Introduction
Rubella, also known as German measles, is a contagious viral infection that primarily affects children and young adults[1]. It is characterized by a rash, fever, and swollen lymph nodes[2]. Rubella can have serious consequences for pregnant women, as it can cause birth defects in the developing fetus[3]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of rubella.
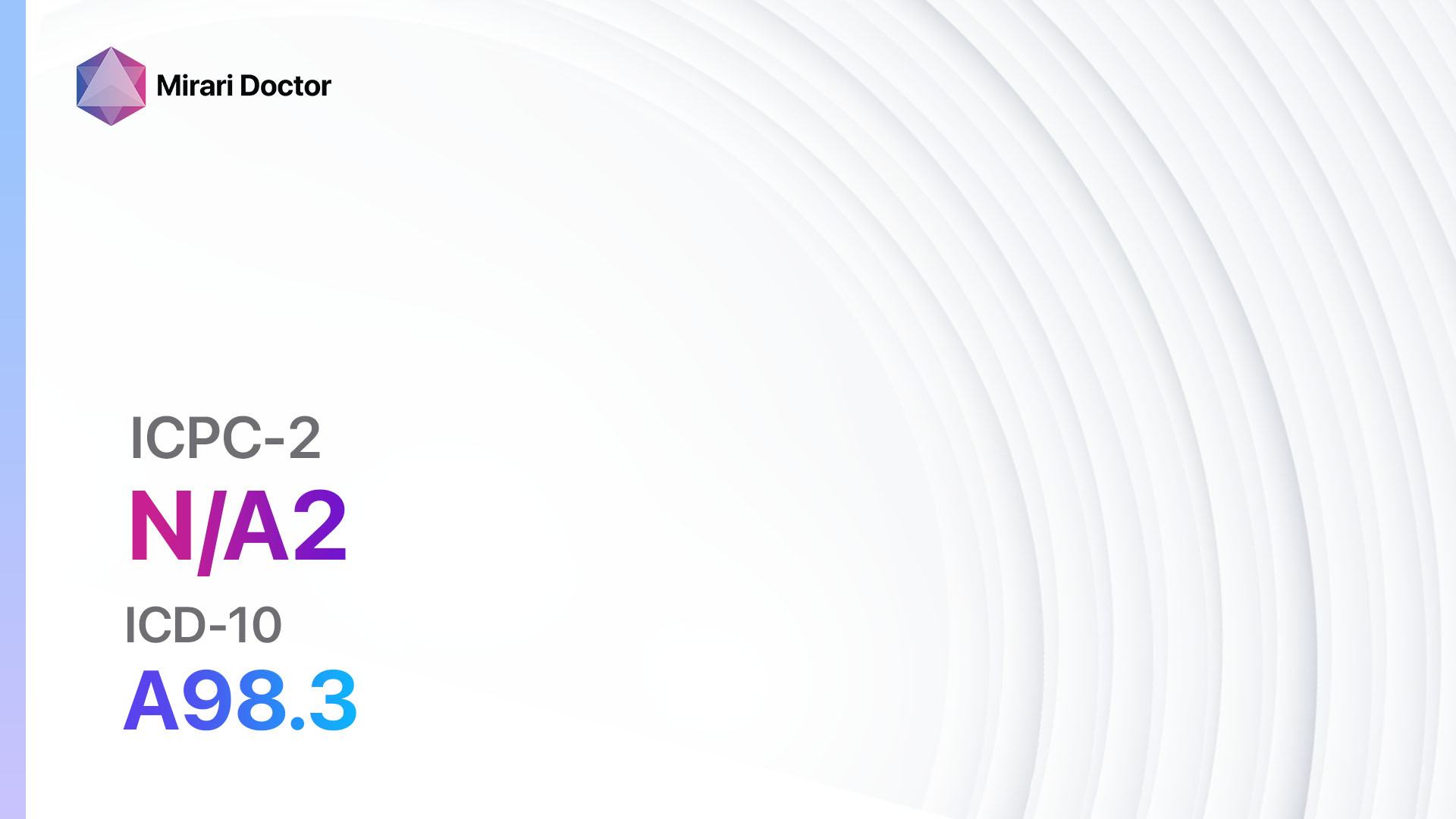
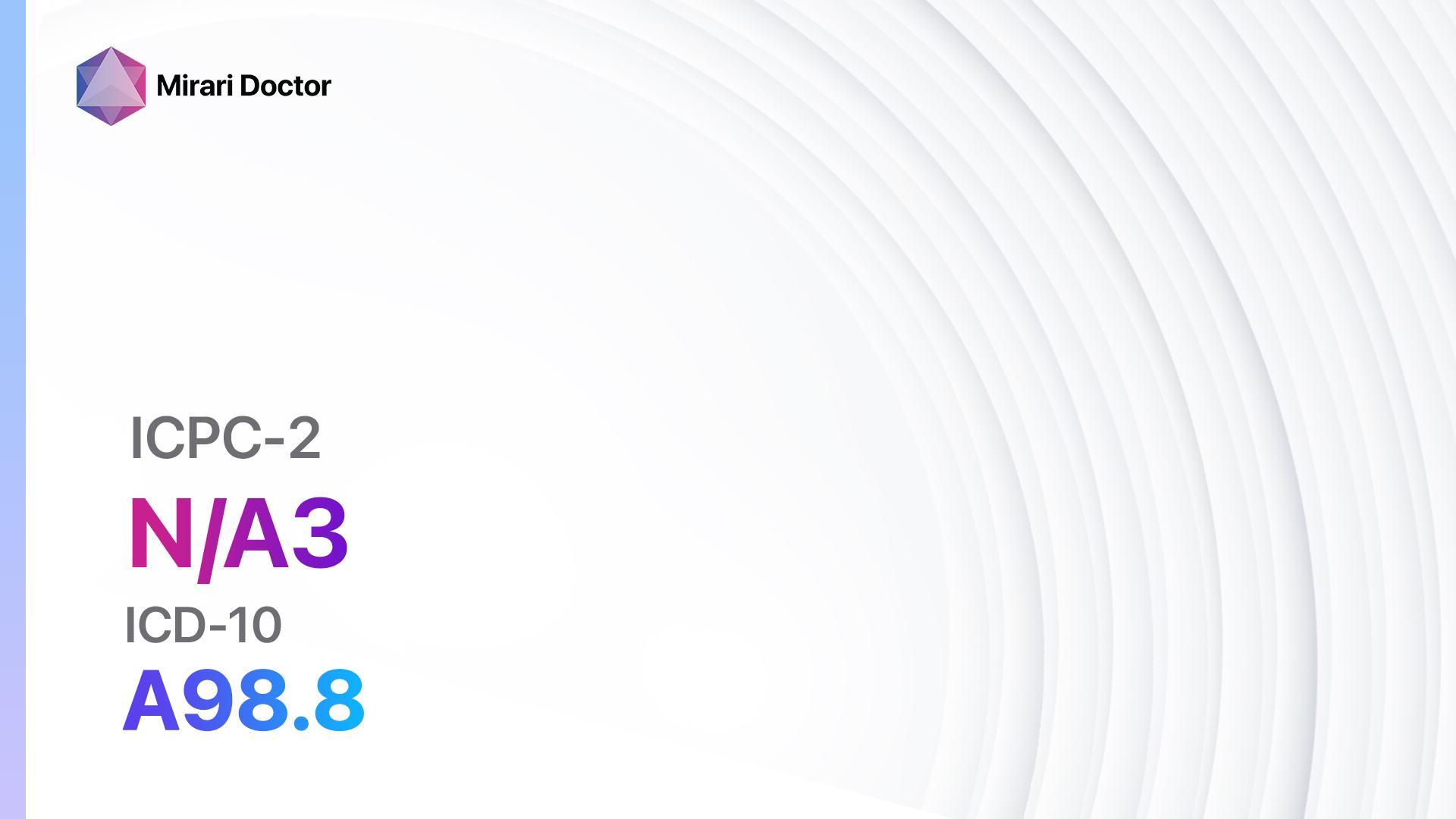
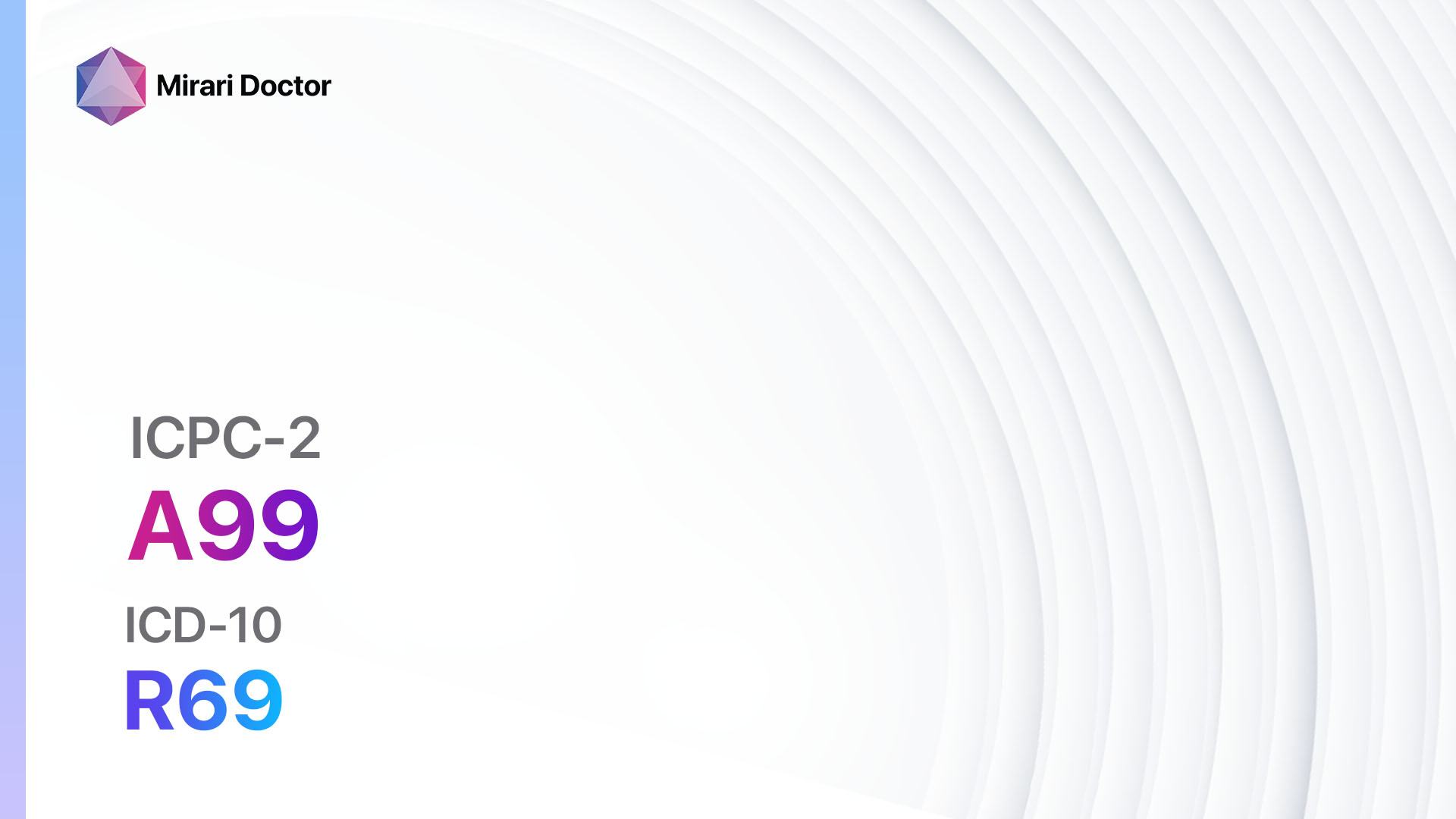
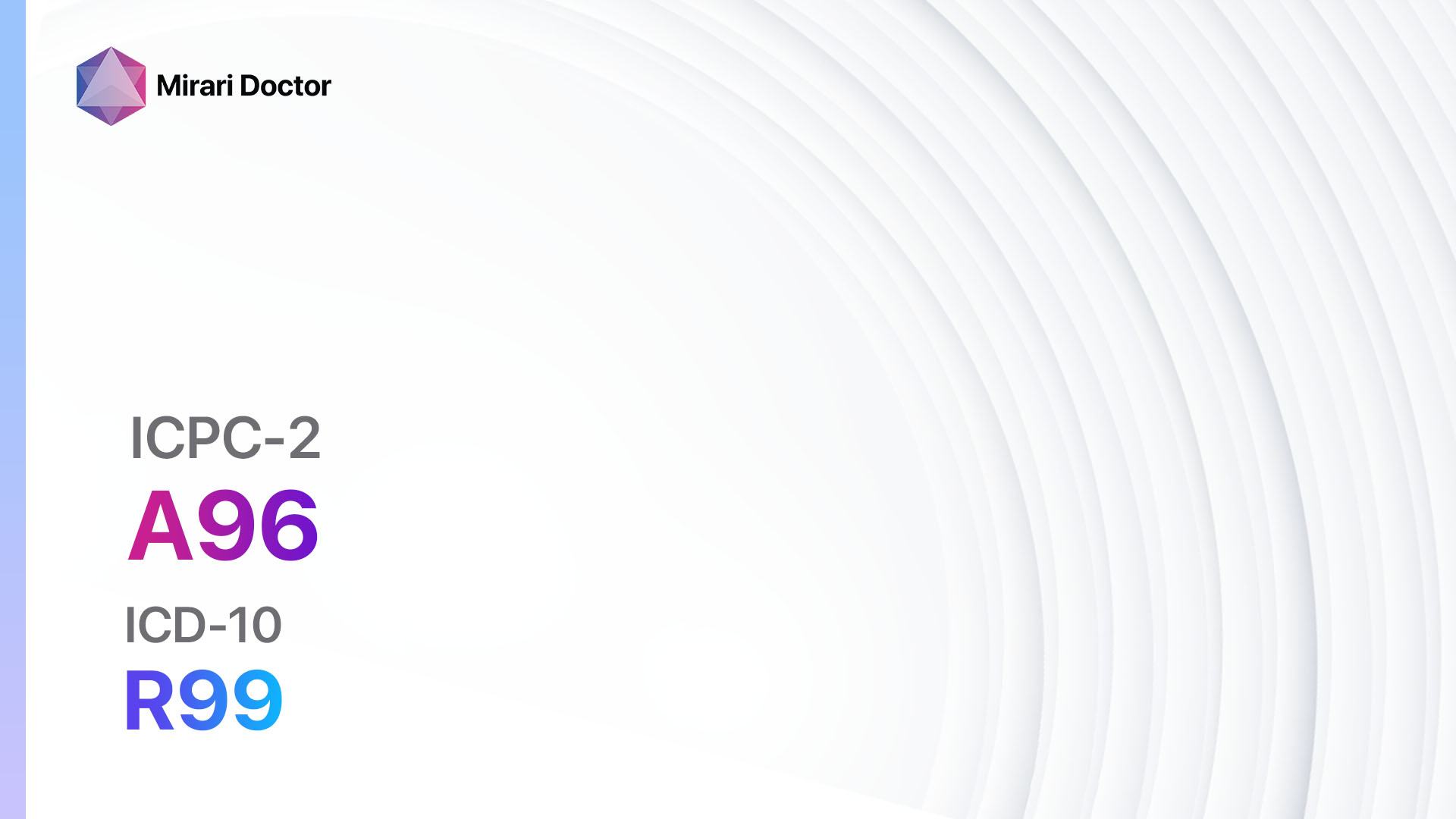
Codes
Symptoms
- Rash: The most common symptom of rubella is a rash that starts on the face and spreads to the rest of the body. The rash is typically pink or light red and may be accompanied by itching[4].
- Fever: Rubella is often accompanied by a low-grade fever, usually less than 102°F (38.9°C)[5].
- Swollen lymph nodes: Lymph nodes, particularly those located behind the ears and at the back of the neck, may become swollen and tender[6].
Causes
- Rubella virus: Rubella is caused by the rubella virus, which is transmitted from person to person through respiratory droplets. It can also be transmitted from a pregnant woman to her unborn baby[7].
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the onset and duration of the rash, presence of fever, and any other associated symptoms.
- Inquire about the patient’s vaccination history, particularly if they have received the MMR (measles, mumps, and rubella) vaccine[8].
- Ask about any recent exposure to individuals with rubella or suspected cases of rubella.
Physical Examination
- Perform a thorough physical examination, paying particular attention to the presence and characteristics of the rash.
- Palpate the lymph nodes to assess for swelling and tenderness.
- Check for any other signs or symptoms that may be indicative of rubella, such as fever or joint pain.
Laboratory Tests
- Rubella IgM antibody test: This blood test detects the presence of IgM antibodies, which indicate a recent rubella infection[9].
- Rubella IgG antibody test: This blood test detects the presence of IgG antibodies, which indicate a past rubella infection or immunity due to vaccination[10].
- Complete blood count (CBC): A CBC may be performed to assess for any abnormalities, such as leukopenia or thrombocytopenia, which can occur in rubella.
Diagnostic Imaging
- Diagnostic imaging is not typically necessary for the diagnosis of rubella. However, in cases where complications are suspected, such as encephalitis or pneumonia, imaging modalities such as CT scans or MRIs may be used to assess for these complications.
Other Tests
- Viral culture: A viral culture may be performed to isolate and identify the rubella virus from a sample taken from the patient’s throat or urine.
- Amniocentesis: In pregnant women, amniocentesis may be performed to detect the presence of rubella virus in the amniotic fluid.
Follow-up and Patient Education
- Provide the patient with information about rubella, including its transmission, symptoms, and potential complications.
- Emphasize the importance of vaccination, particularly for individuals who are planning to become pregnant or are in close contact with pregnant women.
- Advise the patient to avoid contact with pregnant women or individuals who are immunocompromised until they are no longer contagious.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Rubella:
- Acetaminophen (e.g., Tylenol):
- Cost: $5-$10 for a bottle of generic acetaminophen.
- Contraindications: Hypersensitivity to acetaminophen.
- Side effects: Rare, but can include allergic reactions or liver damage with high doses.
- Severe side effects: Severe allergic reactions, liver failure.
- Drug interactions: Alcohol, warfarin.
- Warning: Do not exceed the recommended dosage.
- Antihistamines (e.g., Benadryl, Claritin):
- Cost: $5-$15 for a box of generic antihistamines.
- Contraindications: Hypersensitivity to antihistamines.
- Side effects: Drowsiness, dry mouth.
- Severe side effects: Rare, but can include severe allergic reactions.
- Drug interactions: Sedatives, alcohol.
- Warning: May cause drowsiness, avoid driving or operating heavy machinery.
- Topical corticosteroids (e.g., hydrocortisone cream):
- Cost: $5-$15 for a tube of generic hydrocortisone cream.
- Contraindications: Hypersensitivity to corticosteroids.
- Side effects: Rare, but can include skin thinning or discoloration.
- Severe side effects: Rare, but can include severe allergic reactions.
- Drug interactions: None known.
- Warning: Use only as directed, avoid applying to broken or infected skin.
- Antiviral medications (e.g., ribavirin):
- Cost: $100-$500 for a course of generic ribavirin.
- Contraindications: Hypersensitivity to ribavirin.
- Side effects: Fatigue, nausea, anemia.
- Severe side effects: Rare, but can include severe allergic reactions or liver toxicity.
- Drug interactions: None known.
- Warning: Use only under the supervision of a healthcare professional.
- Immunoglobulin:
- Cost: $500-$1000 for a dose of immunoglobulin.
- Contraindications: Hypersensitivity to immunoglobulin.
- Side effects: Rare, but can include headache, fever, or allergic reactions.
- Severe side effects: Rare, but can include severe allergic reactions or blood clots.
- Drug interactions: None known.
- Warning: Use only under the supervision of a healthcare professional.
Alternative Drugs:
- No alternative drugs are currently recommended for the treatment of rubella.
Surgical Procedures:
- No surgical procedures are indicated for the treatment of rubella.
Alternative Interventions
- Rest and hydration: Adequate rest and hydration can help support the immune system and promote recovery. Cost: None.
- Herbal remedies: Some herbal remedies, such as echinacea or elderberry, may have immune-boosting properties. Cost: Varies depending on the specific remedy.
- Homeopathic remedies: Homeopathic remedies, such as pulsatilla or belladonna, may be used to alleviate symptoms. Cost: Varies depending on the specific remedy.
- Naturopathic treatments: Naturopathic treatments, such as hydrotherapy or dietary modifications, may be recommended to support the body’s natural healing processes. Cost: Varies depending on the specific treatment.
Lifestyle Interventions
- Isolation and quarantine: Individuals with rubella should be isolated to prevent the spread of the virus. Cost: None.
- Good hygiene practices: Practicing good hygiene, such as regular handwashing, can help prevent the spread of rubella. Cost: None.
- Vaccination: Vaccination is the most effective way to prevent rubella. Cost: Varies depending on the location and availability of the vaccine.
- Avoidance of crowded places: Individuals with rubella should avoid crowded places to minimize the risk of transmission. Cost: None.
- Supportive care: Providing supportive care, such as rest, fluids, and over-the-counter medications, can help alleviate symptoms. Cost: Varies depending on the specific medications and treatments used.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – A74 Rubella (ICD-10:B06)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Rubella effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Rubella. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Centers for Disease Control and Prevention. (2021). Rubella (German Measles, Three-Day Measles). https://www.cdc.gov/rubella/index.html
- Mayo Clinic. (2021). Rubella. https://www.mayoclinic.org/diseases-conditions/rubella/symptoms-causes/syc-20377310
- World Health Organization. (2020). Rubella. https://www.who.int/news-room/fact-sheets/detail/rubella
- American Academy of Pediatrics. (2021). Rubella (German Measles). In D. W. Kimberlin, M. T. Brady, M. A. Jackson, & S. S. Long (Eds.), Red Book: 2021-2024 Report of the Committee on Infectious Diseases (pp. 627-631). American Academy of Pediatrics.
- Banatvala, J. E., & Brown, D. W. (2004). Rubella. The Lancet, 363(9415), 1127-1137. https://doi.org/10.1016/S0140-6736(04)15897-2
- Dontigny, L., Arsenault, M. Y., & Martel, M. J. (2008). Rubella in pregnancy. Journal of Obstetrics and Gynaecology Canada, 30(2), 152-158. https://doi.org/10.1016/S1701-2163(16)32737-5
- Reef, S. E., & Plotkin, S. A. (2018). Rubella Vaccines. In S. A. Plotkin, W. A. Orenstein, P. A. Offit, & K. M. Edwards (Eds.), Plotkin’s Vaccines (7th ed., pp. 970-1000). Elsevier.
- Zimmerman, L. A., Muscat, M., Singh, S., Ben Mamou, M., Jankovic, D., Datta, S., & Grant, G. B. (2019). Progress Toward Rubella and Congenital Rubella Syndrome Control and Elimination – Worldwide, 2000-2018. MMWR. Morbidity and Mortality Weekly Report, 68(39), 855-859. https://doi.org/10.15585/mmwr.mm6839a5
- Tipples, G. A., & Hiebert, J. (2011). Detection of measles, mumps,a and rubella viruses. In D. Liu (Ed.), Molecular Detection of Human Viral Pathogens (pp. 501-510). CRC Press.
- Skendzel, L. P. (1996). Rubella immunity: Defining the level of protective antibody. American Journal of Clinical Pathology, 106(2), 170-174. https://doi.org/10.1093/ajcp/106.2.170
Related articles
Made in USA