Introduction
Pain face, also known as facial pain, is a condition characterized by discomfort or pain in the face. It can be caused by various factors and may vary in severity and duration. This guide aims to provide an overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle interventions for pain face.
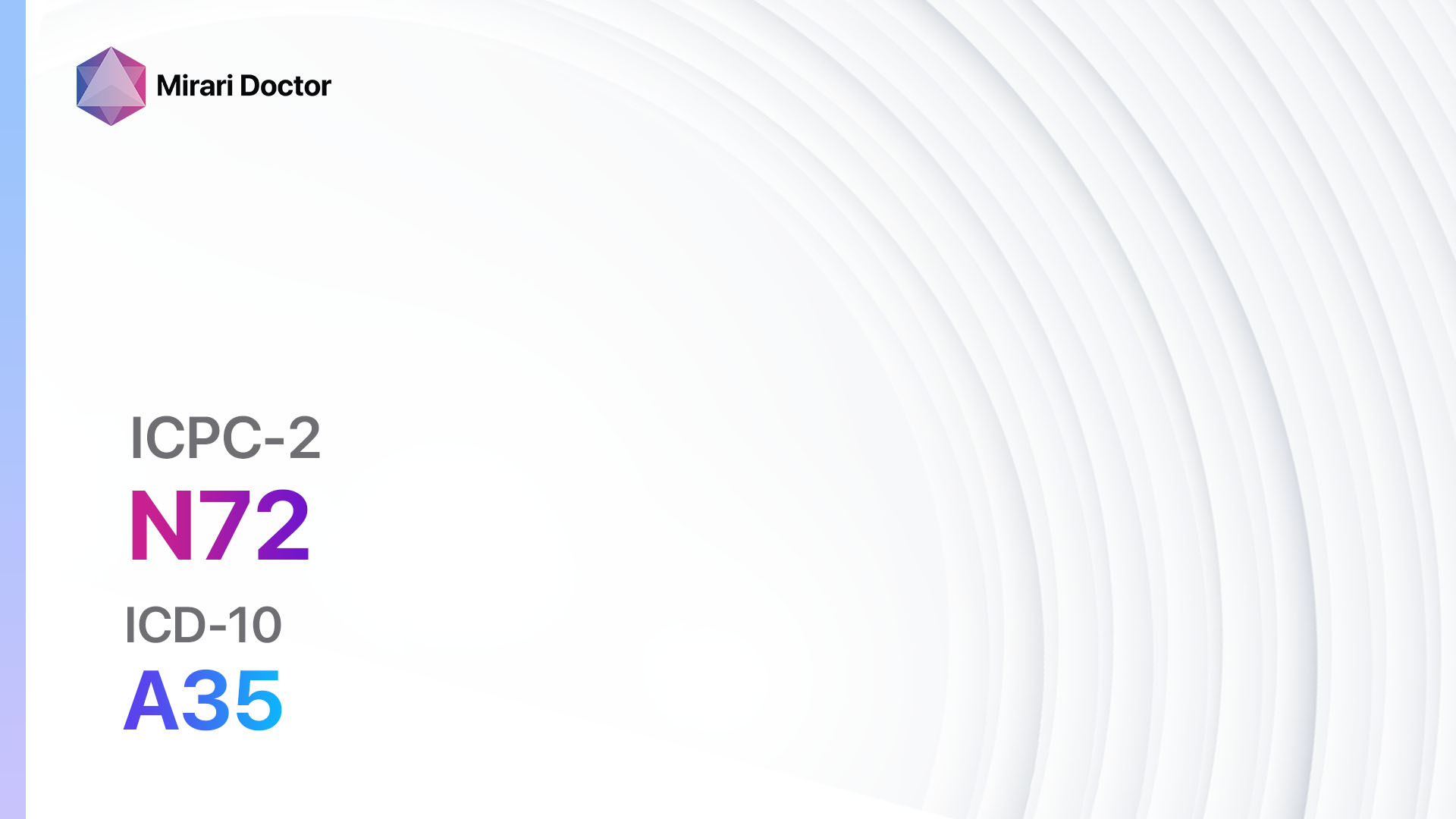
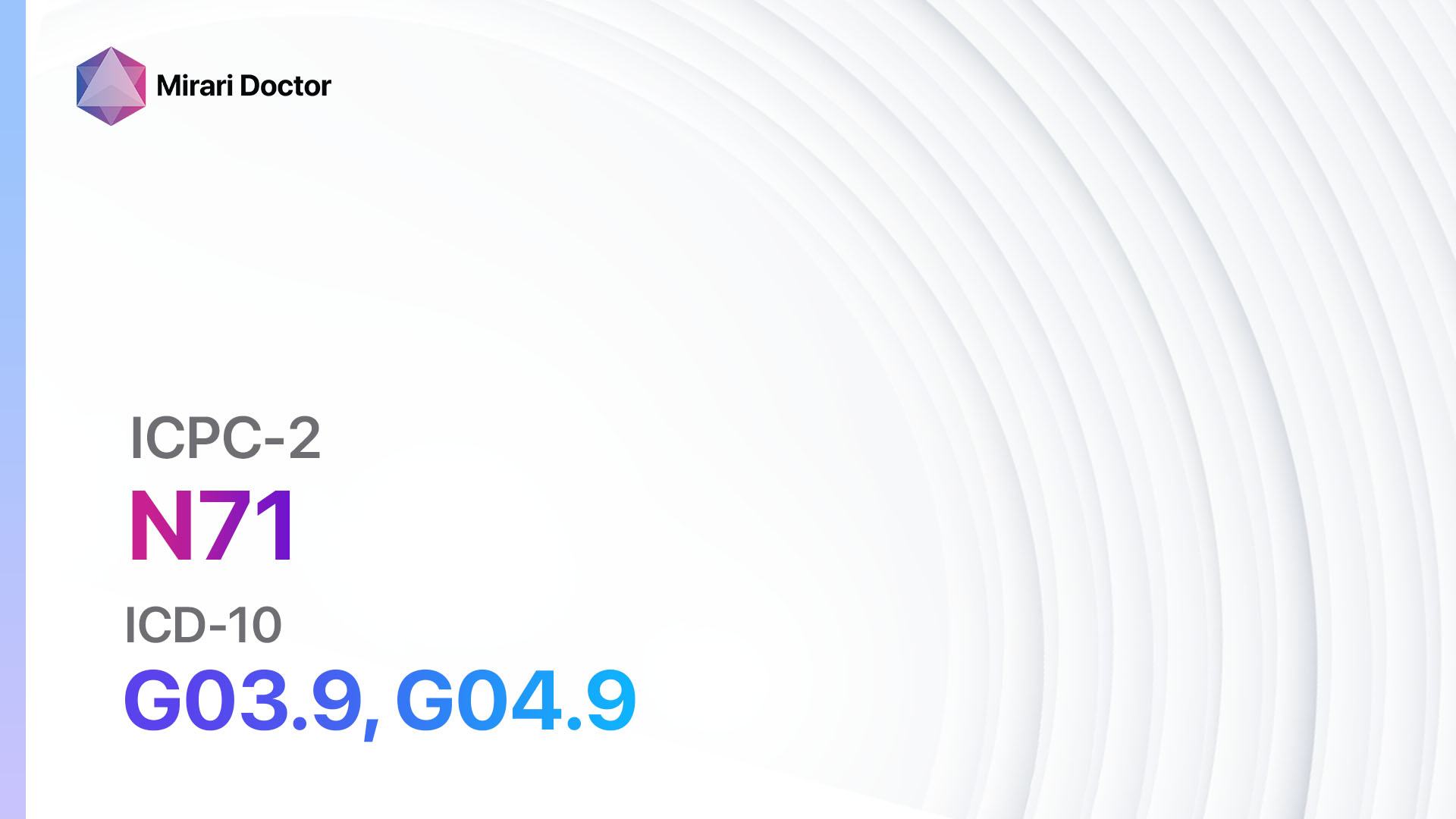
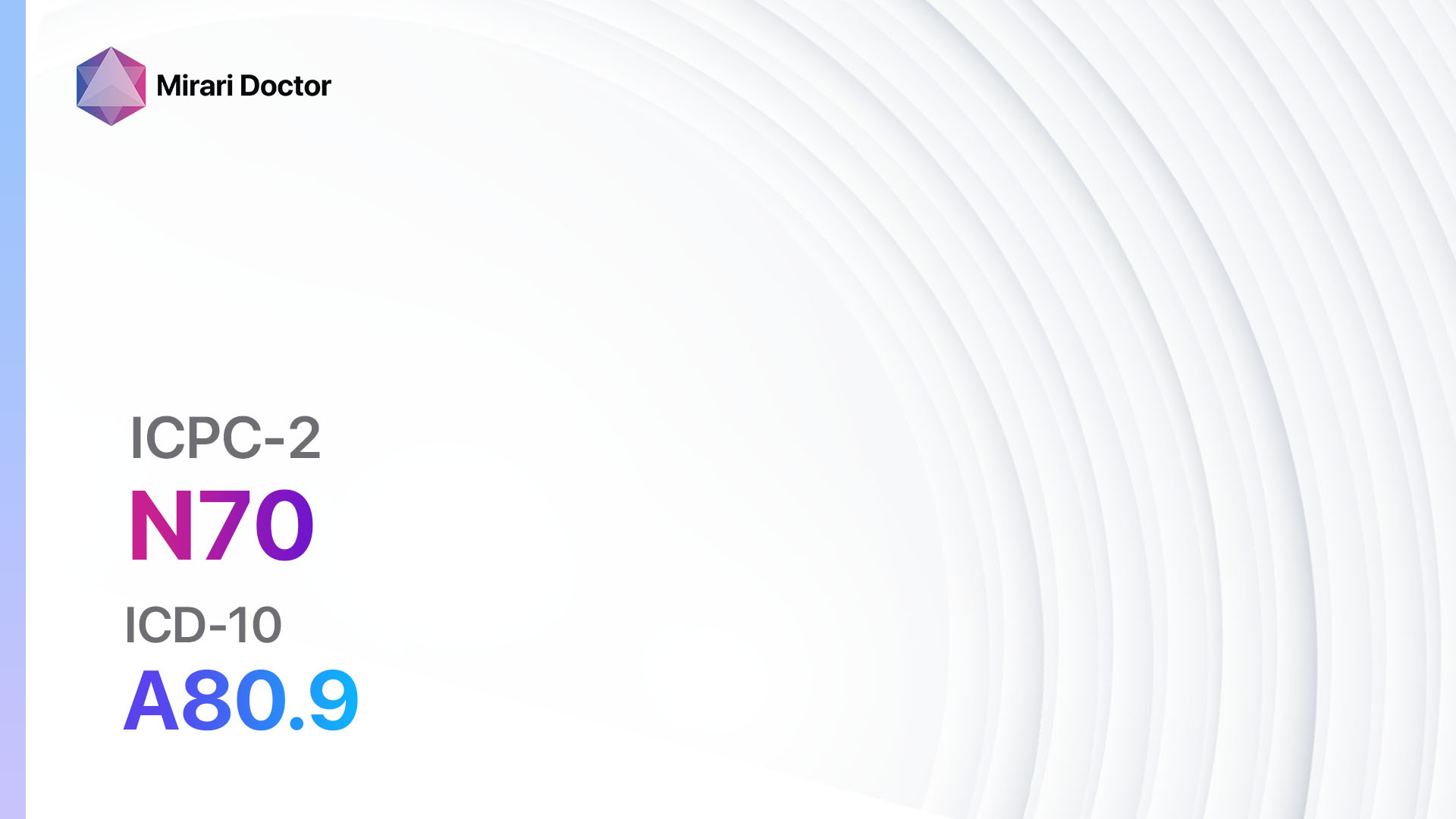
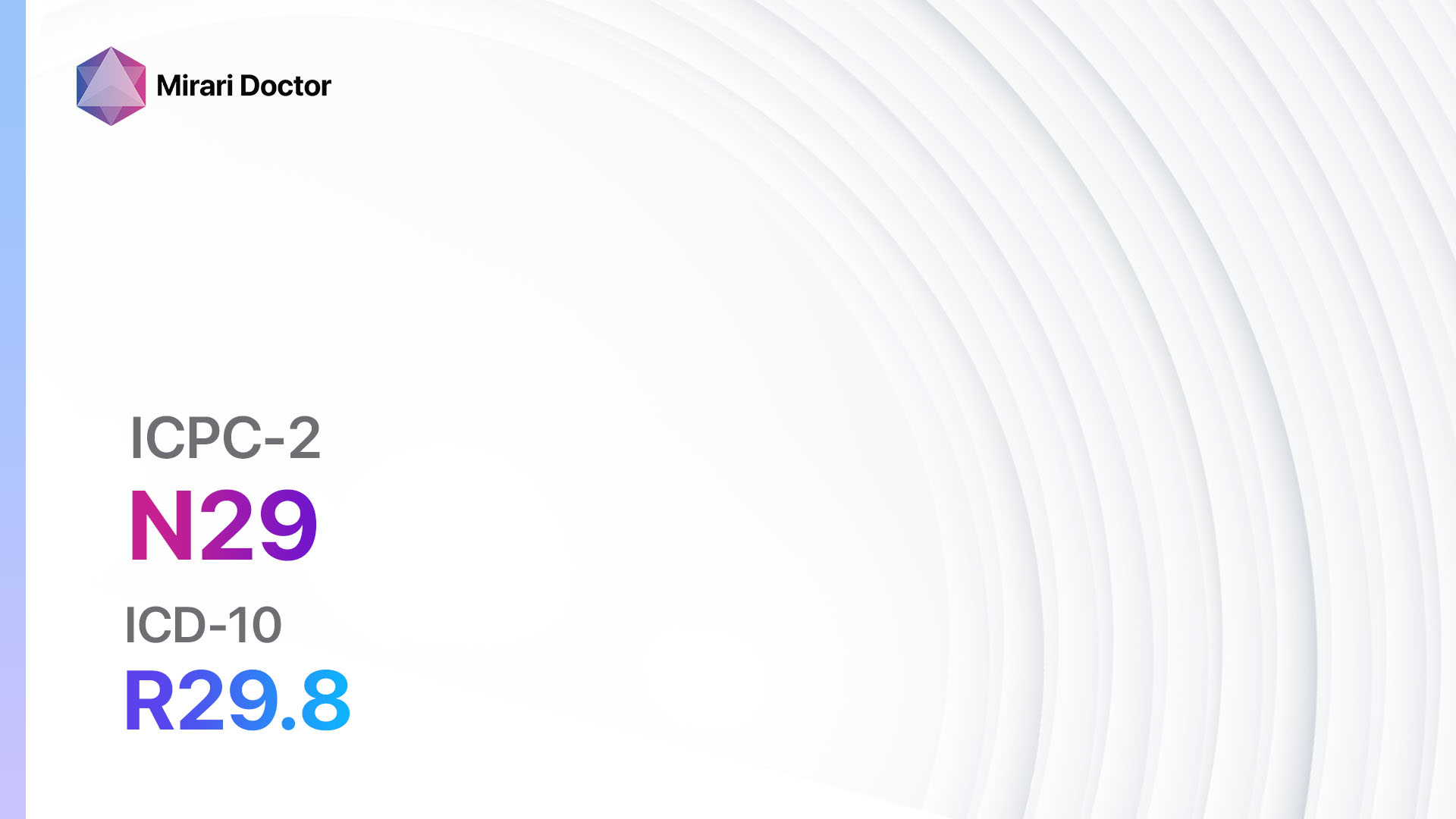
Codes
Symptoms
- Facial pain: Dull, aching, or sharp pain in the face.
- Facial tenderness: Sensitivity or tenderness in the facial muscles or skin.
- Headache: Pain that radiates from the face to the head.
- Jaw pain: Discomfort or pain in the jaw area.
- Toothache: Pain or sensitivity in the teeth.
- Earache: Pain or discomfort in the ears.
- Facial swelling: Swelling or inflammation in the face.
- Difficulty chewing or speaking: Pain or discomfort that affects the ability to chew food or speak properly.[1][2]
Causes
- Dental problems: Tooth decay, gum disease, or dental infections can cause facial pain.
- Sinusitis: Inflammation or infection of the sinuses can lead to facial pain.
- Temporomandibular joint disorder (TMJ): Dysfunction or inflammation of the jaw joint can cause facial pain.
- Trigeminal neuralgia: A chronic condition characterized by severe facial pain due to irritation or damage to the trigeminal nerve.
- Cluster headaches: Intense headaches that occur in clusters and cause severe facial pain.
- Migraines: Severe headaches that can cause facial pain and other symptoms.
- Facial trauma: Injuries to the face, such as fractures or contusions, can result in facial pain.
- Infections: Viral or bacterial infections, such as herpes zoster or sinus infections, can cause facial pain.
- Nerve damage: Damage to the facial nerves can lead to chronic facial pain.[3][4]
Diagnostic Steps
Medical History
- Obtain a detailed medical history, including any previous facial trauma, dental problems, or history of sinusitis.
- Ask about the location, duration, and severity of the facial pain.
- Inquire about any associated symptoms, such as headaches, jaw pain, or toothache.
- Assess for any risk factors, such as a history of migraines or trigeminal neuralgia.[5]
Physical Examination
- Perform a thorough physical examination of the face, jaw, and teeth.
- Palpate the facial muscles and assess for tenderness or swelling.
- Examine the teeth and gums for signs of decay, infection, or gum disease.
- Evaluate the temporomandibular joint for any signs of dysfunction or inflammation.
- Check for any abnormalities or deformities in the facial bones.[6]
Laboratory Tests
- Complete blood count (CBC): To rule out any underlying infections or systemic conditions.
- Erythrocyte sedimentation rate (ESR): To assess for inflammation in the body.
- C-reactive protein (CRP): Another marker of inflammation that can help identify the cause of facial pain.
- Viral and bacterial cultures: If an infection is suspected, cultures can help identify the causative organism.[7]
Diagnostic Imaging
- X-rays: Can help identify any dental or jaw abnormalities, such as fractures or impacted teeth.
- CT scan: Provides detailed images of the facial bones, sinuses, and temporomandibular joint.
- MRI: Useful for evaluating soft tissues, nerves, and blood vessels in the face and head.[8]
Other Tests
- Dental examination: A thorough examination by a dentist can help identify any dental causes of facial pain.
- Neurological examination: If nerve damage or trigeminal neuralgia is suspected, a neurological examination may be necessary.
- Sinus endoscopy: A procedure to visualize the sinuses and assess for any abnormalities or signs of infection.[9]
Follow-up and Patient Education
- Schedule a follow-up appointment to discuss the results of the diagnostic tests and determine the appropriate treatment plan.
- Provide education to the patient about the condition, its causes, and possible treatment options.
- Emphasize the importance of good oral hygiene and regular dental check-ups to prevent dental causes of facial pain.[10]
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for facial pain:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., Ibuprofen, Naproxen):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: History of gastrointestinal bleeding, renal impairment.
- Side effects: Upset stomach, heartburn, dizziness.
- Severe side effects: Gastrointestinal bleeding, kidney damage.
- Drug interactions: Aspirin, other NSAIDs, blood thinners.
- Warning: Prolonged use can increase the risk of cardiovascular events.
- Anticonvulsants (e.g., Gabapentin, Carbamazepine):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Drowsiness, dizziness, nausea.
- Severe side effects: Stevens-Johnson syndrome, liver toxicity.
- Drug interactions: Oral contraceptives, antacids.
- Warning: May cause drowsiness, avoid driving or operating machinery.
- Muscle relaxants (e.g., Cyclobenzaprine, Baclofen):
- Cost: Generic versions can be $10-$30/month.
- Contraindications: Hypersensitivity to the medication, history of liver disease.
- Side effects: Drowsiness, dry mouth, dizziness.
- Severe side effects: Seizures, hallucinations.
- Drug interactions: Alcohol, opioids.
- Warning: May cause drowsiness, avoid driving or operating machinery.
- Tricyclic antidepressants (e.g., Amitriptyline, Nortriptyline):
- Cost: Generic versions can be $10-$30/month.
- Contraindications: Recent myocardial infarction, glaucoma.
- Side effects: Dry mouth, constipation, drowsiness.
- Severe side effects: Cardiac arrhythmias, serotonin syndrome.
- Drug interactions: Monoamine oxidase inhibitors (MAOIs), antihistamines.
- Warning: May cause drowsiness, avoid driving or operating machinery.
- Opioids (e.g., Codeine, Oxycodone):
- Cost: Generic versions can range from $10-$100/month.
- Contraindications: Respiratory depression, history of substance abuse.
- Side effects: Constipation, drowsiness, nausea.
- Severe side effects: Respiratory depression, addiction.
- Drug interactions: Benzodiazepines, alcohol.
- Warning: High risk of addiction and dependence, use with caution.
Alternative Drugs:
- Topical analgesics (e.g., Lidocaine patches): Can provide localized pain relief. Cost: $10-$50 per patch.
- Antidepressants (e.g., Duloxetine, Venlafaxine): May help with chronic pain management. Cost: $10-$50/month.
- Botox injections: Can be used for specific types of facial pain, such as trigeminal neuralgia. Cost: $300-$600 per injection.
- Steroids: Can be used for short-term pain relief in certain cases. Cost: Varies depending on the specific steroid and route of administration.
- Antiviral medications: If a viral infection is suspected, antiviral medications may be prescribed. Cost: Varies depending on the specific medication.
Surgical Procedures:
- Microvascular decompression: A surgical procedure to relieve pressure on the trigeminal nerve. Cost: $10,000-$30,000.
- Rhizotomy: A procedure to selectively destroy nerve fibers to alleviate pain. Cost: $5,000-$15,000.
- Nerve blocks: Injection of anesthetic medication to block pain signals. Cost: $500-$1,500 per injection.
- Radiofrequency ablation: A minimally invasive procedure that uses heat to destroy nerve fibers. Cost: $2,000-$5,000.
- Neurostimulation: Implantation of a device that delivers electrical impulses to block pain signals. Cost: $20,000-$50,000.
Alternative Interventions
- Acupuncture: May help relieve facial pain by stimulating specific points on the body. Cost: $60-$120 per session.
- Chiropractic care: Manipulation of the spine and joints to alleviate pain. Cost: $50-$200 per session.
- Herbal supplements: Some herbs, such as turmeric or ginger, may have anti-inflammatory properties. Cost: Varies depending on the specific supplement.
- Mind-body techniques: Practices like meditation, yoga, or relaxation exercises can help manage pain. Cost: Varies depending on the specific program or class.
- Physical therapy: Exercises and techniques to improve muscle strength and flexibility. Cost: $50-$150 per session.
Lifestyle Interventions
- Stress management: Learning stress reduction techniques, such as deep breathing or mindfulness, can help manage facial pain. Cost: Varies depending on the specific program or class.
- Heat or cold therapy: Applying heat or cold packs to the face can provide temporary pain relief. Cost: $10-$30 for heat or cold packs.
- Dietary modifications: Avoiding trigger foods, such as caffeine or alcohol, may help reduce facial pain. Cost: Varies depending on individual food choices.
- Good oral hygiene: Regular brushing, flossing, and dental check-ups can prevent dental causes of facial pain. Cost: Varies depending on dental insurance coverage.
- Sleep hygiene: Establishing a regular sleep routine and creating a comfortable sleep environment can help manage facial pain. Cost: Varies depending on individual sleep needs.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. It is recommended to consult with a healthcare professional for personalized treatment options and cost estimates.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – N03 Pain face (ICD-10:R51)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 7 (Neuro system & ENT) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 7 (Neuro system & ENT) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Pain face effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Pain face. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Zakrzewska JM. Differential diagnosis of facial pain and guidelines for management. Br J Anaesth. 2013;111(1):95-104.
- Romero-Reyes M, Uyanik JM. Orofacial pain management: current perspectives. J Pain Res. 2014;7:99-115.
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211.
- Benoliel R, Eliav E, Sharav Y. Classification of chronic orofacial pain: applicability of chronic headache criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(6):729-737.
- Aggarwal VR, McBeth J, Zakrzewska JM, Lunt M, Macfarlane GJ. The epidemiology of chronic syndromes that are frequently unexplained: do they have common associated factors? Int J Epidemiol. 2006;35(2):468-476.
- Okeson JP. Bell’s Oral and Facial Pain. 7th ed. Chicago, IL: Quintessence Publishing; 2014.
- Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008;359(25):2693-2705.
- Cruccu G, Finnerup NB, Jensen TS, et al. Trigeminal neuralgia: New classification and diagnostic grading for practice and research. Neurology. 2016;87(2):220-228.
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 Suppl):S1-S39.
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28(1):6-27.
Related articles
Made in USA