Introduction
Macular degeneration is a chronic eye condition that affects the macula, the part of the retina responsible for central vision. It is a leading cause of vision loss in older adults[1]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of macular degeneration.
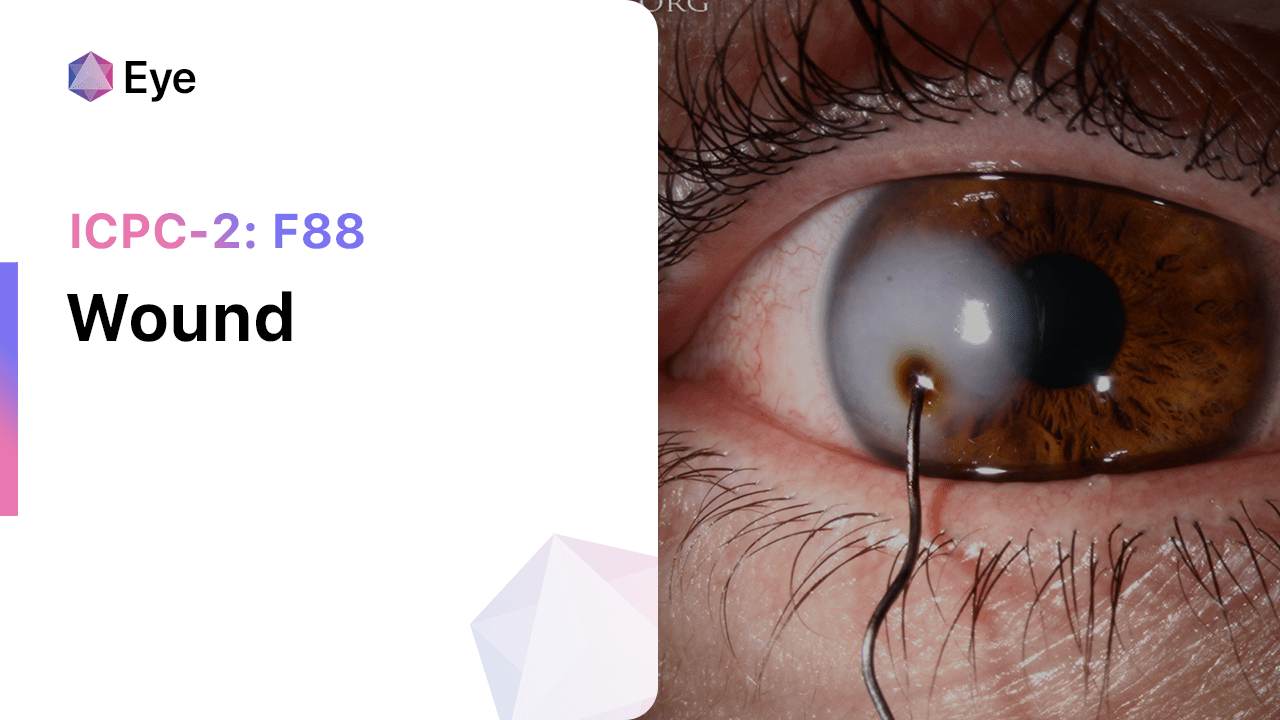
Codes
Symptoms
- Blurred or distorted central vision[2]
- Difficulty reading or recognizing faces[3]
- Dark or empty areas in the central vision[4]
- Decreased color perception[5]
- Straight lines appearing wavy or distorted[6]
Causes
- Age-related macular degeneration (AMD): The most common form of macular degeneration, which occurs due to aging and degeneration of the macula[7].
- Genetic factors: Certain genetic variations have been associated with an increased risk of developing macular degeneration[8].
- Smoking: Smoking has been identified as a significant risk factor for macular degeneration[9].
- Family history: Having a family history of macular degeneration increases the risk of developing the condition[10].
Diagnostic Steps
Medical History
- Gather information about the patient’s age, family history of macular degeneration, and smoking history.
- Ask about any symptoms related to macular degeneration, such as blurred or distorted vision.
- Inquire about any other medical conditions or medications that may contribute to the development or progression of macular degeneration.
Physical Examination
- Perform a comprehensive eye examination, including visual acuity testing, dilated fundus examination, and evaluation of the macula.
- Look for signs of macular degeneration, such as drusen (yellow deposits under the retina) or pigmentary changes in the macula.
- Assess the patient’s overall eye health and rule out other potential causes of vision loss.
Laboratory Tests
- There are no specific laboratory tests for diagnosing macular degeneration.
- However, blood tests may be ordered to rule out other medical conditions that can mimic macular degeneration, such as autoimmune diseases or vitamin deficiencies.
Diagnostic Imaging
- Optical coherence tomography (OCT): This non-invasive imaging test provides detailed cross-sectional images of the retina, allowing for the detection and monitoring of macular degeneration.
- Fluorescein angiography: This test involves injecting a dye into the patient’s arm and taking photographs of the retina as the dye circulates. It helps identify abnormal blood vessels or leakage in the macula.
Other Tests
- Electroretinography (ERG): This test measures the electrical activity of the retina and can help differentiate between different types of macular degeneration.
- Genetic testing: In certain cases, genetic testing may be recommended to identify specific genetic variations associated with macular degeneration.
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the progression of macular degeneration and adjust treatment as needed.
- Educate the patient about the importance of lifestyle modifications, such as quitting smoking and maintaining a healthy diet, in slowing the progression of macular degeneration.
- Provide information about low vision aids and resources for patients with advanced macular degeneration.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Macular degeneration:
- Anti-VEGF agents (e.g., Ranibizumab, Bevacizumab, Aflibercept):
- Cost: $1,800-$2,000 per injection.
- Contraindications: Hypersensitivity to the drug.
- Side effects: Eye pain, increased intraocular pressure.
- Severe side effects: Endophthalmitis, retinal detachment.
- Drug interactions: None reported.
- Warning: Regular monitoring of intraocular pressure and signs of infection required.
- Corticosteroids (e.g., Triamcinolone acetonide):
- Cost: $500-$1,000 per injection.
- Contraindications: Active ocular infection, glaucoma.
- Side effects: Increased intraocular pressure, cataract formation.
- Severe side effects: Endophthalmitis, retinal detachment.
- Drug interactions: None reported.
- Warning: Regular monitoring of intraocular pressure and signs of infection required.
- Photodynamic therapy (PDT) with Verteporfin:
- Cost: $2,000-$3,000 per treatment.
- Contraindications: Porphyria, hypersensitivity to porphyrins.
- Side effects: Transient visual disturbances, skin photosensitivity.
- Severe side effects: Severe skin reactions, anaphylaxis.
- Drug interactions: None reported.
- Warning: Patients should avoid direct sunlight for 48 hours after treatment.
- Laser photocoagulation:
- Cost: $1,000-$2,000 per treatment.
- Contraindications: Foveal involvement, subfoveal hemorrhage.
- Side effects: Transient visual disturbances, scarring.
- Severe side effects: Vision loss, retinal detachment.
- Drug interactions: None reported.
- Warning: Regular monitoring of visual acuity and signs of complications required.
- Vitamin and mineral supplements (e.g., AREDS2 formulation):
- Cost: $20-$30 per month.
- Contraindications: None reported.
- Side effects: Gastrointestinal upset.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Patients should consult with their healthcare provider before starting any new supplements.
Alternative Drugs:
- Omega-3 fatty acids: Some studies suggest that omega-3 fatty acids may have a protective effect on the macula. Cost: $10-$20 per month.
- Lutein and zeaxanthin: These antioxidants are found in high concentrations in the macula and may help protect against macular degeneration. Cost: $10-$20 per month.
- B vitamins: Some evidence suggests that B vitamins, particularly vitamin B12 and folic acid, may reduce the risk of macular degeneration. Cost: $5-$10 per month.
- Ginkgo biloba: This herbal supplement has been studied for its potential benefits in improving vision and blood flow to the retina. Cost: $10-$20 per month.
- Coenzyme Q10: This antioxidant may have protective effects on the macula. Cost: $10-$20 per month.
Surgical Procedures:
- Photodynamic therapy (PDT) with Verteporfin: This procedure involves injecting a light-activated drug into the patient’s arm and then using a laser to activate the drug in the macula. Cost: $2,000-$3,000 per treatment.
- Retinal laser photocoagulation: This procedure uses a laser to seal leaking blood vessels in the macula. Cost: $1,000-$2,000 per treatment.
Alternative Interventions
- Acupuncture: May help improve blood flow and reduce pain. Cost: $60-$120 per session.
- Chelation therapy: Controversial treatment involving the administration of chelating agents to remove heavy metals from the body. Cost: $75-$150 per session.
- Hyperbaric oxygen therapy: Involves breathing pure oxygen in a pressurized chamber to increase oxygen delivery to tissues. Cost: $200-$300 per session.
- Herbal supplements: Some herbs, such as garlic and ginkgo biloba, may have potential benefits for improving circulation. Cost: Varies depending on the specific supplement.
Lifestyle Interventions
- Smoking cessation: Quitting smoking can help slow the progression of macular degeneration. Cost: Varies depending on the method used (e.g., nicotine replacement therapy, medications, counseling).
- Healthy diet: Consuming a diet rich in fruits, vegetables, and omega-3 fatty acids may help protect against macular degeneration. Cost: Varies depending on food choices.
- Regular exercise: Engaging in regular physical activity can improve overall health and may have a positive impact on macular degeneration. Cost: Varies depending on the chosen activity.
- UV protection: Wearing sunglasses and hats with brims can help protect the eyes from harmful UV rays. Cost: Varies depending on the chosen eyewear.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – F84 Macular degeneration (ICD-10:H35.3)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Macular degeneration effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Macular degeneration. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Lim, L. S., Mitchell, P., Seddon, J. M., Holz, F. G., & Wong, T. Y. (2012). Age-related macular degeneration. The Lancet, 379(9827), 1728-1738.
- Jager, R. D., Mieler, W. F., & Miller, J. W. (2008). Age-related macular degeneration. New England Journal of Medicine, 358(24), 2606-2617.
- Cheung, L. K., & Eaton, A. (2013). Age-related macular degeneration. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 33(8), 838-855.
- Ambati, J., & Fowler, B. J. (2012). Mechanisms of age-related macular degeneration. Neuron, 75(1), 26-39.
- Neelam, K., Nolan, J., Chakravarthy, U., & Beatty, S. (2009). Psychophysical function in age-related maculopathy. Survey of Ophthalmology, 54(2), 167-210.
- Hogg, R. E., & Chakravarthy, U. (2006). Visual function and dysfunction in early and late age-related maculopathy. Progress in Retinal and Eye Research, 25(3), 249-276.
- Chakravarthy, U., Wong, T. Y., Fletcher, A., Piault, E., Evans, C., Zlateva, G., … & Mitchell, P. (2010). Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmology, 10(1), 31.
- DeAngelis, M. M., Owen, L. A., Morrison, M. A., Morgan, D. J., Li, M., Shakoor, A., … & Kim, I. K. (2017). Genetics of age-related macular degeneration (AMD). Human Molecular Genetics, 26(R1), R45-R50.
- Myers, C. E., Klein, B. E., Gangnon, R., Sivakumaran, T. A., Iyengar, S. K., & Klein, R. (2014). Cigarette smoking and the natural history of age-related macular degeneration: the Beaver Dam Eye Study. Ophthalmology, 121(10), 1949-1955.
- Seddon, J. M., Cote, J., Page, W. F., Aggen, S. H., & Neale, M. C. (2005). The US twin study of age-related macular degeneration: relative roles of genetic and environmental influences. Archives of Ophthalmology, 123(3), 321-327.
Related articles
Made in USA