Introduction
Gonorrhoea is a sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae. It is a common infection that can affect both men and women[1]. The aim of this guide is to provide healthcare professionals with a comprehensive procedural guide for diagnosing and managing gonorrhoea in males.
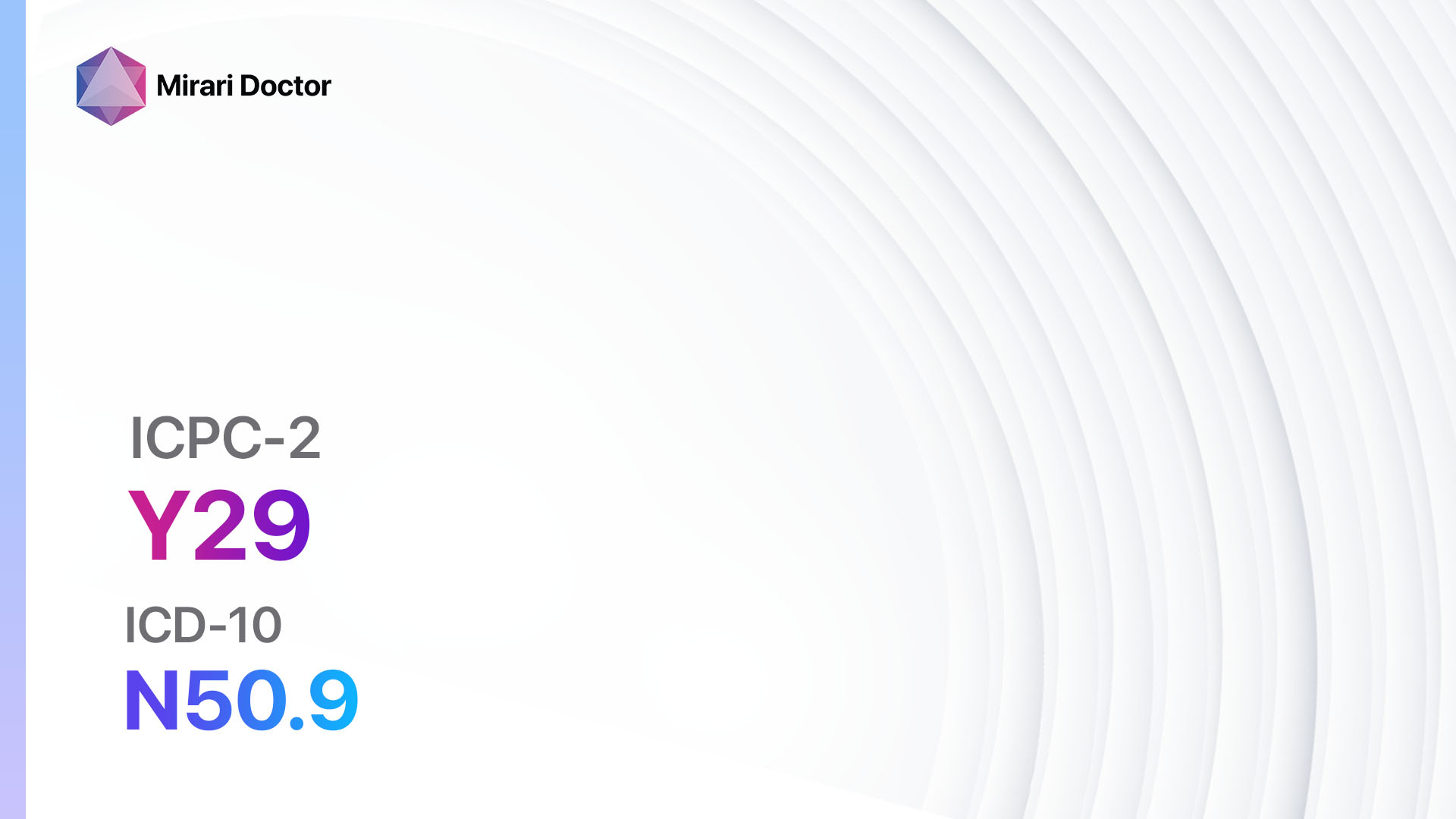
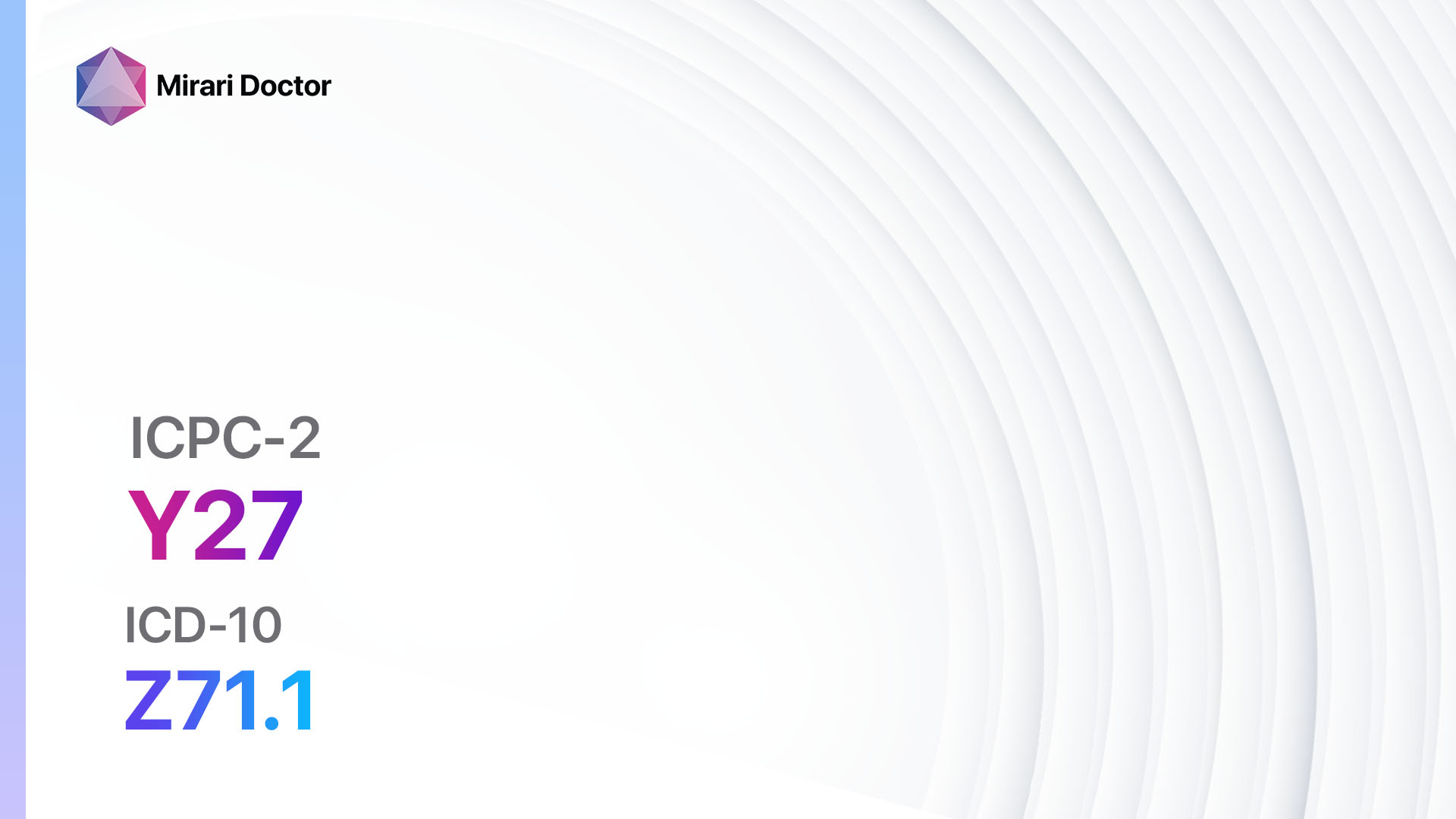
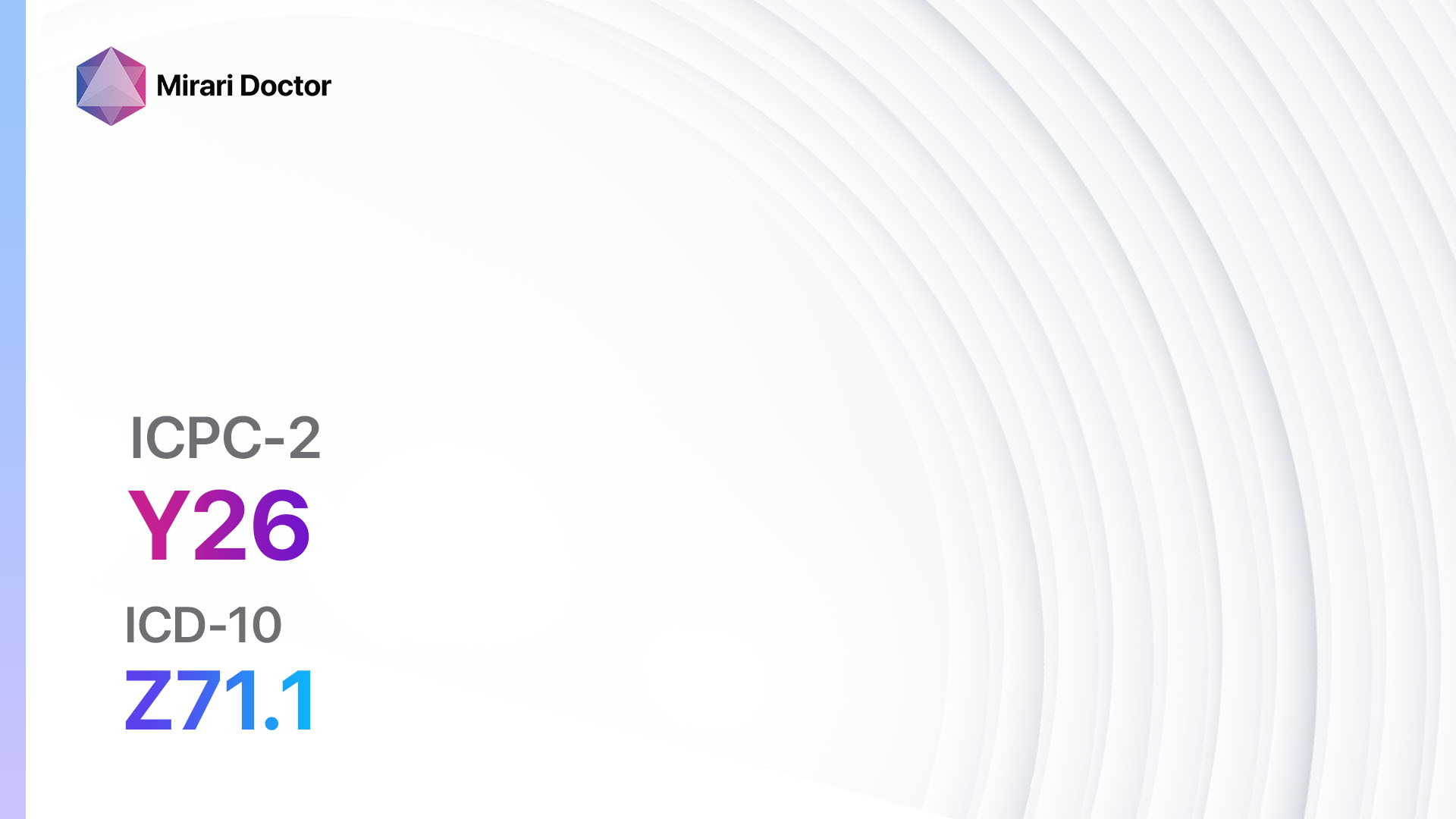
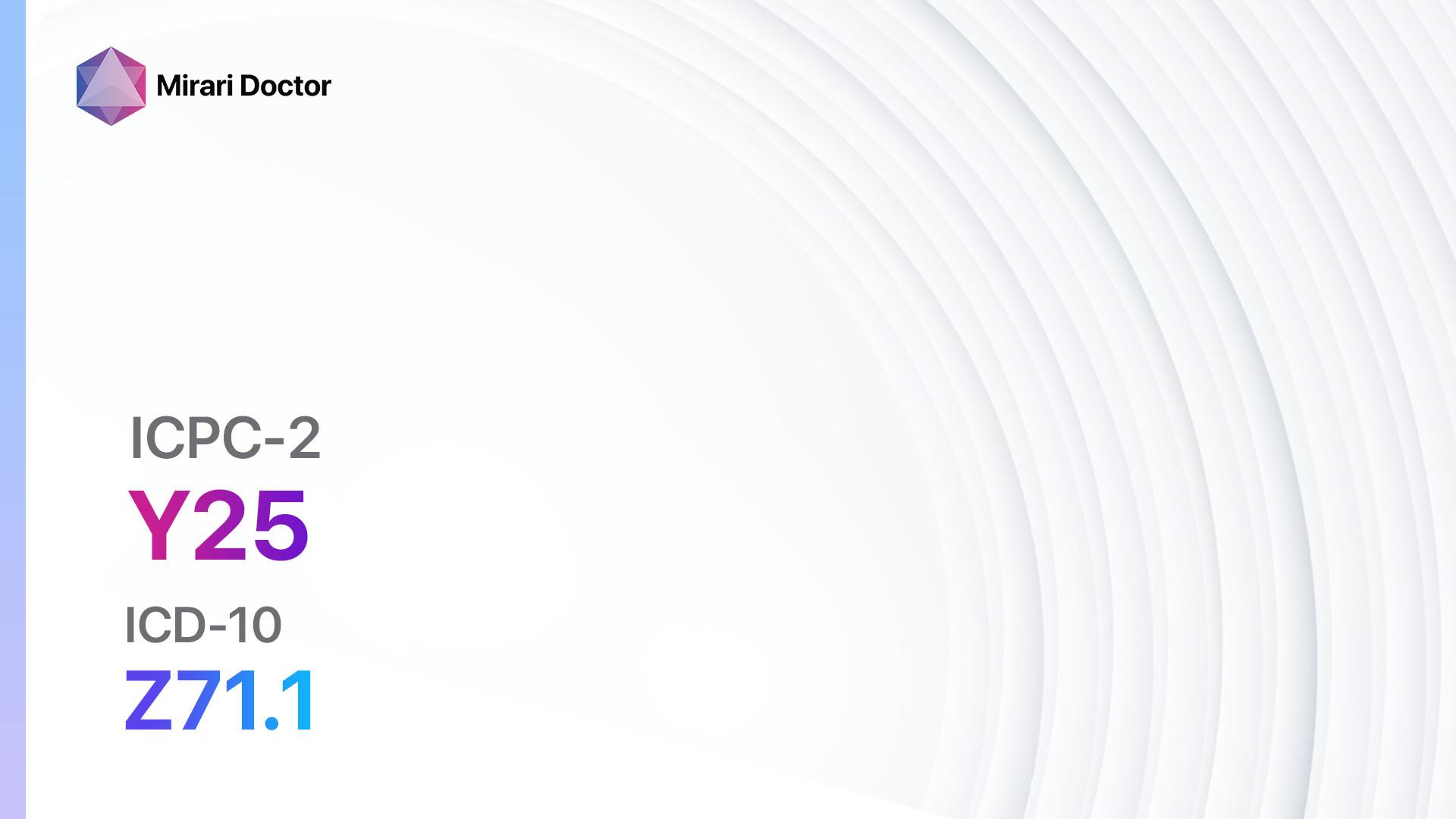
Codes
Symptoms
- Urethral discharge: Yellowish or white discharge from the penis[2]
- Painful or frequent urination: Discomfort or pain during urination, or an increased urge to urinate[3]
- Pain or swelling in the testicles: Inflammation or swelling of the testicles
- Anal symptoms: Rectal discharge, itching, or pain (in cases of receptive anal intercourse)[4]
- Sore throat: In cases of oral sex, the throat may become infected and show symptoms such as soreness or difficulty swallowing[5]
Causes
- Sexual contact: The primary mode of transmission is through sexual contact, including vaginal, anal, or oral sex.
- Unprotected sex: Engaging in sexual activity without using condoms increases the risk of contracting gonorrhoea[6].
- Multiple sexual partners: Having multiple sexual partners increases the likelihood of exposure to the infection.
Diagnostic Steps
Medical History
- Gather information about the patient’s sexual history, including recent sexual partners, and any high-risk sexual behaviors[7].
- Determine if the patient has a history of previous gonorrhoea infections or other sexually transmitted infections.
- Assess for any symptoms associated with gonorrhoea, such as discharge or pain during urination.
Physical Examination
- Inspect the genitals for any signs of inflammation, discharge, or ulcers.
- Palpate the testicles to check for swelling or tenderness.
- Examine the throat for any signs of infection or inflammation (in cases of oral sex)[8].
Laboratory Tests
- Nucleic acid amplification tests (NAATs): These tests are highly sensitive and specific for detecting gonorrhoea infections. They can be performed on urine samples, genital swabs, or rectal swabs[9].
- Gram stain: This test can be used to identify the presence of gonorrhoea bacteria in a urethral or genital swab.
- Culture: Culturing the bacteria in the lab can help confirm the diagnosis and determine antibiotic susceptibility[10].
Diagnostic Imaging
- No diagnostic imaging is typically required for the diagnosis of gonorrhoea in males.
Other Tests
- HIV and syphilis screening: It is recommended to screen for other sexually transmitted infections, such as HIV and syphilis, as they often coexist with gonorrhoea.
Follow-up and Patient Education
- Provide the patient with information about gonorrhoea, including the transmission, symptoms, and potential complications.
- Encourage the patient to inform their sexual partners and recommend that they get tested and treated as well.
- Schedule a follow-up visit to assess treatment response and ensure the infection has cleared.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Gonorrhoea:
- Ceftriaxone:
- Cost: $5-$15 per injection.
- Contraindications: Hypersensitivity to cephalosporins.
- Side effects: Diarrhea, nausea, rash.
- Severe side effects: Severe allergic reactions, anaphylaxis.
- Drug interactions: No significant drug interactions.
- Warning: Treatment failure has been reported, so close follow-up is necessary.
- Azithromycin:
- Cost: $10-$20 per course.
- Contraindications: Hypersensitivity to macrolides.
- Side effects: Diarrhea, nausea, abdominal pain.
- Severe side effects: Rare but possible severe allergic reactions.
- Drug interactions: No significant drug interactions.
- Warning: Treatment failure has been reported, so close follow-up is necessary.
- Doxycycline:
- Cost: $10-$20 per course.
- Contraindications: Hypersensitivity to tetracyclines, pregnancy, children under 8 years old.
- Side effects: Nausea, vomiting, photosensitivity.
- Severe side effects: Rare but possible severe allergic reactions, liver toxicity.
- Drug interactions: Avoid concomitant use with antacids, iron supplements, or dairy products.
- Warning: Treatment failure has been reported, so close follow-up is necessary.
- Ciprofloxacin:
- Cost: $10-$20 per course.
- Contraindications: Hypersensitivity to fluoroquinolones, children under 18 years old.
- Side effects: Nausea, diarrhea, headache.
- Severe side effects: Tendon rupture, severe allergic reactions.
- Drug interactions: Avoid concomitant use with certain medications, such as antacids or iron supplements.
- Warning: Increasing resistance to ciprofloxacin has been reported, so it should only be used in areas with low resistance rates.
- Gentamicin:
- Cost: $10-$20 per injection.
- Contraindications: Hypersensitivity to aminoglycosides.
- Side effects: Nausea, vomiting, dizziness.
- Severe side effects: Kidney damage, hearing loss.
- Drug interactions: No significant drug interactions.
- Warning: Close monitoring of kidney function and hearing is necessary.
Alternative Drugs:
- Gemifloxacin: A fluoroquinolone antibiotic that can be used as an alternative to ciprofloxacin.
- Spectinomycin: An injectable antibiotic that can be used as an alternative to ceftriaxone.
- Erythromycin: A macrolide antibiotic that can be used as an alternative to azithromycin.
Surgical Procedures:
- There are no surgical procedures indicated for the treatment of gonorrhoea in males.
Alternative Interventions
- Herbal remedies: Some herbal remedies, such as garlic and echinacea, may have antimicrobial properties. Cost: Varies depending on the specific herb or supplement.
- Probiotics: Probiotics may help restore the natural balance of bacteria in the body. Cost: $10-$40 per month.
- Pelvic floor exercises: These exercises can help manage symptoms of prostatitis and ease discomfort. Cost: No additional cost.
- Stress reduction techniques: Stress reduction techniques, such as meditation or yoga, may help improve overall well-being. Cost: Varies depending on the specific technique.
Lifestyle Interventions
- Abstinence: Avoiding sexual activity until the infection has cleared can prevent the spread of gonorrhoea. Cost: No additional cost.
- Safe sex practices: Using condoms consistently and correctly can reduce the risk of gonorrhoea transmission. Cost: Varies depending on the type and brand of condoms.
- Partner notification and treatment: Informing sexual partners about the infection and encouraging them to get tested and treated can prevent reinfection. Cost: No additional cost.
- Regular check-ups: Regular check-ups with a healthcare professional can help detect and treat gonorrhoea at an early stage. Cost: Varies depending on healthcare provider and insurance coverage.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – Y71 Gonorrhoea male (ICD-10:A54.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Gonorrhoea male effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Gonorrhoea male. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- World Health Organization. (2016). WHO guidelines for the treatment of Neisseria gonorrhoeae. Geneva: World Health Organization.
- Centers for Disease Control and Prevention. (2021). Gonorrhea – CDC Fact Sheet. Retrieved from https://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
- Bignell, C., & Unemo, M. (2013). 2012 European guideline on the diagnosis and treatment of gonorrhoea in adults. International Journal of STD & AIDS, 24(2), 85-92.
- Kent, C. K., Chaw, J. K., Wong, W., Liska, S., Gibson, S., Hubbard, G., & Klausner, J. D. (2005). Prevalence of rectal, urethral, and pharyngeal chlamydia and gonorrhea detected in 2 clinical settings among men who have sex with men: San Francisco, California, 2003. Clinical Infectious Diseases, 41(1), 67-74.
- Wiesner, P. J., Tronca, E., Bonin, P., Pedersen, A. H., & Holmes, K. K. (1973). Clinical spectrum of pharyngeal gonococcal infection. New England Journal of Medicine, 288(4), 181-185.
- Holmes, K. K., Levine, R., & Weaver, M. (2004). Effectiveness of condoms in preventing sexually transmitted infections. Bulletin of the World Health Organization, 82, 454-461.
- Workowski, K. A., & Bolan, G. A. (2015). Sexually transmitted diseases treatment guidelines, 2015. MMWR Recommendations and Reports, 64(RR-03), 1-137.
- Unemo, M., & Shafer, W. M. (2014). Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: past, evolution, and future. Clinical Microbiology Reviews, 27(3), 587-613.
- Cook, R. L., Hutchison, S. L., Østergaard, L., Braithwaite, R. S., & Ness, R. B. (2005). Systematic review: noninvasive testing for Chlamydia trachomatis and Neisseria gonorrhoeae. Annals of Internal Medicine, 142(11), 914-925.
- Unemo, M., & Shafer, W. M. (2011). Antibiotic resistance in Neisseria gonorrhoeae: origin, evolution, and lessons learned for the future. Annals of the New York Academy of Sciences, 1230(1), E19-E28.
Related articles
Made in USA