Introduction
Malaria is a life-threatening disease caused by parasites that are transmitted to humans through the bites of infected female Anopheles mosquitoes[1]. It is a significant global health concern, particularly in tropical and subtropical regions[2]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of malaria.
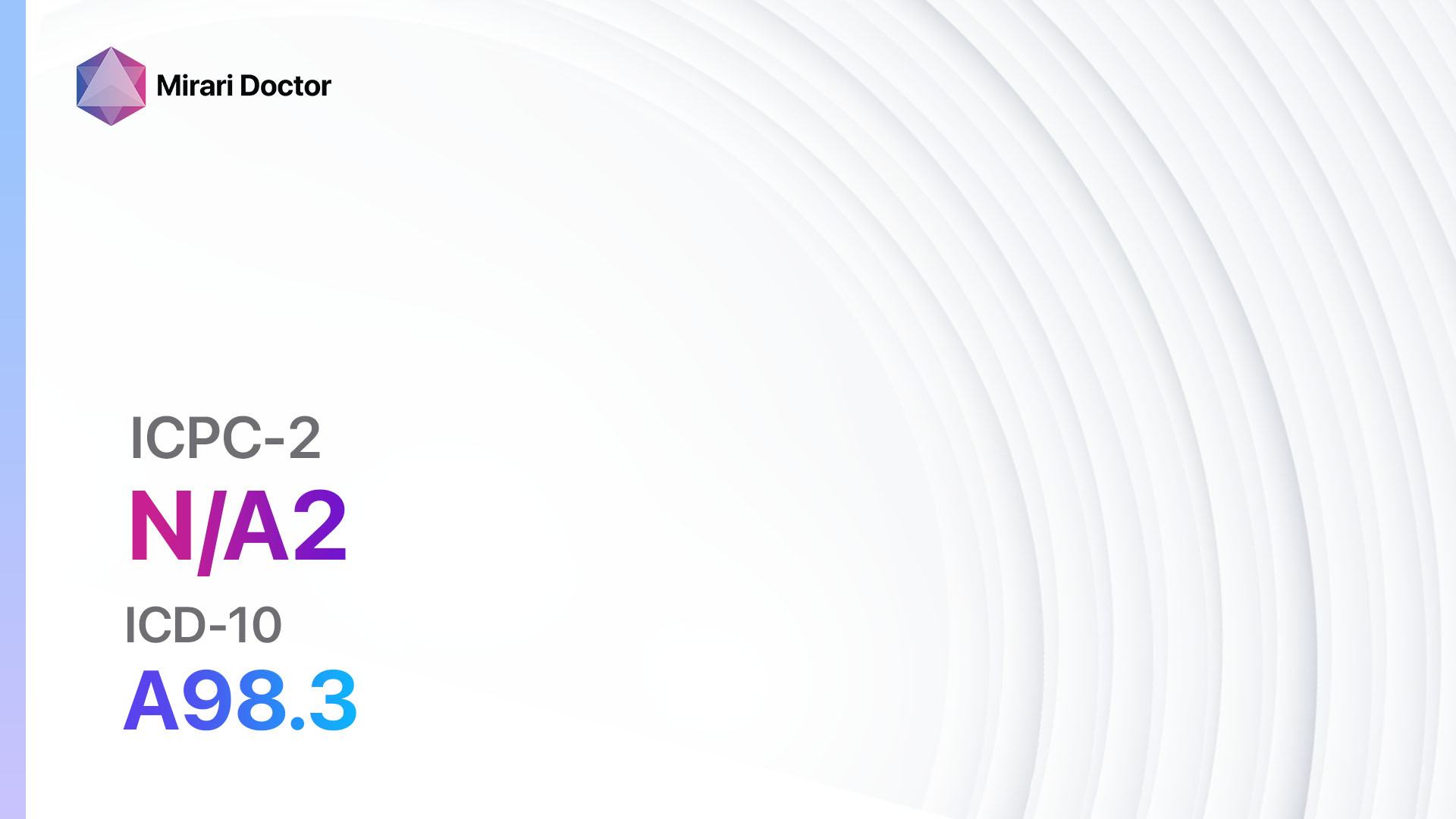
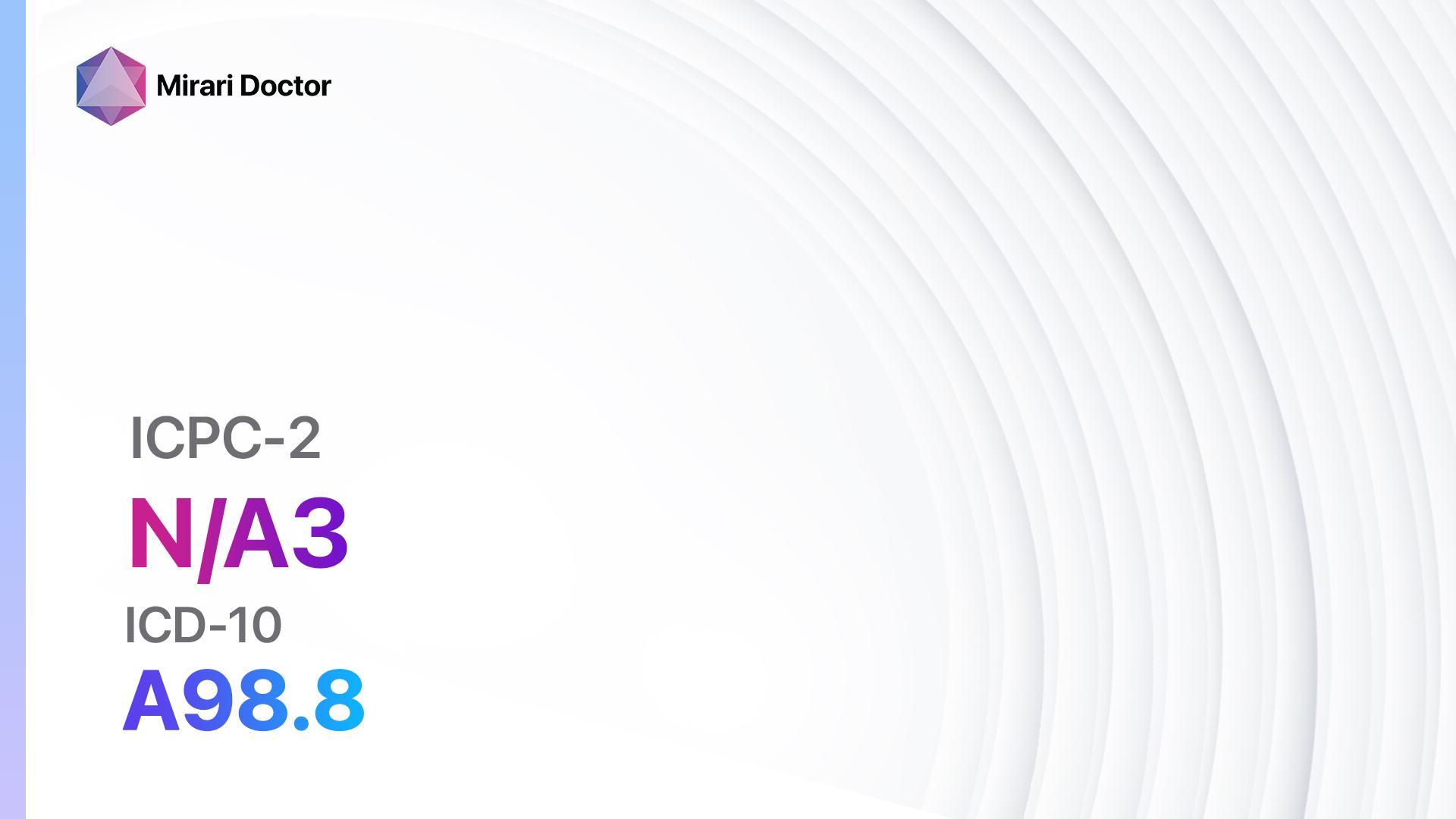
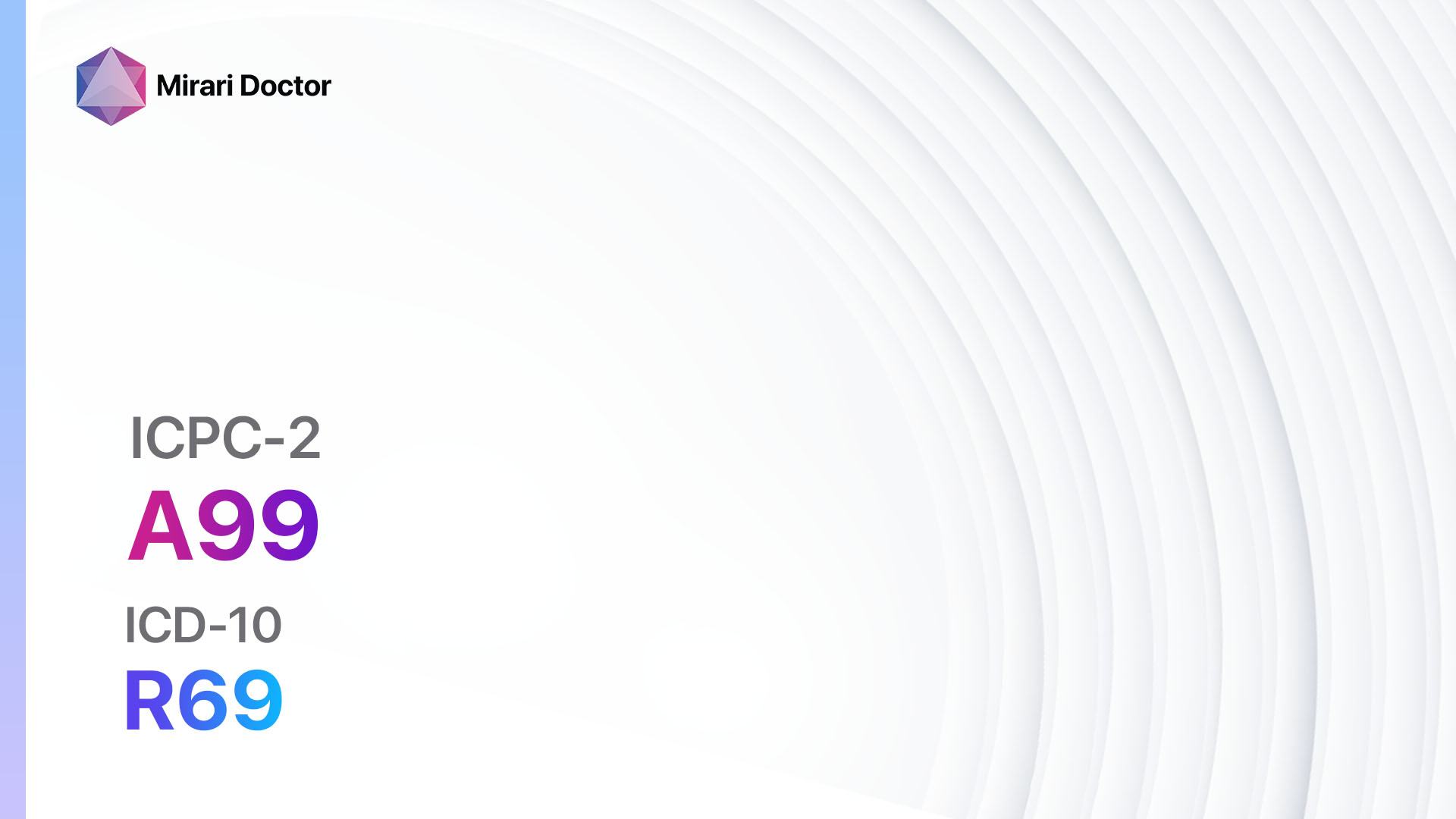
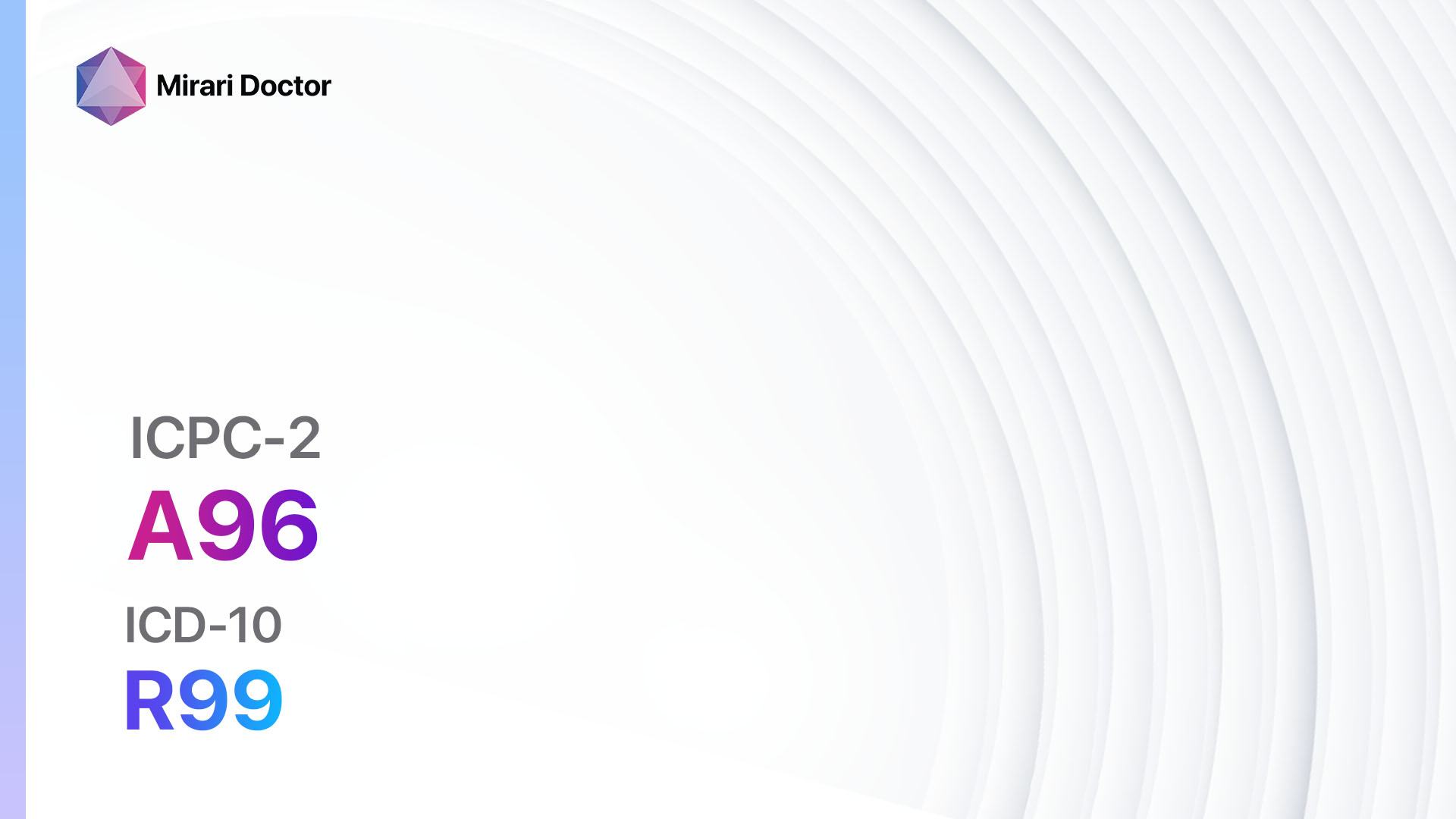
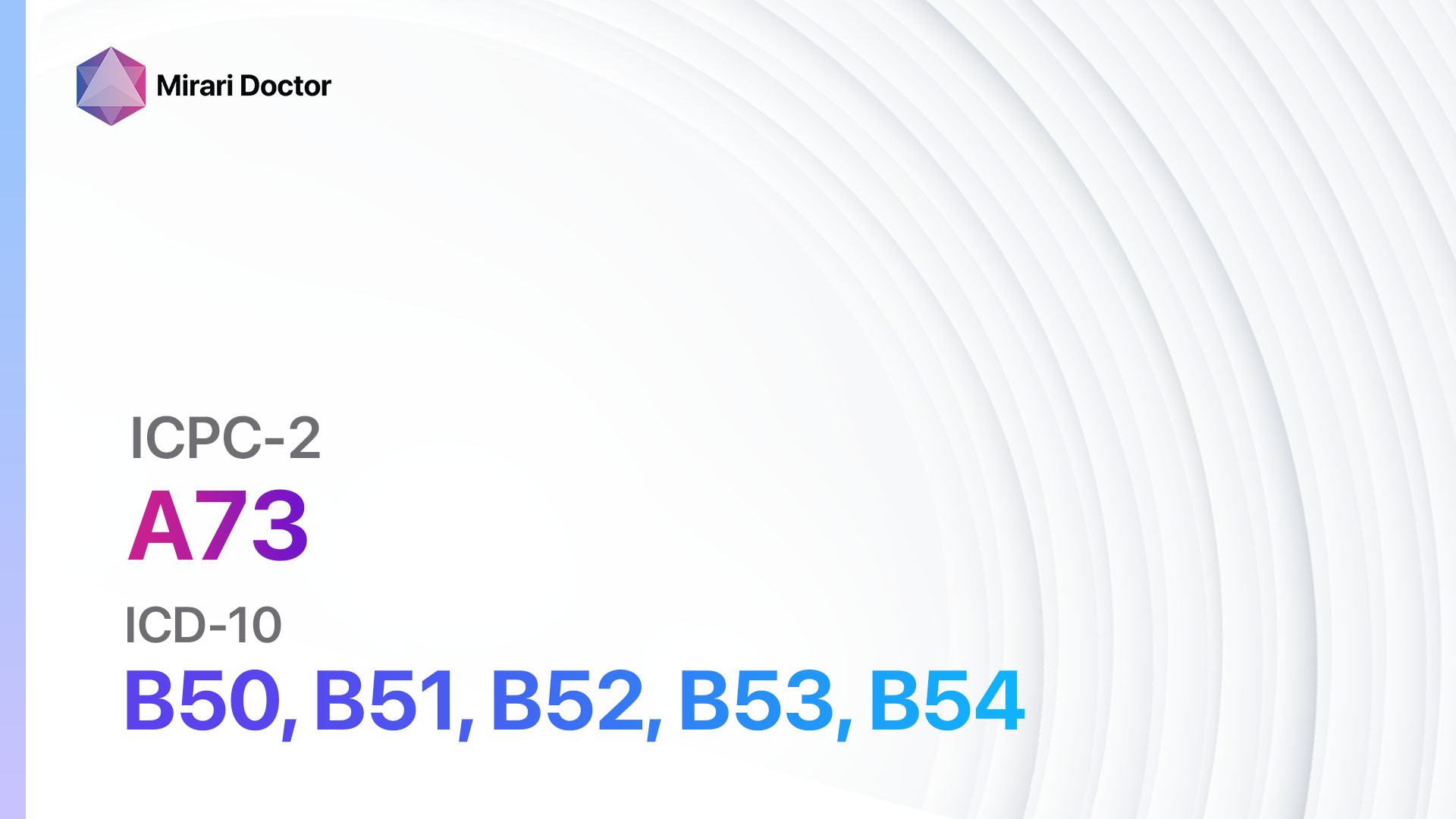
Codes
Symptoms
- Fever: Malaria is often characterized by recurrent episodes of fever, which may be accompanied by chills and sweating[3].
- Headache: Many individuals with malaria experience severe headaches[4].
- Fatigue: Malaria can cause extreme tiredness and weakness[5].
- Muscle and joint pain: Individuals with malaria may experience muscle and joint pain, which can be debilitating[6].
- Nausea and vomiting: Malaria can cause gastrointestinal symptoms, including nausea and vomiting[7].
- Anemia: Malaria can lead to a decrease in red blood cells, resulting in anemia[8].
- Jaundice: In severe cases, malaria can cause yellowing of the skin and eyes[9].
- Respiratory distress: Severe malaria can lead to respiratory distress and difficulty breathing[10].
- Neurological symptoms: In some cases, malaria can cause seizures, confusion, and coma.
Causes
- Plasmodium parasites: Malaria is caused by infection with Plasmodium parasites, which are transmitted to humans through the bites of infected mosquitoes.
- Anopheles mosquitoes: Female Anopheles mosquitoes are the primary vectors for transmitting malaria to humans.
Diagnostic Steps
Medical History
- Gather information about the patient’s travel history, particularly if they have recently visited a malaria-endemic region.
- Ask about symptoms, including the presence of fever, headache, fatigue, and other characteristic symptoms of malaria.
- Inquire about any previous episodes of malaria or exposure to malaria.
Physical Examination
- Perform a thorough physical examination, paying particular attention to signs of anemia, jaundice, and enlarged spleen or liver.
- Check for the presence of fever and assess the patient’s general appearance and level of consciousness.
Laboratory Tests
- Blood smear: A blood smear is the gold standard for diagnosing malaria. It involves examining a sample of the patient’s blood under a microscope to identify the presence of Plasmodium parasites.
- Rapid diagnostic tests (RDTs): RDTs are simple, point-of-care tests that can detect malaria antigens in the patient’s blood. They provide rapid results and are particularly useful in resource-limited settings.
- Polymerase chain reaction (PCR): PCR can be used to detect and identify specific Plasmodium species in the patient’s blood. It is a highly sensitive and specific test but is not widely available in all healthcare settings.
Diagnostic Imaging
- Diagnostic imaging is not typically used in the diagnosis of malaria.
Other Tests
- Additional laboratory tests may be necessary to assess the patient’s overall health and identify any complications associated with severe malaria. These may include:
- Complete blood count (CBC) to assess for anemia and other blood abnormalities.
- Liver function tests to evaluate liver function and detect any liver damage.
- Kidney function tests to assess renal function.
- Blood glucose levels to screen for hypoglycemia, which can occur in severe malaria.
Follow-up and Patient Education
- Provide appropriate treatment based on the diagnosis and severity of the malaria infection.
- Educate the patient about the importance of completing the full course of treatment and taking preventive measures to avoid future infections.
- Advise the patient to seek medical attention if symptoms worsen or if new symptoms develop.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Malaria:
- Artemether-Lumefantrine:
- Cost: $1-$3 per treatment course.
- Contraindications: Hypersensitivity to artemether or lumefantrine.
- Side effects: Nausea, vomiting, headache.
- Severe side effects: Cardiac arrhythmias, severe allergic reactions.
- Drug interactions: CYP3A4 inducers or inhibitors.
- Warning: Not recommended for patients with severe malaria or severe hepatic impairment.
- Chloroquine:
- Cost: $0.50-$1 per treatment course.
- Contraindications: Hypersensitivity to chloroquine or 4-aminoquinoline compounds.
- Side effects: Nausea, vomiting, headache.
- Severe side effects: Retinopathy, cardiomyopathy.
- Drug interactions: CYP2D6 inhibitors, drugs that prolong QT interval.
- Warning: Resistance to chloroquine is widespread in many malaria-endemic regions.
- Mefloquine:
- Cost: $1-$2 per treatment course.
- Contraindications: History of psychiatric disorders, seizures, or cardiac conduction disorders.
- Side effects: Nausea, vomiting, dizziness.
- Severe side effects: Psychiatric symptoms, seizures.
- Drug interactions: CYP3A4 inducers or inhibitors.
- Warning: Not recommended for patients with a history of psychiatric disorders.
- Doxycycline:
- Cost: $0.10-$0.50 per treatment course.
- Contraindications: Hypersensitivity to tetracyclines, pregnancy, children under 8 years old.
- Side effects: Nausea, vomiting, photosensitivity.
- Severe side effects: Severe skin reactions, esophageal ulceration.
- Drug interactions: Antacids, iron supplements, warfarin.
- Warning: Not recommended for pregnant women or children under 8 years old.
- Atovaquone-Proguanil:
- Cost: $3-$5 per treatment course.
- Contraindications: Hypersensitivity to atovaquone or proguanil.
- Side effects: Nausea, vomiting, headache.
- Severe side effects: Severe skin reactions, hepatotoxicity.
- Drug interactions: Rifampin, rifabutin, efavirenz.
- Warning: Not recommended for patients with severe renal impairment.
Alternative Drugs:
- Quinine:
- Cost: $0.50-$1 per treatment course.
- Contraindications: Hypersensitivity to quinine or quinidine, glucose-6-phosphate dehydrogenase (G6PD) deficiency.
- Side effects: Nausea, vomiting, tinnitus.
- Severe side effects: Cinchonism, hemolytic anemia (in patients with G6PD deficiency).
- Drug interactions: CYP3A4 inducers or inhibitors.
- Warning: Not recommended as first-line treatment due to potential side effects.
- Primaquine:
- Cost: $0.50-$1 per treatment course.
- Contraindications: Hypersensitivity to primaquine, pregnancy, breastfeeding, G6PD deficiency.
- Side effects: Nausea, vomiting, abdominal pain.
- Severe side effects: Hemolytic anemia (in patients with G6PD deficiency).
- Drug interactions: CYP2D6 inhibitors, drugs that prolong QT interval.
- Warning: Not recommended for pregnant women, breastfeeding women, or patients with G6PD deficiency.
- Artesunate:
- Cost: $1-$3 per treatment course.
- Contraindications: Hypersensitivity to artesunate or other artemisinin derivatives.
- Side effects: Nausea, vomiting, headache.
- Severe side effects: Cardiac arrhythmias, severe allergic reactions.
- Drug interactions: CYP3A4 inducers or inhibitors.
- Warning: Not recommended as monotherapy due to potential resistance.
Surgical Procedures:
- Surgical intervention is not typically required for the treatment of malaria.
Alternative Interventions
- Herbal remedies: Some herbal remedies, such as Artemisia annua (sweet wormwood), have been traditionally used for the treatment of malaria. However, their effectiveness and safety have not been well-established. Cost: Varies depending on the specific herb or remedy.
- Homeopathy: Homeopathic remedies may be used as adjunctive therapy for malaria. However, there is limited scientific evidence to support their effectiveness. Cost: Varies depending on the specific remedy and practitioner fees.
- Traditional medicine: Traditional medicine practices, such as Ayurveda or Traditional Chinese Medicine, may offer alternative treatment options for malaria. However, their efficacy and safety should be evaluated on an individual basis. Cost: Varies depending on the specific treatment and practitioner fees.
Lifestyle Interventions
- Insecticide-treated bed nets: Sleeping under insecticide-treated bed nets can help prevent mosquito bites and reduce the risk of malaria transmission. Cost: $5-$10 per bed net.
- Indoor residual spraying: Applying insecticides to the interior walls of houses can help kill mosquitoes and reduce malaria transmission. Cost: Varies depending on the size of the house and the insecticide used.
- Protective clothing: Wearing long-sleeved shirts, long pants, and socks can help protect against mosquito bites. Cost: Varies depending on the clothing items purchased.
- Mosquito repellents: Applying mosquito repellents containing DEET, picaridin, or other recommended ingredients can help prevent mosquito bites. Cost: $5-$15 per bottle.
- Environmental modifications: Removing stagnant water sources and improving drainage can help reduce mosquito breeding sites. Cost: Varies depending on the specific modifications required.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – A73 Malaria (ICD-10:B50, B51, B52, B53, B54)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Malaria effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Malaria. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- World Health Organization. (2021). Malaria. https://www.who.int/news-room/fact-sheets/detail/malaria
- Centers for Disease Control and Prevention. (2021). About Malaria. https://www.cdc.gov/malaria/about/index.html
- Bartoloni, A., & Zammarchi, L. (2012). Clinical aspects of uncomplicated and severe malaria. Mediterranean Journal of Hematology and Infectious Diseases, 4(1), e2012026. https://doi.org/10.4084/MJHID.2012.026
- Garg, R. K., Karak, B., & Misra, S. (1998). Neurological manifestations of malaria: an update. Neurology India, 46(2), 85-91.
- Suh, K. N., Kain, K. C., & Keystone, J. S. (2004). Malaria. CMAJ : Canadian Medical Association Journal, 170(11), 1693-1702. https://doi.org/10.1503/cmaj.1030418
- Anstey, N. M., Russell, B., Yeo, T. W., & Price, R. N. (2009). The pathophysiology of vivax malaria. Trends in Parasitology, 25(5), 220-227. https://doi.org/10.1016/j.pt.2009.02.003
- Mohapatra, M. K., Dash, L. K., Barih, P. K., & Karua, P. C. (2012). Profile of mixed species (Plasmodium vivax and falciparum) malaria in adults. The Journal of the Association of Physicians of India, 60, 20-24.
- Menendez, C., Fleming, A. F., & Alonso, P. L. (2000). Malaria-related anaemia. Parasitology Today, 16(11), 469-476. https://doi.org/10.1016/s0169-4758(00)01774-9
- Mishra, S. K., Mohanty, S., Satpathy, S. K., & Mohapatra, D. N. (2007). Cerebral malaria in adults — a description of 526 cases admitted to Ispat General Hospital in Rourkela, India. Annals of Tropical Medicine and Parasitology, 101(3), 187-193. https://doi.org/10.1179/136485907X157059
- Taylor, W. R., Hanson, J., Turner, G. D., White, N. J., & Dondorp, A. M. (2012). Respiratory manifestations of malaria. Chest, 142(2), 492-505. https://doi.org/10.1378/chest.11-2655
Related articles
Made in USA