Introduction
Family planning is a crucial aspect of reproductive health for individuals and couples. It involves making informed decisions about when to have children, how many children to have, and the use of contraceptive methods to prevent unintended pregnancies[1]. Family planning for males includes various options for contraception that are safe and effective. This guide aims to provide information on the symptoms, causes, diagnostic steps, possible interventions, and follow-up for family planning male other (ICPC-2: Y14).
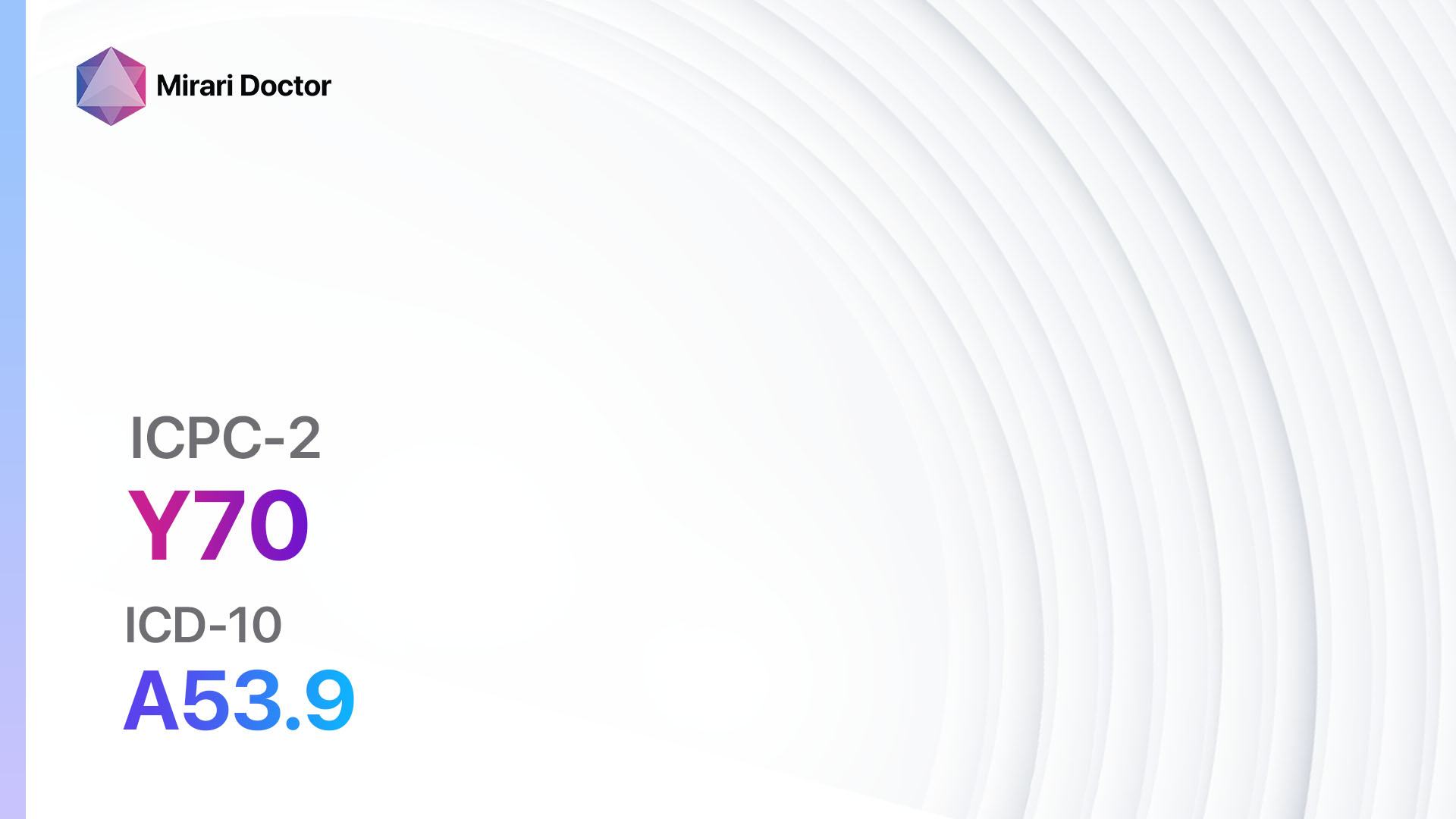
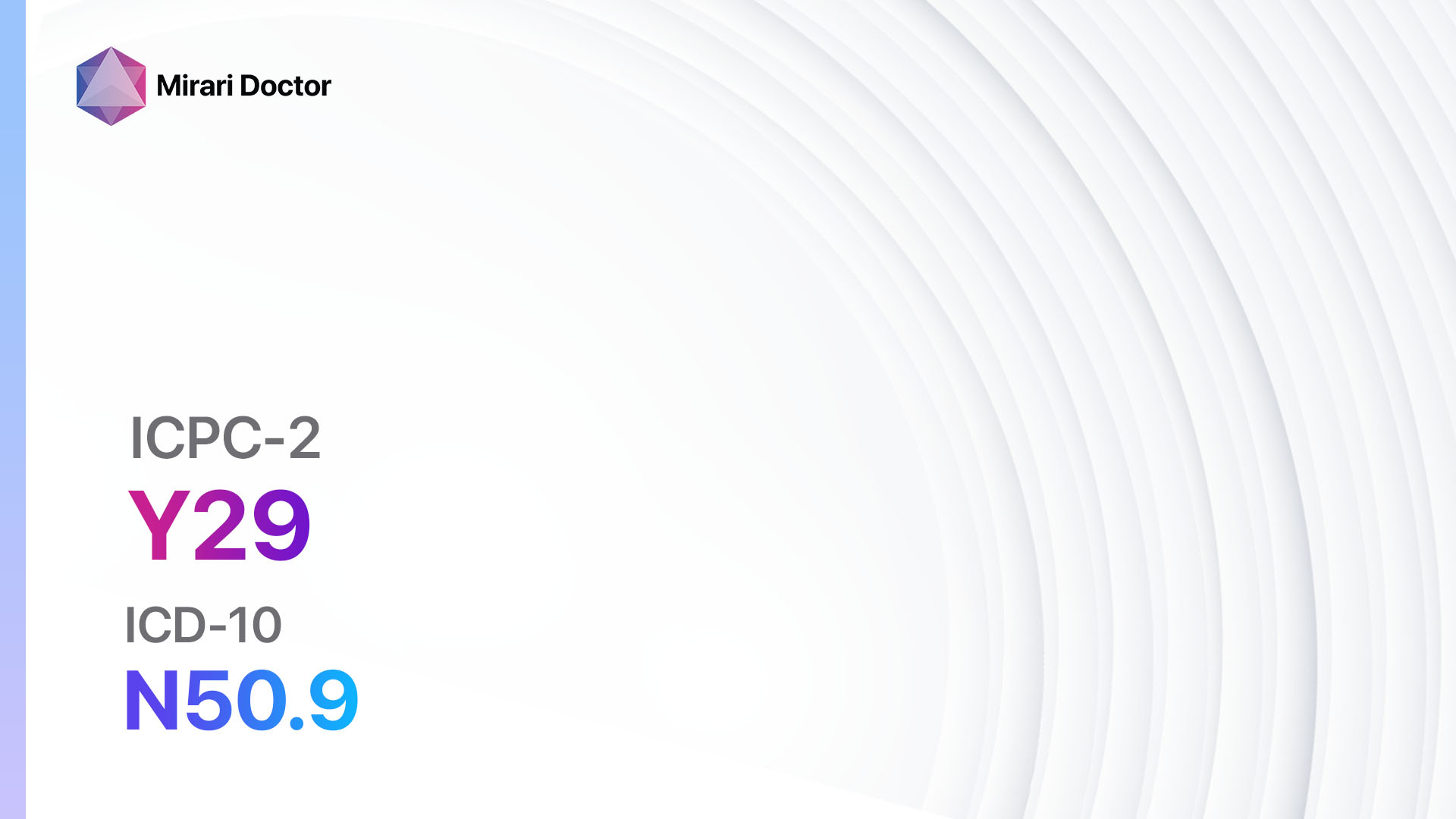
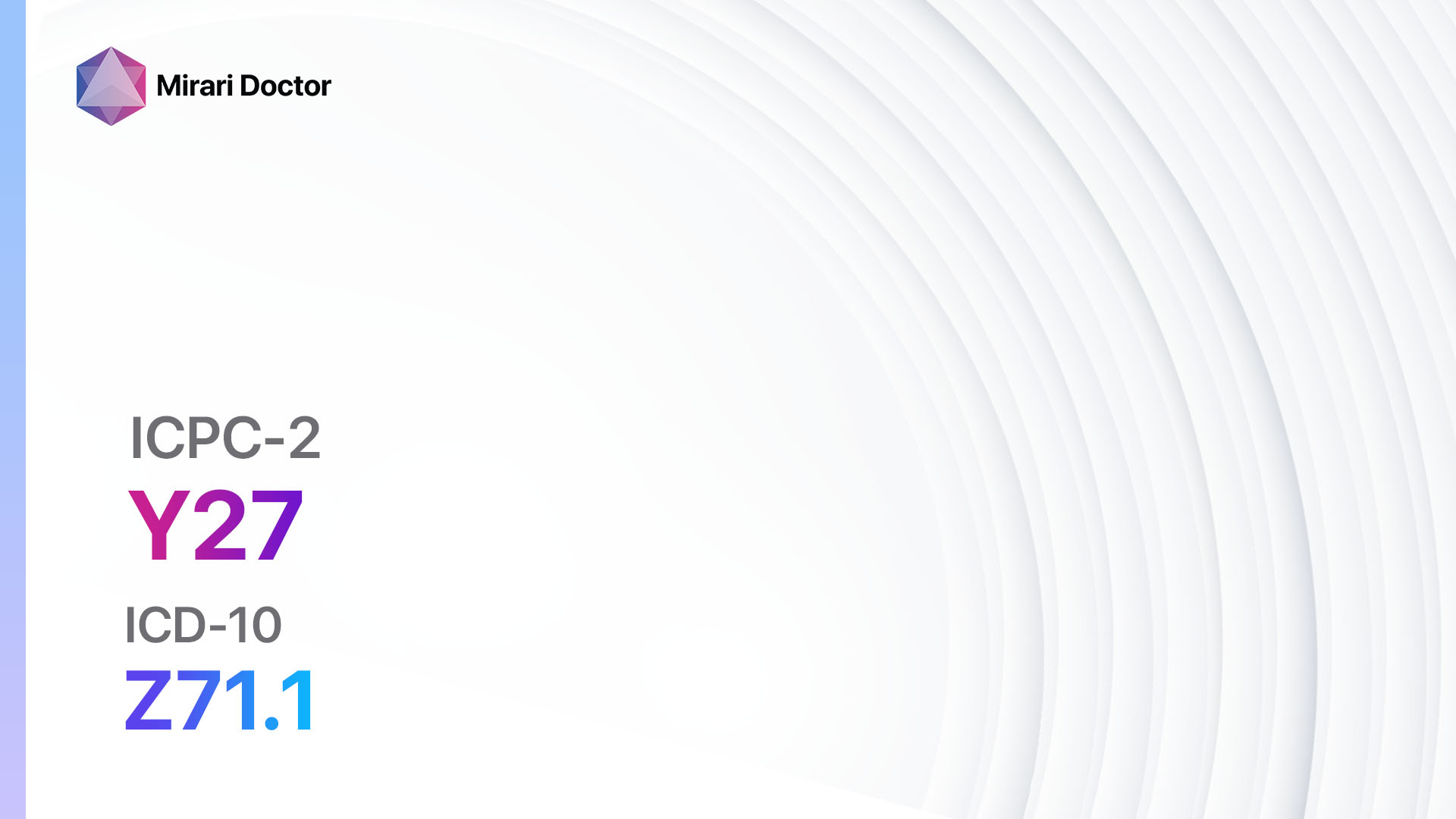
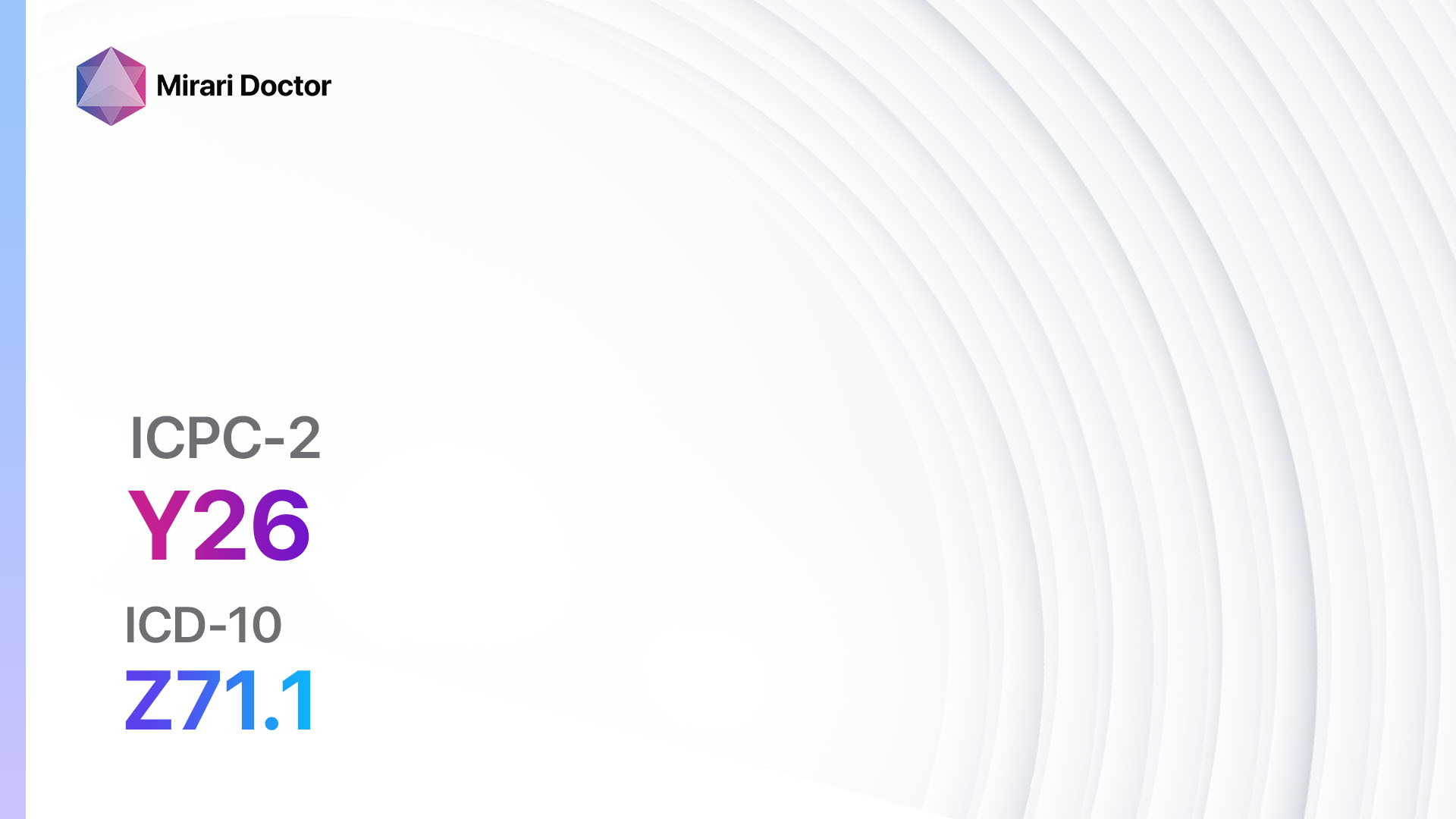
Codes
Symptoms
- Low libido: Decreased sexual desire or interest.
- Erectile dysfunction: Difficulty in achieving or maintaining an erection.
- Pain during sexual intercourse: Discomfort or pain experienced during sexual activity.
- Abnormal ejaculation: Changes in the volume, consistency, or timing of ejaculation[4].
It is important to note that the symptoms mentioned above may not be specific to family planning male other (ICPC-2: Y14) and can be associated with other medical conditions. It is necessary to consult a healthcare professional for a proper diagnosis.
Causes
- Hormonal imbalance: Fluctuations in testosterone levels can affect sexual desire and function.
- Psychological factors: Stress, anxiety, depression, or relationship issues can contribute to sexual problems.
- Medications: Certain medications, such as antidepressants or blood pressure medications, can have side effects that affect sexual function.
- Chronic medical conditions: Conditions like diabetes, heart disease, or neurological disorders can impact sexual health[5].
Diagnostic Steps
Medical History
- Gather information about the patient’s sexual history, including any previous pregnancies or children.
- Assess the patient’s current sexual function and any symptoms related to family planning male other (ICPC-2: Y14).
- Inquire about any underlying medical conditions, medications, or psychological factors that may contribute to the symptoms[6].
Physical Examination
- Perform a comprehensive physical examination, including a genital examination, to assess for any abnormalities or signs of underlying medical conditions.
- Check blood pressure and assess overall cardiovascular health.
- Evaluate the patient’s overall health status and identify any potential risk factors for family planning male other (ICPC-2: Y14)[7].
Laboratory Tests
- Hormone levels: Testosterone, luteinizing hormone (LH), follicle-stimulating hormone (FSH).
- Blood tests: Complete blood count (CBC), lipid profile, blood glucose levels.
- Urinalysis: To rule out urinary tract infections or other urinary abnormalities.
- Sexually transmitted infection (STI) screening: Depending on risk factors and sexual history[8].
Diagnostic Imaging
- Ultrasound: Can be used to evaluate the testicles, prostate, or other structures related to sexual function.
- Magnetic resonance imaging (MRI): In certain cases, an MRI may be necessary to assess specific conditions or abnormalities[9].
Other Tests
- Semen analysis: If fertility is a concern, a semen analysis can evaluate sperm count, motility, and morphology.
- Psychological assessment: In some cases, a psychological evaluation may be helpful in identifying any underlying psychological factors contributing to sexual problems[10].
Follow-up and Patient Education
- Provide appropriate counseling and education to the patient regarding family planning options for males.
- Discuss the potential benefits and risks of various contraceptive methods.
- Emphasize the importance of regular follow-up visits to monitor the effectiveness of chosen interventions and address any concerns or side effects.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for family planning male other (ICPC-2: Y14):
- Condoms:
- Cost: Varies depending on the brand and quantity, ranging from $0.50 to $2 per condom.
- Contraindications: Allergy to latex or polyurethane.
- Side effects: Latex allergies may cause skin irritation or allergic reactions.
- Severe side effects: Rare, but possible allergic reactions.
- Drug interactions: None.
- Warning: Proper use is essential for effectiveness in preventing pregnancy and STIs.
- Vasectomy:
- Cost: The cost of a vasectomy procedure can range from $500 to $3,000.
- Contraindications: None, but it is considered a permanent form of contraception.
- Side effects: Temporary discomfort, swelling, or bruising after the procedure.
- Severe side effects: Rare, but possible infection or bleeding.
- Drug interactions: None.
- Warning: The procedure should be considered irreversible, and alternative options should be explored if future fertility is desired.
- Withdrawal method:
- Cost: Free.
- Contraindications: Requires trust, communication, and self-control.
- Side effects: None.
- Severe side effects: High risk of pregnancy if not used correctly.
- Drug interactions: None.
- Warning: Not considered a reliable method of contraception due to the risk of pre-ejaculate containing sperm.
- Spermicides:
- Cost: Varies depending on the brand and quantity, ranging from $5 to $15 for a pack of 12.
- Contraindications: Allergy to spermicide ingredients.
- Side effects: Possible genital irritation or allergic reactions.
- Severe side effects: Rare, but possible allergic reactions.
- Drug interactions: None.
- Warning: Should be used in combination with other barrier methods for optimal effectiveness.
- Hormonal methods (e.g., contraceptive pills, patches, injections):
- Cost: Varies depending on the specific method and insurance coverage, ranging from $0 to $50 per month.
- Contraindications: History of blood clots, certain cancers, liver disease, or uncontrolled high blood pressure.
- Side effects: Possible hormonal side effects such as mood changes, breast tenderness, or irregular bleeding.
- Severe side effects: Rare, but possible blood clots, stroke, or heart attack.
- Drug interactions: Certain medications may reduce the effectiveness of hormonal contraceptives.
- Warning: Requires consistent and correct use for optimal effectiveness in preventing pregnancy.
Alternative Drugs:
- Intrauterine devices (IUDs): While not directly applicable to males, IUDs can be a reliable form of contraception for couples.
- Emergency contraception: Options such as levonorgestrel or ulipristal acetate can be used in case of contraceptive failure or unprotected intercourse.
Surgical Procedures:
- Vasectomy reversal: In cases where future fertility is desired, a vasectomy reversal procedure can be performed to reconnect the vas deferens. Cost: The cost of vasectomy reversal can range from $3,000 to $15,000.
- Testicular sperm extraction (TESE): In cases of male infertility, TESE can be performed to retrieve sperm directly from the testicles for use in assisted reproductive techniques. Cost: The cost of TESE can range from $2,000 to $10,000.
Alternative Interventions
- Natural family planning: Methods such as tracking menstrual cycles, monitoring basal body temperature, or observing cervical mucus changes can be used to identify fertile and infertile periods. Cost: Free.
- Male contraceptive research: Ongoing research is being conducted on male contraceptive options, including hormonal methods, non-hormonal methods, and injections. Cost: Varies depending on the research study or clinical trial participation.
Lifestyle Interventions
- Healthy lifestyle: Encourage the adoption of a healthy diet, regular exercise, stress management techniques, and adequate sleep, as these factors can positively impact sexual health. Cost: Varies depending on personal choices.
- Avoidance of tobacco and excessive alcohol: Smoking and excessive alcohol consumption can negatively affect sexual function. Cost: Varies depending on personal choices.
- Open communication and relationship counseling: Addressing any relationship issues or communication barriers can help improve sexual satisfaction. Cost: Varies depending on the counseling or therapy options chosen.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
By following the diagnostic steps and considering the possible interventions mentioned in this guide, healthcare professionals can provide appropriate care and guidance to individuals seeking family planning options for males.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – Y14 Family planning male other (ICD-10:Z30.8)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: Localized Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: Localized Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: Localized Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 4 (Diabetes) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 4 (Diabetes) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 4 (Diabetes) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 5 (Prostatitis) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 5 (Prostatitis) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 5 (Prostatitis) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Family planning male other effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Family planning male other. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- World Health Organization. Family planning/Contraception methods. Available at: https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception
- World Organization of Family Doctors (WONCA). International Classification of Primary Care, Second edition (ICPC-2). Oxford University Press, 1998.
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Geneva: WHO, 2019.
- McCabe MP, Sharlip ID, Lewis R, et al. Incidence and prevalence of sexual dysfunction in women and men: a consensus statement from the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016;13(2):144-152.
- Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013;381(9861):153-165.
- Hatzimouratidis K, Giuliano F, Moncada I, et al. EAU guidelines on erectile dysfunction, premature ejaculation, penile curvature and priapism. Eur Urol. 2016;70(2):e1-e17.
- Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536-2559.
- Burnett AL, Nehra A, Breau RH, et al. Erectile Dysfunction: AUA Guideline. J Urol. 2018;200(3):633-641.
- Cokkinos DD, Antypa E, Tserotas P, et al. Emergency ultrasound of the scrotum: A review of the commonest pathologic conditions. Curr Probl Diagn Radiol. 2011;40(1):1-14.
- Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822-830.
Related articles
Made in USA