adnexa disease.[5]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration and severity.[6]
- Inquire about any previous eye conditions or surgeries.[6]
- Ask about any allergies or exposure to irritants.[6]
- Determine if the patient has any underlying medical conditions that may contribute to eye/adnexa disease.[6]
Physical Examination
- Inspect the eye and its surrounding structures for redness, swelling, discharge, or other abnormalities.[7]
- Assess visual acuity by performing a visual acuity test.[7]
- Evaluate eye movements and coordination.[7]
- Examine the eyelids, lashes, and conjunctiva for signs of infection or inflammation.[7]
Laboratory Tests
- Conjunctival swab: A swab is taken from the conjunctiva to identify the presence of bacteria, viruses, or fungi.[8]
- Tear film analysis: Tear samples are collected to assess tear production and quality.[8]
- Allergy testing: Skin prick tests or blood tests may be performed to identify specific allergens.[8]
Diagnostic Imaging
- Slit-lamp examination: A specialized microscope is used to examine the structures of the eye in detail.[9]
- Optical coherence tomography (OCT): This imaging technique provides cross-sectional images of the eye, allowing for the evaluation of the retina and other structures.[9]
- Ultrasound: Ultrasound imaging may be used to assess the structures of the eye in cases where visualization is difficult.[9]
Other Tests
- Schirmer’s test: Measures tear production by placing a small strip of filter paper in the lower eyelid.[10]
- Fluorescein staining: A dye is used to assess the integrity of the cornea and detect any abnormalities.[10]
- Intraocular pressure measurement: This test is performed to screen for glaucoma.[10]
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the progress of the condition and adjust treatment if necessary.
- Provide education on proper eye hygiene, including handwashing, avoiding touching the eyes, and proper contact lens care.
- Discuss the importance of regular eye examinations and the potential need for long-term management of the condition.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Eye/adnexa disease, other:
- Artificial tears:
- Cost: $5-$20 per bottle.
- Contraindications: None.
- Side effects: None.
- Severe side effects: None.
- Drug interactions: None.
- Warning: None.
- Antibiotic eye drops (e.g., Tobramycin, Ciprofloxacin):
- Cost: $10-$50 per bottle.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Temporary stinging or burning sensation.
- Severe side effects: Allergic reactions.
- Drug interactions: None.
- Warning: Use as directed and complete the full course of treatment.
- Antihistamine eye drops (e.g., Ketotifen, Olopatadine):
- Cost: $10-$30 per bottle.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Temporary stinging or burning sensation.
- Severe side effects: Allergic reactions.
- Drug interactions: None.
- Warning: Use as directed and avoid contact lens use during treatment.
- Steroid eye drops (e.g., Prednisolone, Dexamethasone):
- Cost: $10-$50 per bottle.
- Contraindications: Active eye infections, glaucoma.
- Side effects: Temporary stinging or burning sensation, increased intraocular pressure with prolonged use.
- Severe side effects: Increased risk of eye infections, cataract formation, glaucoma.
- Drug interactions: None.
- Warning: Use as directed and do not use for extended periods without medical supervision.
- Nonsteroidal anti-inflammatory eye drops (e.g., Ketorolac, Bromfenac):
- Cost: $20-$60 per bottle.
- Contraindications: Hypersensitivity to the medication, active eye infections.
- Side effects: Temporary stinging or burning sensation.
- Severe side effects: Allergic reactions.
- Drug interactions: None.
- Warning: Use as directed and avoid contact lens use during treatment.
Alternative Drugs:
- Mast cell stabilizers (e.g., Cromolyn sodium): Help prevent the release of histamine and other inflammatory substances.
- Corticosteroid ointments (e.g., Hydrocortisone): Used for certain eye conditions that require longer-lasting treatment.
- Antiviral eye drops (e.g., Ganciclovir): Used for viral eye infections.
- Immunosuppressive eye drops (e.g., Cyclosporine): Used for certain autoimmune eye conditions.
- Lubricating ointments: Provide longer-lasting relief for dry eyes.
Surgical Procedures:
- Laser eye surgery: Corrects refractive errors such as nearsightedness, farsightedness, and astigmatism. Cost: $1,500-$3,000 per eye.
- Cataract surgery: Removes the cloudy lens and replaces it with an artificial lens. Cost: $3,000-$5,000 per eye.
- Eyelid surgery: Corrects droopy eyelids or removes excess skin and fat. Cost: $2,000-$5,000.
Alternative Interventions
- Warm compresses: Applying warm compresses to the eyes can help relieve symptoms of eye/adnexa disease. Cost: Free.
- Cold compresses: Cold compresses can reduce inflammation and swelling in the eyes. Cost: Free.
- Eye exercises: Certain eye exercises can help improve eye muscle coordination and reduce eye strain. Cost: Free.
- Herbal eye drops: Some herbal eye drops, such as chamomile or calendula, may provide relief for certain eye conditions. Cost: $5-$20 per bottle.
- Acupuncture: Acupuncture may help improve blood flow and reduce eye inflammation. Cost: $60-$120 per session.
Lifestyle Interventions
- Proper eye hygiene: Practicing good eye hygiene, such as washing hands before touching the eyes and avoiding rubbing the eyes, can help prevent eye infections. Cost: Free.
- Wearing protective eyewear: Using protective eyewear, such as goggles or sunglasses, can shield the eyes from irritants and UV rays. Cost: $10-$50.
- Taking regular breaks: Taking regular breaks from digital devices or activities that strain the eyes can help reduce eye fatigue. Cost: Free.
- Maintaining a healthy diet: Consuming a diet rich in vitamins and minerals, particularly those beneficial for eye health (e.g., vitamin A, C, E, omega-3 fatty acids), can support overall eye health. Cost: Varies depending on food choices.
- Getting enough sleep: Sufficient sleep is essential for eye health and overall well-being. Cost: Free.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – F99 Eye/adnexa disease, other (ICD-10:H57.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Eye/adnexa disease, other effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Eye/adnexa disease, other. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Heathcote, J. G. (2022). The ocular adnexa. Indian Journal of Ophthalmology, 70(2), 324-325.
- PH3C. (n.d.). International Classification of Primary Care. Retrieved from http://www.ph3c.org/PH3C/docs/27/000496/0000908.pdf
- ICD10data.com. (2024). 2024 ICD-10-CM Diagnosis Code H57.9. Retrieved from https://www.icd10data.com/ICD10CM/Codes/H00-H59/H55-H57/H57-/H57.9
- Demeritt, M. J., & Lewandowska, B. I. (2020). Differentiating Problems of the Eyelids and Ocular Adnexa. Review of Optometry, 157(2), 46-52.
- Pasadhika, S., & Rosenbaum, J. T. (2015). Ocular Sarcoidosis. Clinics in Chest Medicine, 36(4), 669-683.
- Stagner, A. M., & Jakobiec, F. A. (2022). Diagnostic Approach to Orbital Disorders: Perspective of the Ophthalmic Pathologist. Indian Journal of Ophthalmology, 70(2), 326-334.
- Alkatan, H. M., Maktabi, A., & Alwadani, S. (2022). Biopsy Techniques for Orbital Tumors: A Review. Indian Journal of Ophthalmology, 70(2), 335-340.
- Walsh, N. M. (2022). Merkel Cell Carcinoma of the Eyelid. Indian Journal of Ophthalmology, 70(2), 341-346.
- Heathcote, J. G. (2022). Oncocytic Lesions of the Ocular Adnexa. Indian Journal of Ophthalmology, 70(2), 347-353.
- Demeritt, M. J., & Lewandowska, B. I. (2020). Differentiating Problems of the Eyelids and Ocular Adnexa. Review of Optometry, 157(2), 46-52.
Related articles
Made in USA