Introduction
Eye infection or inflammation, also known as conjunctivitis, is a common condition that affects the outermost layer of the eye and the inner surface of the eyelids. It can be caused by various factors such as bacteria, viruses, allergies, or irritants. The aim of this guide is to provide a comprehensive overview of the symptoms, causes, diagnostic steps, possible interventions, and patient education for eye infection/inflammation.
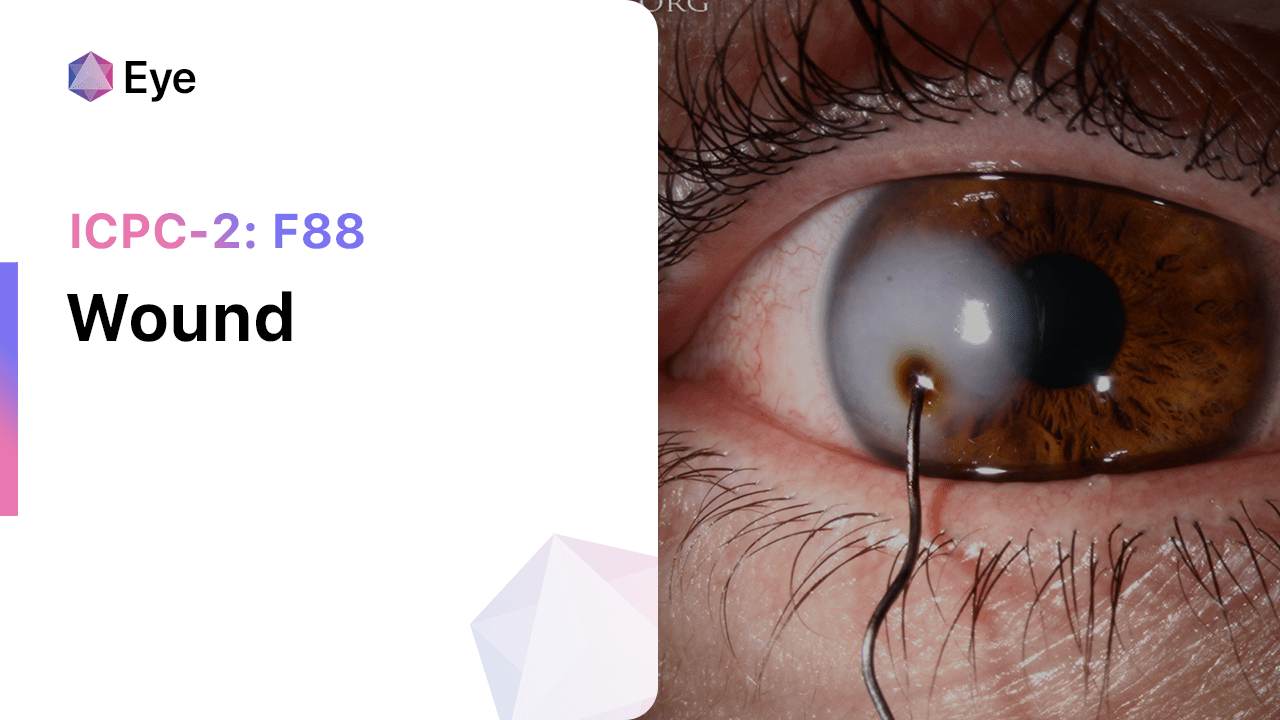
Codes
Symptoms
- Redness of the eye[3]
- Itching or burning sensation[4]
- Excessive tearing or discharge[5]
- Swelling of the eyelids[6]
- Sensitivity to light[7]
- Blurred vision[8]
Causes
- Bacterial infection: Caused by bacteria such as Staphylococcus aureus or Streptococcus pneumoniae.[9]
- Viral infection: Caused by viruses such as adenovirus or herpes simplex virus.[10]
- Allergic reaction: Triggered by allergens such as pollen, dust mites, or pet dander.
- Irritants: Exposure to irritants such as smoke, chemicals, or contact lenses.
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration and severity.
- Ask about any recent exposure to potential irritants or allergens.
- Inquire about any history of eye infections or allergies.
- Assess the patient’s overall health and any underlying medical conditions.
Physical Examination
- Inspect the eye for redness, swelling, or discharge.
- Evaluate the eyelids for signs of inflammation or crusting.
- Assess visual acuity and perform a basic eye examination.
- Check for any enlarged lymph nodes near the ear or neck.
Laboratory Tests
- Conjunctival swab: Collect a sample from the eye to identify the presence of bacteria or viruses.
- Allergy testing: Perform skin prick or blood tests to determine specific allergens causing the inflammation.
Diagnostic Imaging
- Not applicable for eye infection/inflammation.
Other Tests
- Schirmer’s test: Measures tear production to assess for dry eye syndrome.
- Fluorescein staining: Uses a dye to detect corneal abrasions or ulcers.
- Intraocular pressure measurement: Checks for elevated pressure, which may indicate glaucoma.
Follow-up and Patient Education
- Advise the patient to follow the prescribed treatment plan and complete the full course of medication.
- Instruct the patient to practice good hygiene, such as washing hands frequently and avoiding touching or rubbing the eyes.
- Educate the patient about the importance of avoiding irritants or allergens that may trigger the condition.
- Schedule a follow-up appointment to monitor the progress and ensure complete resolution of symptoms.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Eye infection/inflammation:
- Antibiotic eye drops (e.g., Tobramycin, Ciprofloxacin):
- Cost: $10-$30 per bottle.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Temporary stinging or burning sensation.
- Severe side effects: Allergic reactions, eye irritation.
- Drug interactions: None reported.
- Warning: Use as directed and complete the full course of treatment.
- Antiviral eye drops (e.g., Ganciclovir, Trifluridine):
- Cost: $20-$50 per bottle.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Temporary stinging or burning sensation.
- Severe side effects: Allergic reactions, eye irritation.
- Drug interactions: None reported.
- Warning: Use as directed and complete the full course of treatment.
- Antihistamine eye drops (e.g., Ketotifen, Olopatadine):
- Cost: $10-$30 per bottle.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Temporary stinging or burning sensation.
- Severe side effects: Allergic reactions, eye irritation.
- Drug interactions: None reported.
- Warning: Use as directed and avoid contact lens use during treatment.
- Steroid eye drops (e.g., Prednisolone, Dexamethasone):
- Cost: $10-$30 per bottle.
- Contraindications: Active viral or fungal eye infections.
- Side effects: Temporary stinging or burning sensation, increased intraocular pressure.
- Severe side effects: Eye infections, cataract formation.
- Drug interactions: None reported.
- Warning: Use as directed and do not abruptly stop treatment.
- Artificial tears (e.g., Refresh Tears, Systane):
- Cost: $5-$15 per bottle.
- Contraindications: Hypersensitivity to the medication.
- Side effects: None reported.
- Severe side effects: None reported.
- Drug interactions: None reported.
- Warning: Use as needed for lubrication and relief of dryness.
Alternative Drugs:
- Oral antihistamines (e.g., Loratadine, Cetirizine): May be used for allergic conjunctivitis. Cost: $5-$20 per month.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., Ketorolac, Nepafenac): Can help reduce inflammation. Cost: $10-$30 per bottle.
- Mast cell stabilizers (e.g., Cromolyn sodium, Lodoxamide): Prevent the release of histamine. Cost: $10-$30 per bottle.
- Topical decongestants (e.g., Phenylephrine, Naphazoline): Provide temporary relief of redness. Cost: $5-$15 per bottle.
- Systemic antibiotics (e.g., Azithromycin, Doxycycline): Used for severe or persistent bacterial conjunctivitis. Cost: $10-$50 per course.
Surgical Procedures:
- Not applicable for eye infection/inflammation.
Alternative Interventions
- Warm compress: Apply a warm compress to the affected eye to help relieve symptoms. Cost: Free.
- Cold compress: Apply a cold compress to reduce swelling and soothe the eye. Cost: Free.
- Saline rinses: Rinse the eyes with saline solution to flush out irritants. Cost: $5-$10 per bottle.
- Herbal eye drops: Some herbal eye drops, such as chamomile or calendula, may provide relief. Cost: $10-$20 per bottle.
- Probiotics: Taking probiotic supplements may help improve overall eye health. Cost: $10-$30 per month.
Lifestyle Interventions
- Avoidance of allergens: Identify and avoid allergens that trigger the condition, such as pollen or pet dander. Cost: Free.
- Good hygiene practices: Wash hands frequently, avoid touching or rubbing the eyes, and clean contact lenses properly. Cost: Free.
- Use of protective eyewear: Wear sunglasses or goggles to protect the eyes from irritants or allergens. Cost: $10-$50 per pair.
- Proper contact lens care: Follow proper cleaning and disinfection procedures for contact lenses. Cost: $10-$30 per bottle of contact lens solution.
- Adequate rest and hydration: Get enough sleep and drink plenty of water to support overall eye health. Cost: Free.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – F73 Eye infection/inflammation other (ICD-10:H10.8)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Eye infection/inflammation other effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Eye infection/inflammation other. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- World Health Organization. (2022). International Classification of Primary Care, Second edition (ICPC-2). Retrieved from https://www.who.int/standards/classifications/other-classifications/international-classification-of-primary-care
- World Health Organization. (2022). International Statistical Classification of Diseases and Related Health Problems (ICD-10). Retrieved from https://www.who.int/standards/classifications/classification-of-diseases
- Azari, A. A., & Barney, N. P. (2013). Conjunctivitis: a systematic review of diagnosis and treatment. JAMA, 310(16), 1721-1729. https://doi.org/10.1001/jama.2013.280318
- Høvding, G. (2008). Acute bacterial conjunctivitis. Acta Ophthalmologica, 86(1), 5-17. https://doi.org/10.1111/j.1600-0420.2007.01006.x
- Silverstein, B. E., & Morris, T. W. (2019). Conjunctivitis. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK537164/
- Rietveld, R. P., ter Riet, G., Bindels, P. J., Sloos, J. H., & van Weert, H. C. (2005). Predicting bacterial cause in infectious conjunctivitis: cohort study on informativeness of combinations of signs and symptoms. BMJ, 330(7497), 942. https://doi.org/10.1136/bmj.38420.658204.AE
- Cronau, H., Kankanala, R. R., & Mauger, T. (2010). Diagnosis and management of red eye in primary care. American family physician, 81(2), 137-144. https://www.aafp.org/pubs/afp/issues/2010/0115/p137.html
- Kaufman, H. E. (2011). Adenovirus advances: new diagnostic and therapeutic options. Current opinion in ophthalmology, 22(4), 290-293. https://doi.org/10.1097/ICU.0b013e328346d590
- Bielory, L., & Friedlaender, M. H. (2008). Allergic conjunctivitis. Immunology and Allergy Clinics of North America, 28(1), 43-58. https://doi.org/10.1016/j.iac.2007.12.005
- Liddle, Olivia Louise ; Samuel, Mannampallil Itty ; Sudhanva, Malur ; Ellis, Joanna ; Taylor, Chris (2015). Adenovirus urethritis and concurrent conjunctivitis: a case series and review of the literature. DOI: 10.1136/sextrans-2014-051868
Related articles
Made in USA