Introduction
Glaucoma is a group of eye conditions that damage the optic nerve, leading to vision loss and blindness if left untreated[1]. It is a significant condition as it affects millions of people worldwide and is a leading cause of irreversible blindness[2]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of glaucoma, including its symptoms, causes, diagnostic steps, possible interventions, and patient education.
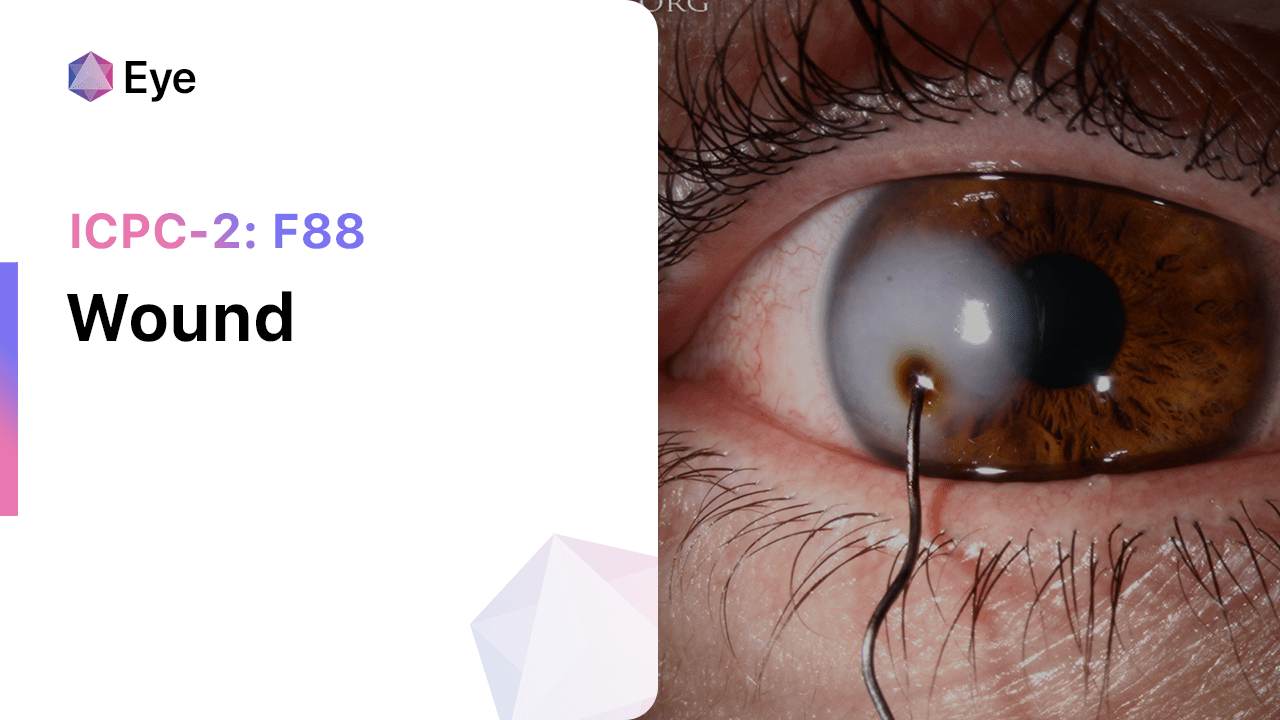
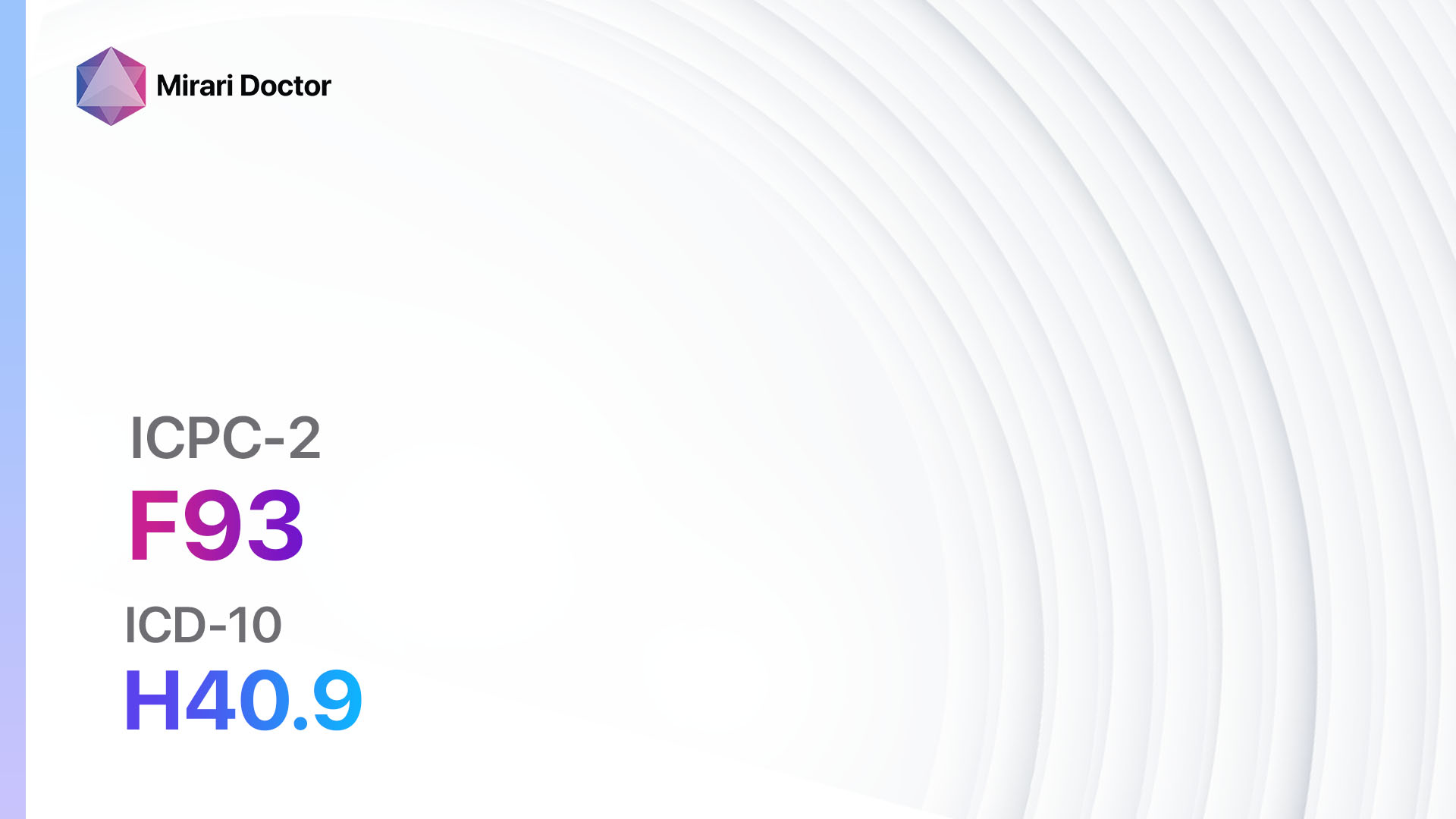
Codes
Symptoms
- Gradual loss of peripheral vision[5]
- Tunnel vision[5]
- Blurred vision[6]
- Halos around lights[6]
- Eye pain[7]
- Redness in the eye[7]
- Nausea or vomiting (in acute angle-closure glaucoma)[7]
Causes
- Increased intraocular pressure (IOP)[8]
- Impaired blood flow to the optic nerve[9]
- Genetic factors[10]
- Age-related changes in the eye
- Eye injuries or trauma
- Certain medical conditions, such as diabetes and high blood pressure
Diagnostic Steps
Medical History
- Gather information about the patient’s risk factors, such as family history of glaucoma, age, and medical conditions.
- Ask about symptoms related to glaucoma, such as vision changes, eye pain, and redness.
- Inquire about any previous eye injuries or surgeries.
- Assess the patient’s current medications, as some may increase the risk of glaucoma.
Physical Examination
- Measure intraocular pressure (IOP) using a tonometer.
- Examine the optic nerve for signs of damage, such as cupping or thinning.
- Evaluate visual acuity and visual field.
- Assess the anterior chamber angle using gonioscopy.
Laboratory Tests
- None required for the diagnosis of glaucoma.
Diagnostic Imaging
- Optical coherence tomography (OCT) to assess the thickness of the retinal nerve fiber layer.
- Visual field testing to detect peripheral vision loss.
- Fundus photography to document optic nerve appearance and changes over time.
Other Tests
- Corneal pachymetry to measure corneal thickness, which can affect IOP measurements.
- Genetic testing for certain types of glaucoma, such as primary open-angle glaucoma.
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor disease progression and treatment effectiveness.
- Educate patients about the importance of adherence to medication and regular eye examinations.
- Provide information on lifestyle modifications, such as avoiding smoking and maintaining a healthy diet.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Glaucoma:
- Prostaglandin analogs (e.g., Latanoprost, Bimatoprost):
- Cost: $50-$150/month.
- Contraindications: Hypersensitivity to the drug.
- Side effects: Eye redness, darkening of the iris or eyelid skin.
- Severe side effects: Macular edema, uveitis.
- Drug interactions: None significant.
- Warning: May cause changes in eye color and eyelash growth.
- Beta-blockers (e.g., Timolol, Betaxolol):
- Cost: $10-$50/month.
- Contraindications: Asthma, severe chronic obstructive pulmonary disease (COPD).
- Side effects: Eye irritation, decreased heart rate.
- Severe side effects: Bronchospasm, heart block.
- Drug interactions: Calcium channel blockers, insulin.
- Warning: May worsen respiratory conditions.
- Alpha-adrenergic agonists (e.g., Brimonidine, Apraclonidine):
- Cost: $20-$80/month.
- Contraindications: Hypersensitivity to the drug.
- Side effects: Eye redness, dry mouth.
- Severe side effects: Allergic reactions, hypotension.
- Drug interactions: Monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants.
- Warning: May cause drowsiness and fatigue.
- Carbonic anhydrase inhibitors (e.g., Dorzolamide, Brinzolamide):
- Cost: $30-$100/month.
- Contraindications: Sulfa allergy.
- Side effects: Eye burning or stinging, bitter taste.
- Severe side effects: Stevens-Johnson syndrome, blood disorders.
- Drug interactions: Aspirin, other carbonic anhydrase inhibitors.
- Warning: May cause electrolyte imbalances.
- Miotic agents (e.g., Pilocarpine):
- Cost: $10-$30/month.
- Contraindications: Inflammatory conditions of the eye.
- Side effects: Eye irritation, blurred vision.
- Severe side effects: Retinal detachment, cataracts.
- Drug interactions: None significant.
- Warning: May cause difficulty seeing in dim light.
Alternative Drugs:
- Rho kinase inhibitors (e.g., Netarsudil): A newer class of glaucoma medications that can be used as an alternative or adjunct to traditional treatments.
- Combination medications: Some medications combine two or more classes of glaucoma drugs to improve convenience and adherence.
Surgical Procedures:
- Trabeculectomy: A surgical procedure to create a new drainage channel for the aqueous humor, reducing intraocular pressure. Cost: $3,000-$6,000.
- Glaucoma drainage devices: Implantable devices that help drain excess fluid from the eye. Cost: $5,000-$10,000.
- Laser trabeculoplasty: A laser is used to improve the drainage of fluid from the eye. Cost: $1,000-$2,000.
- Cyclophotocoagulation: Laser treatment to reduce the production of fluid in the eye. Cost: $1,500-$3,000.
Alternative Interventions
- Acupuncture: May help reduce intraocular pressure and improve blood flow to the optic nerve. Cost: $60-$120 per session.
- Herbal supplements: Some herbs, such as bilberry and ginkgo biloba, may have potential benefits for glaucoma. Cost: Varies depending on the specific supplement.
- Nutritional supplements: Antioxidants like vitamin C and vitamin E may help protect the optic nerve. Cost: Varies depending on the specific supplement.
- Yoga and meditation: Can help reduce stress and improve overall well-being, potentially benefiting glaucoma patients. Cost: Varies depending on the class or program.
- Lifestyle modifications: Maintaining a healthy diet, regular exercise, and avoiding smoking may help reduce the risk of glaucoma progression. Cost: Varies depending on individual choices.
Lifestyle Interventions
- Regular exercise: Engaging in aerobic exercise, such as walking or swimming, can help improve blood flow and reduce intraocular pressure. Cost: Varies depending on individual choices.
- Healthy diet: Consuming a diet rich in fruits, vegetables, and omega-3 fatty acids may have protective effects on the optic nerve. Cost: Varies depending on individual choices.
- Stress management: Practicing stress-reducing techniques, such as deep breathing exercises or mindfulness meditation, can help lower intraocular pressure. Cost: Varies depending on individual choices.
- Smoking cessation: Quitting smoking can improve overall eye health and reduce the risk of glaucoma progression. Cost: Varies depending on individual choices.
- Proper eye protection: Wearing protective eyewear during activities that may cause eye injuries can help prevent glaucoma-related damage. Cost: Varies depending on individual choices.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – F93 Glaucoma (ICD-10:H40.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Glaucoma effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Glaucoma. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Weinreb, R. N., Aung, T., & Medeiros, F. A. (2014). The pathophysiology and treatment of glaucoma: a review. JAMA, 311(18), 1901-1911.
- Tham, Y. C., Li, X., Wong, T. Y., Quigley, H. A., Aung, T., & Cheng, C. Y. (2014). Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology, 121(11), 2081-2090.
- World Organization of Family Doctors (WONCA). (1998). ICPC-2: International Classification of Primary Care. Oxford University Press, USA.
- World Health Organization. (2019). International statistical classification of diseases and related health problems (11th ed.).
- Crabb, D. P., Smith, N. D., Glen, F. C., Burton, R., & Garway-Heath, D. F. (2013). How does glaucoma look?: patient perception of visual field loss. Ophthalmology, 120(6), 1120-1126.
- Shields, M. B. (2008). Normal-tension glaucoma: is it different from primary open-angle glaucoma?. Current opinion in ophthalmology, 19(2), 85-88.
- Weinreb, R. N., & Khaw, P. T. (2004). Primary open-angle glaucoma. The Lancet, 363(9422), 1711-1720.
- Kwon, Y. H., Fingert, J. H., Kuehn, M. H., & Alward, W. L. (2009). Primary open-angle glaucoma. New England Journal of Medicine, 360(11), 1113-1124.
- Flammer, J., Orgül, S., Costa, V. P., Orzalesi, N., Krieglstein, G. K., Serra, L. M., … & Stefánsson, E. (2002). The impact of ocular blood flow in glaucoma. Progress in retinal and eye research, 21(4), 359-393.
- Wiggs, J. L. (2015). Glaucoma genes and mechanisms. Progress in molecular biology and translational science, 134, 315-342.
Related articles
Made in USA