Introduction
Death is the permanent cessation of all biological functions that sustain a living organism[1]. It is a natural and inevitable part of life, but it can be a challenging and emotional experience for individuals and their loved ones[2]. The aim of this guide is to provide information on the symptoms, causes, diagnostic steps, possible interventions, and follow-up care related to death.
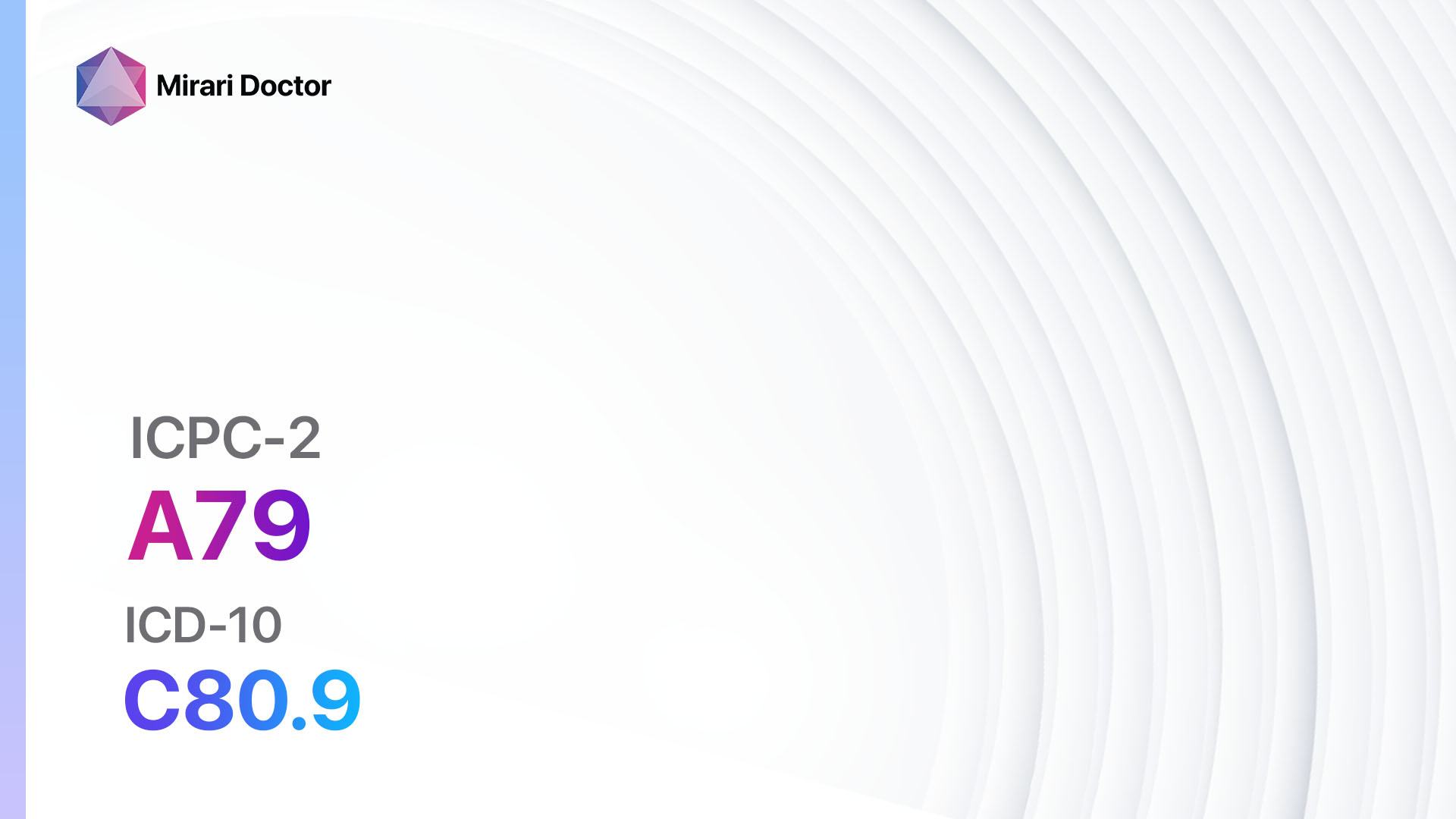
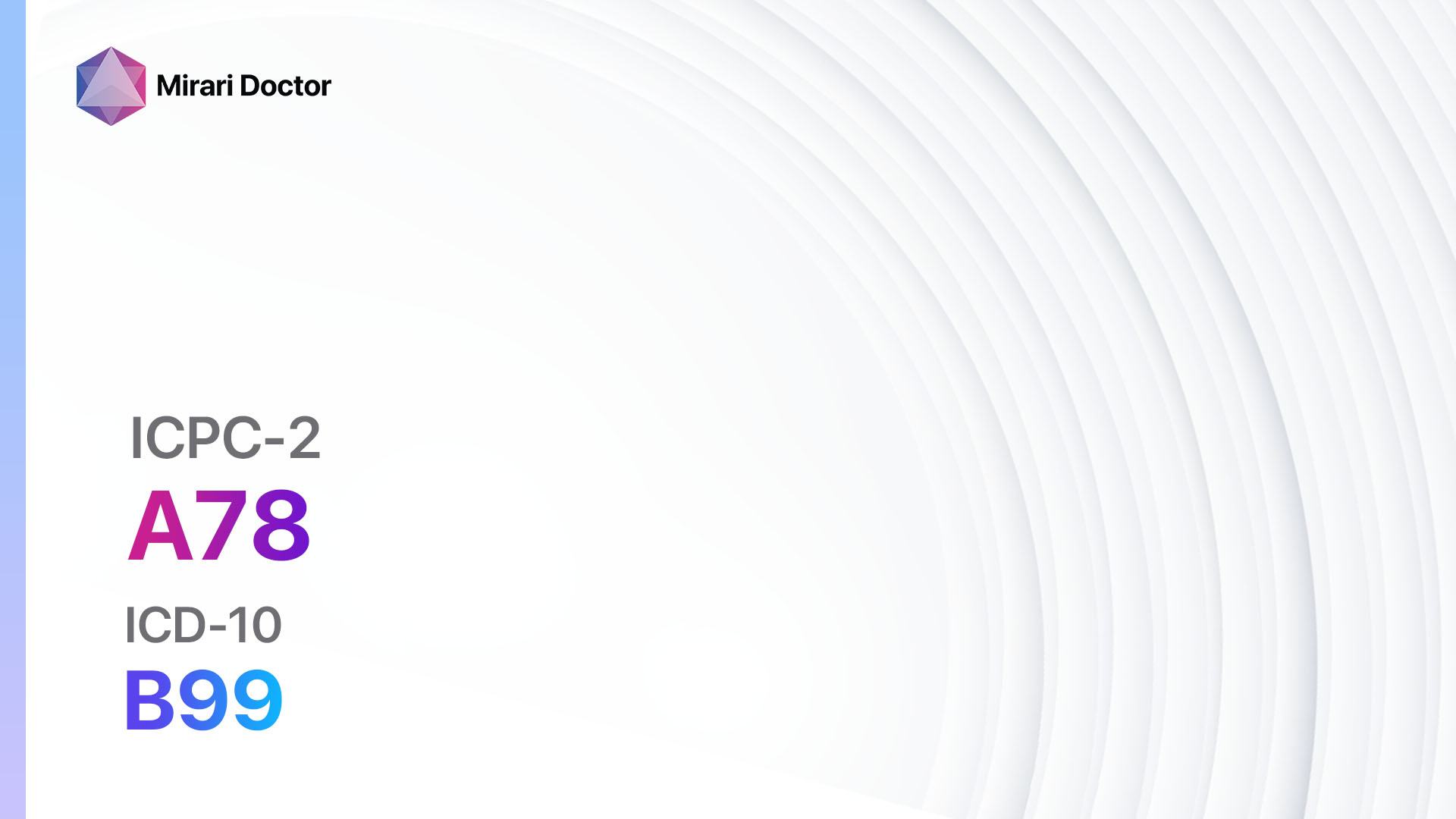
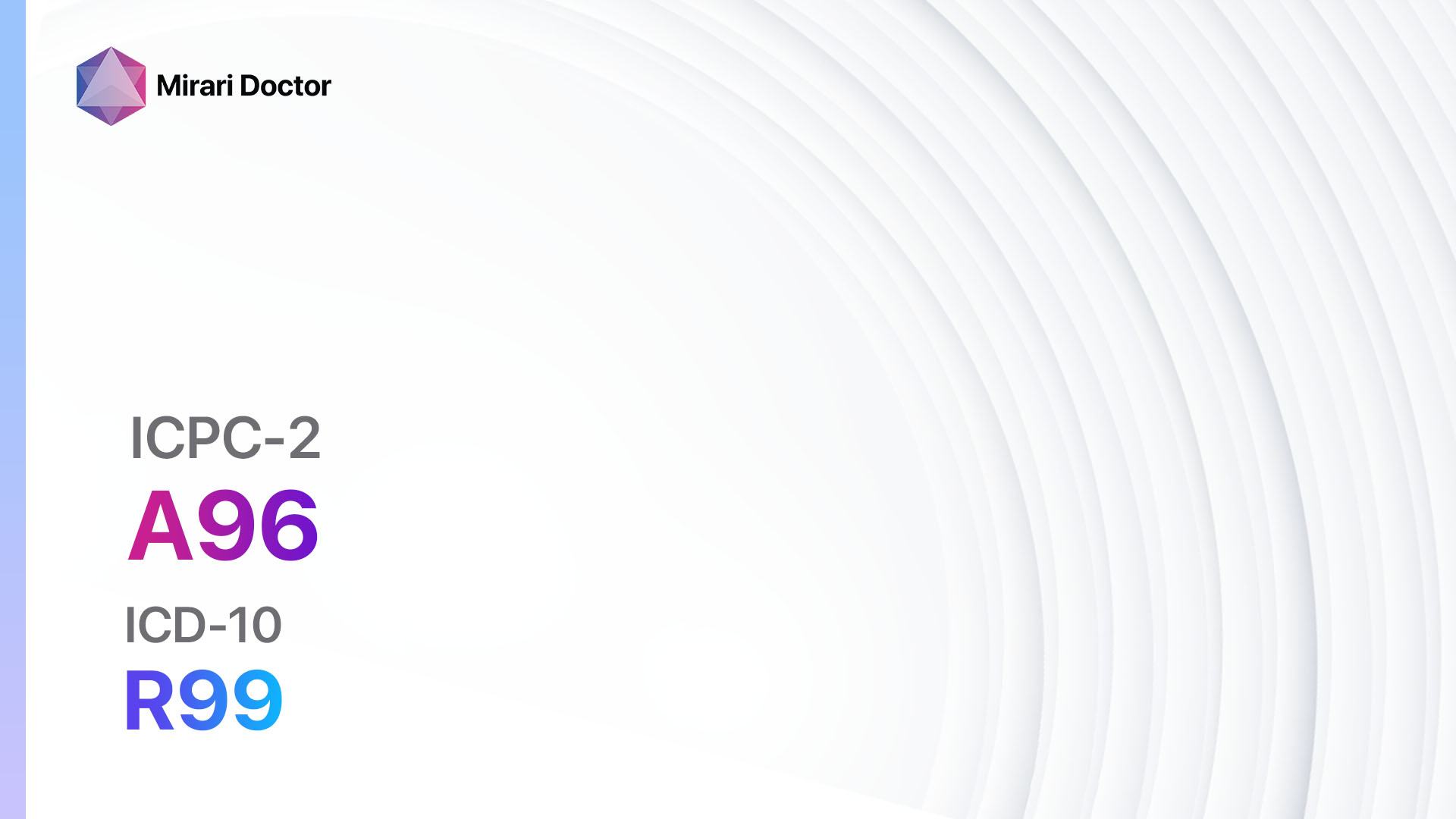
Codes
Symptoms
- Absence of breathing and heartbeat: The individual no longer breathes or has a detectable heartbeat[5].
- Pallor and coolness of the skin: The skin may appear pale and feel cool to the touch[6].
Causes
- Natural causes: Death can occur due to age-related decline in bodily functions, chronic illnesses, or acute medical conditions[7].
- Accidents or trauma: Sudden and unexpected accidents or traumatic events can lead to death[8].
- Terminal illnesses: Individuals with terminal illnesses may experience a decline in health that eventually leads to death[9].
Diagnostic Steps
Medical History
- Obtain a comprehensive medical history to gather relevant patient information, including any pre-existing medical conditions, previous illnesses, and family history of diseases[10].
- Inquire about any recent changes in the individual’s health or any symptoms that may have preceded their death.
Physical Examination
- Perform a thorough physical examination to assess for any signs of trauma or underlying medical conditions that may have contributed to the individual’s death.
- Document any visible signs, such as injuries, wounds, or abnormalities, that may provide clues about the cause of death.
Laboratory Tests
- Post-mortem blood tests: Analyze blood samples for toxicology screening to identify the presence of drugs, alcohol, or other substances that may have contributed to the individual’s death.
- Autopsy: A post-mortem examination of the body to determine the cause of death by examining organs, tissues, and bodily fluids.
Diagnostic Imaging
- X-rays: May be used to identify fractures, foreign objects, or other abnormalities that may have contributed to the individual’s death.
- CT scans or MRIs: Provide detailed images of internal organs and tissues, helping to identify any underlying conditions or injuries.
Other Tests
- Genetic testing: In certain cases, genetic testing may be performed to identify any inherited conditions or genetic abnormalities that may have contributed to the individual’s death.
- Microscopic examination: Tissue samples may be examined under a microscope to identify any cellular abnormalities or signs of disease.
Follow-up and Patient Education
- Provide support and counseling to the family and loved ones of the deceased, addressing their emotional needs and answering any questions they may have.
- Offer resources and information on grief counseling and support groups to help individuals cope with the loss.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for end-of-life care:
- Pain medications (e.g., Morphine, Fentanyl):
- Cost: Varies depending on the formulation and dosage.
- Contraindications: Hypersensitivity to opioids, severe respiratory depression.
- Side effects: Sedation, constipation, nausea.
- Severe side effects: Respiratory depression, hypotension.
- Drug interactions: CNS depressants, MAO inhibitors.
- Warning: Close monitoring of respiratory status is essential.
- Anti-anxiety medications (e.g., Lorazepam, Midazolam):
- Cost: Varies depending on the formulation and dosage.
- Contraindications: Acute narrow-angle glaucoma, respiratory depression.
- Side effects: Sedation, dizziness, confusion.
- Severe side effects: Respiratory depression, paradoxical reactions.
- Drug interactions: CNS depressants, opioids.
- Warning: Caution should be exercised in patients with compromised respiratory function.
- Anti-emetics (e.g., Ondansetron, Metoclopramide):
- Cost: Varies depending on the formulation and dosage.
- Contraindications: Hypersensitivity to the medication, intestinal obstruction.
- Side effects: Headache, constipation, drowsiness.
- Severe side effects: Torsades de pointes, extrapyramidal reactions.
- Drug interactions: Serotonergic drugs, QT-prolonging medications.
- Warning: Monitoring for QT interval prolongation is recommended.
- Anticholinergic medications (e.g., Scopolamine):
- Cost: Varies depending on the formulation and dosage.
- Contraindications: Glaucoma, urinary retention.
- Side effects: Dry mouth, blurred vision, constipation.
- Severe side effects: Delirium, hallucinations.
- Drug interactions: CNS depressants, antihistamines.
- Warning: Caution should be exercised in elderly patients due to increased risk of adverse effects.
- Antibiotics (e.g., Ceftriaxone, Metronidazole):
- Cost: Varies depending on the formulation and dosage.
- Contraindications: Hypersensitivity to the medication, severe liver disease.
- Side effects: Diarrhea, nausea, rash.
- Severe side effects: Anaphylaxis, Clostridium difficile infection.
- Drug interactions: Warfarin, oral contraceptives.
- Warning: Antibiotics should be used judiciously and only when necessary.
Alternative Drugs:
- Corticosteroids (e.g., Dexamethasone): May be used to reduce inflammation and manage symptoms in certain end-of-life conditions.
- Antidepressants (e.g., Sertraline): Can be prescribed to manage depression or anxiety in individuals experiencing end-of-life care.
- Antipsychotics (e.g., Haloperidol): May be used to manage delirium or agitation in individuals nearing the end of life.
- Benzodiazepines (e.g., Diazepam): Can be prescribed to manage anxiety or insomnia in individuals receiving end-of-life care.
- Bronchodilators (e.g., Albuterol): May be used to relieve shortness of breath in individuals with respiratory symptoms.
Surgical Procedures:
- Palliative surgery: Surgical procedures may be performed to alleviate symptoms or improve quality of life in individuals receiving end-of-life care. These procedures are aimed at providing comfort rather than curing the underlying condition.
Alternative Interventions
- Hospice care: Provides comprehensive support and comfort to individuals nearing the end of life, including pain management, emotional support, and assistance with daily activities. Cost: Covered by Medicare, Medicaid, and most private insurance plans.
- Music therapy: The use of music to promote relaxation, reduce anxiety, and provide emotional support. Cost: Varies depending on the provider and location.
- Massage therapy: Gentle manipulation of the body’s soft tissues to promote relaxation and alleviate pain. Cost: $50-$100 per session.
- Pet therapy: Interaction with trained animals to provide comfort and emotional support. Cost: Varies depending on the provider and location.
- Spiritual care: Support from religious or spiritual leaders to address the individual’s spiritual and emotional needs. Cost: Varies depending on the provider and location.
Lifestyle Interventions
- Emotional support: Encourage individuals to seek emotional support from family, friends, or support groups to cope with the emotional challenges associated with end-of-life care. Cost: Varies depending on the availability of support groups and counseling services.
- Nutritional support: Ensure individuals receive adequate nutrition and hydration to maintain their comfort and well-being. Cost: Varies depending on the individual’s dietary needs and preferences.
- Comfort measures: Provide a comfortable and peaceful environment, including pain management, assistance with personal care, and maintaining a calm and soothing atmosphere. Cost: Varies depending on the individual’s preferences and needs.
- Respite care: Offer temporary relief to caregivers by providing professional care for the individual, allowing caregivers to take a break and attend to their own well-being. Cost: Varies depending on the provider and location.
- Advance care planning: Encourage individuals to discuss and document their preferences for end-of-life care, including decisions regarding life-sustaining treatments and funeral arrangements. Cost: Varies depending on the individual’s preferences and legal requirements.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: Localized Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: Localized Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: Localized Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immuno) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immuno) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immuno) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Death effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Death. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Bernat, J. L. (2013). On the definition and criterion of death. Handbook of Clinical Neurology, 118, 419-435.
- Kübler-Ross, E. (2009). On death and dying: What the dying have to teach doctors, nurses, clergy and their own families. Taylor & Francis.
- World Organization of Family Doctors. (2016). ICPC-2: International Classification of Primary Care (2nd ed.). Oxford University Press.
- World Health Organization. (2019). International Statistical Classification of Diseases and Related Health Problems (11th ed.).
- Shemie, S. D., Hornby, L., Baker, A., Teitelbaum, J., Torrance, S., Young, K., … & Noel, L. (2014). International guideline development for the determination of death. Intensive Care Medicine, 40(6), 788-797.
- Pattison, N. (2008). Care of the dying and deceased patient: a practical guide for nurses. John Wiley & Sons.
- Heron, M. (2019). Deaths: Leading causes for 2017. National Vital Statistics Reports, 68(6), 1-77.
- Rhee, C., Joseph, D. A., & Dantes, R. B. (2019). Epidemiology of and risk factors for deaths from unintentional injury among adults aged 65 years or older. Journal of the American Geriatrics Society, 67(9), 1907-1912.
- Murray, S. A., Kendall, M., Boyd, K., & Sheikh, A. (2005). Illness trajectories and palliative care. BMJ, 330(7498), 1007-1011.
- Oppewal, F., & Meyboom-de Jong, B. (2001). Family members’ experiences of the last phase of a terminal illness at home. Scandinavian Journal of Caring Sciences, 15(1), 35-42.
Related articles
Made in USA