Introduction
Gastroenteritis is a common condition characterized by inflammation of the gastrointestinal tract. It is typically caused by a viral or bacterial infection and can lead to symptoms such as diarrhea, vomiting, and abdominal pain[1]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnostic steps and possible interventions for gastroenteritis presumed infection.
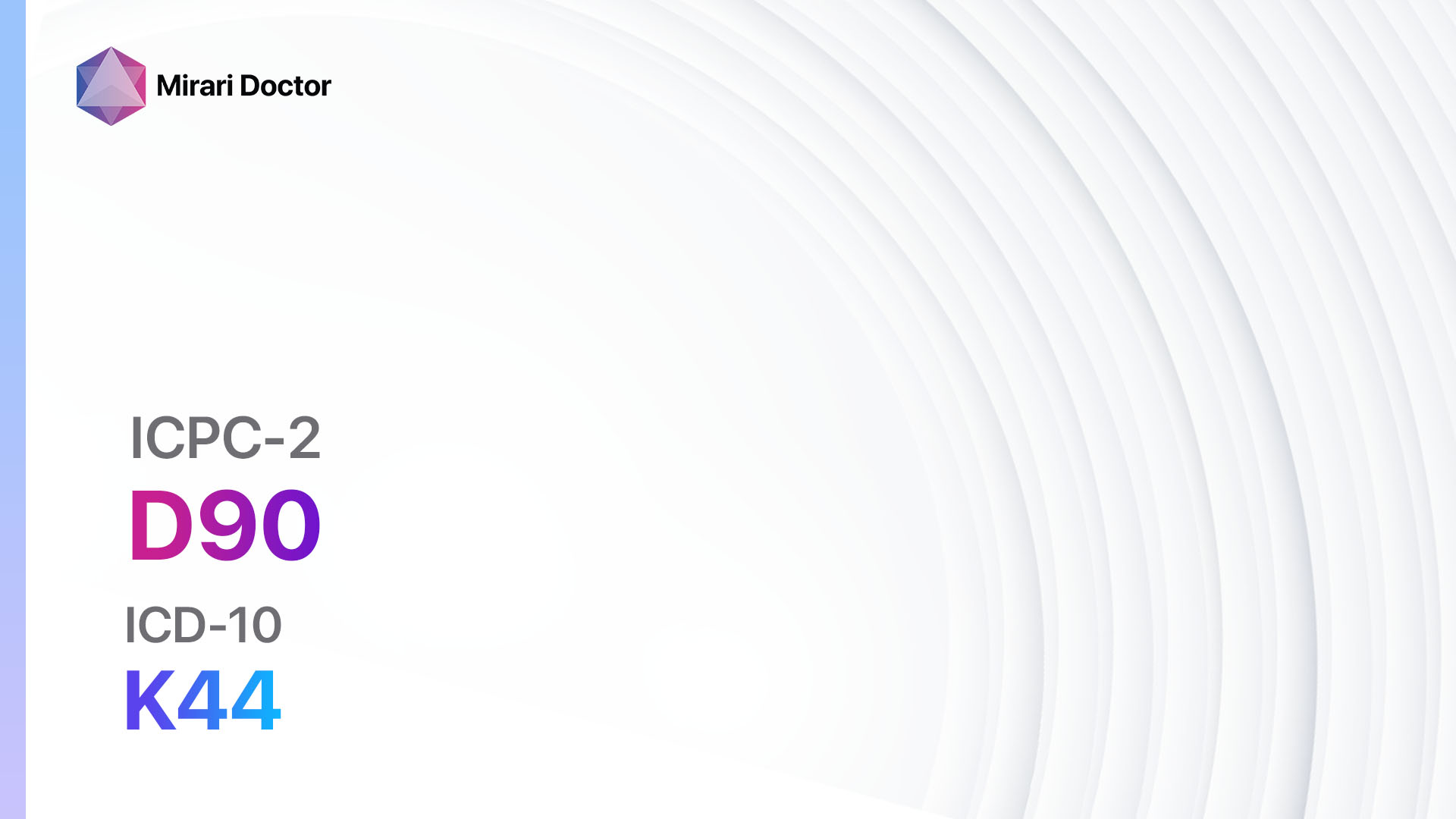
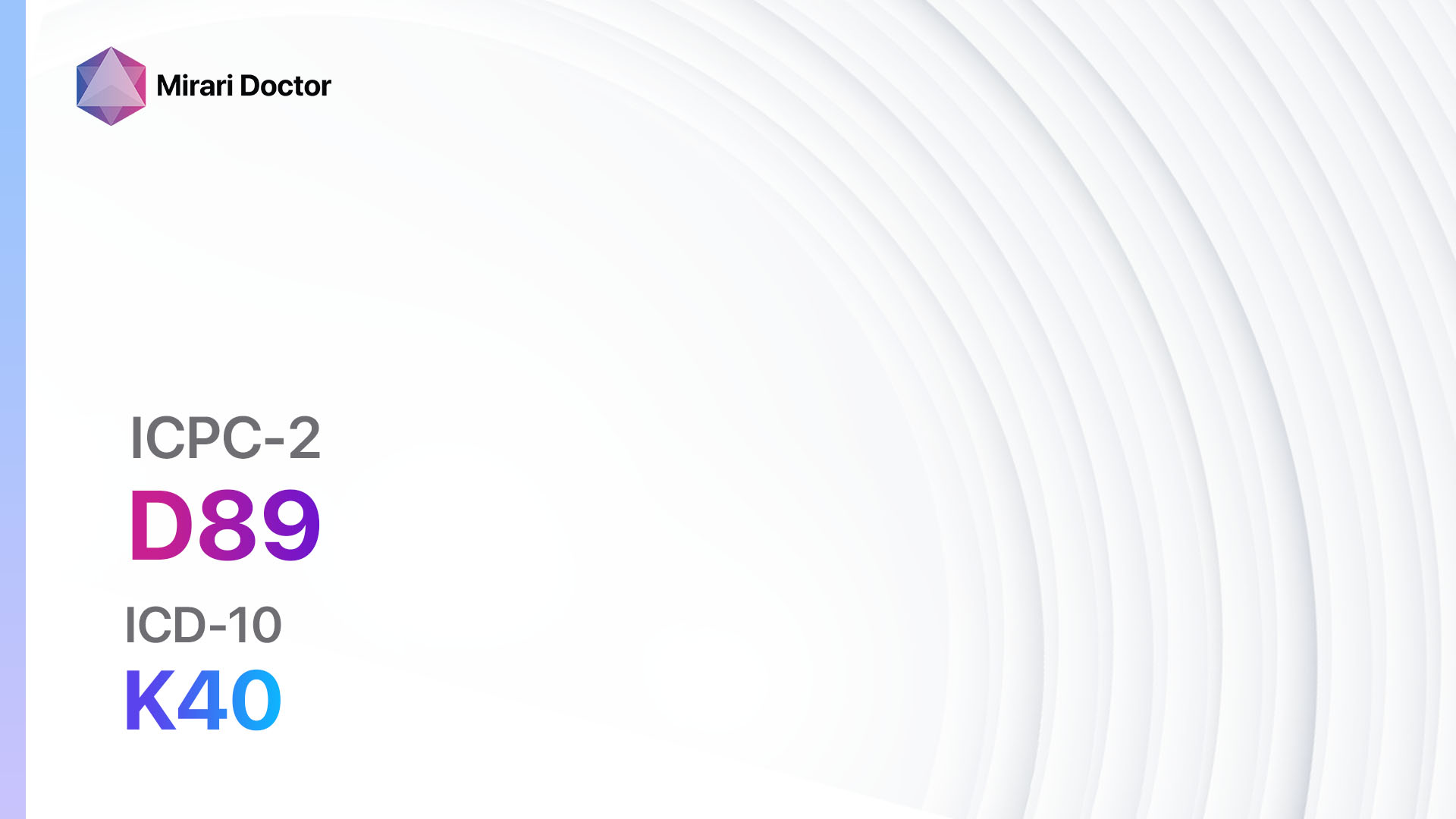
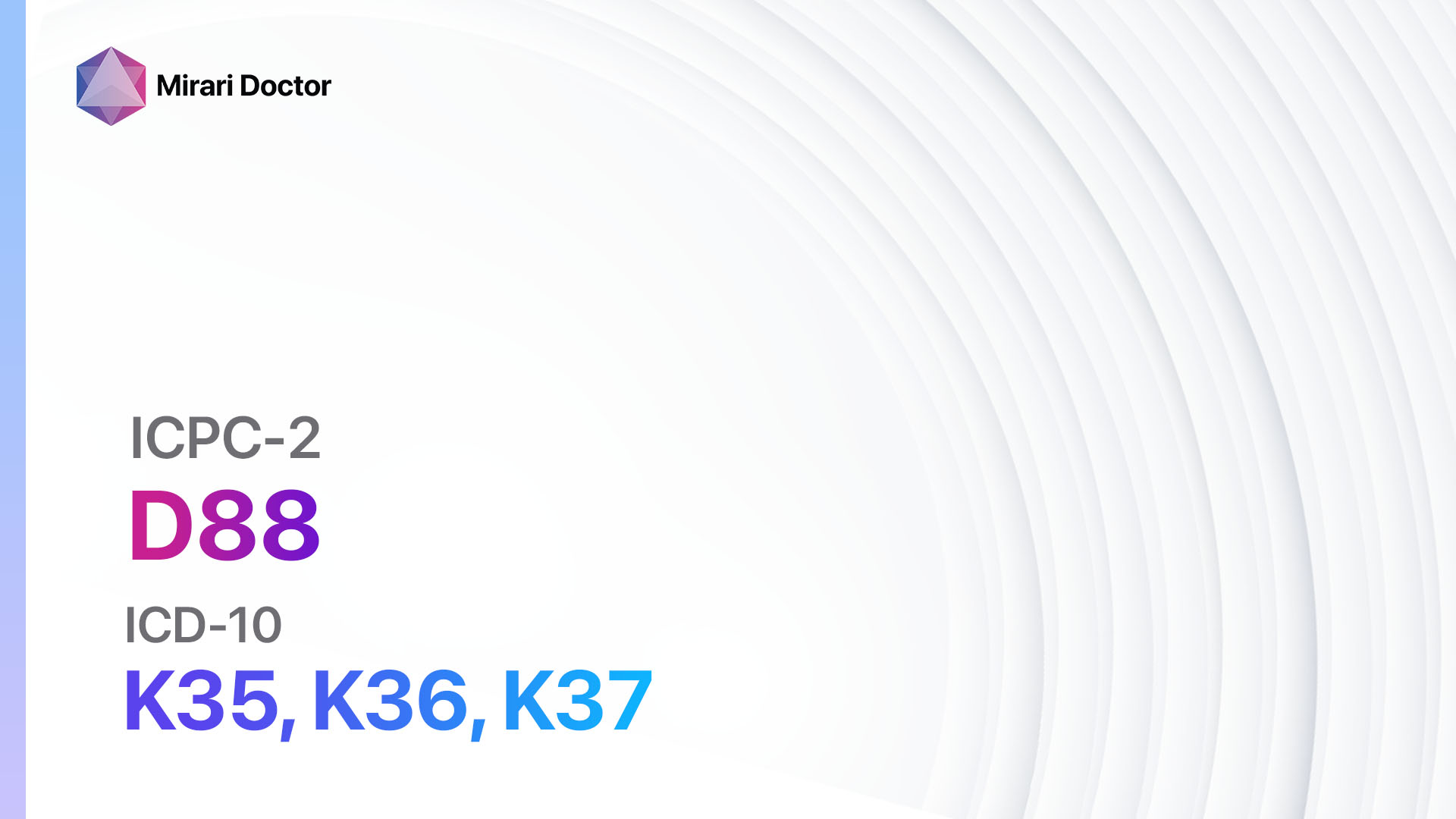
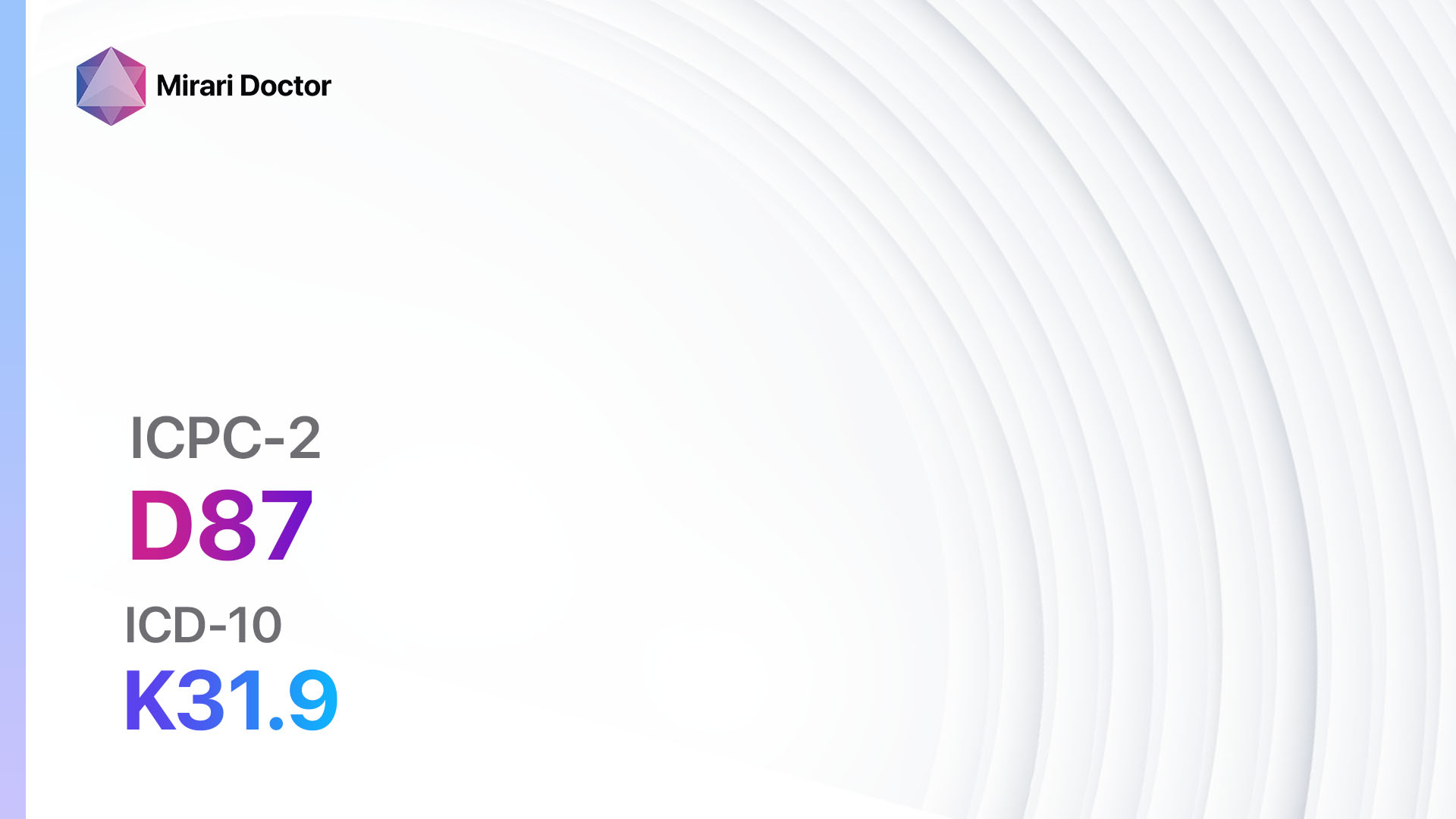
Codes
- ICPC-2 Code: D73 Gastroenteritis presumed infection
- ICD-10 Code: A09.9 Gastroenteritis and colitis of unspecified origin[2]
Symptoms
- Diarrhea: Loose or watery stools that occur more frequently than usual.
- Vomiting: Forceful expulsion of stomach contents through the mouth.
- Abdominal pain: Discomfort or cramping in the stomach or abdominal area.
- Nausea: Feeling of queasiness or the urge to vomit.
- Fever: Elevated body temperature above the normal range[3].
Causes
- Viral infection: Common viruses such as norovirus, rotavirus, and adenovirus can cause gastroenteritis.
- Bacterial infection: Bacteria such as Salmonella, Escherichia coli (E. coli), and Campylobacter can lead to gastroenteritis.
- Parasitic infection: Parasites like Giardia lamblia and Cryptosporidium can cause gastroenteritis[4].
- Foodborne illness: Consuming contaminated food or water can result in gastroenteritis.
- Poor hygiene: Lack of proper handwashing and sanitation can contribute to the spread of gastroenteritis[5].
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration and severity of diarrhea, vomiting, and abdominal pain.
- Inquire about recent travel, exposure to sick individuals, and consumption of potentially contaminated food or water.
- Assess for any underlying medical conditions or medications that may increase the risk of gastroenteritis[6].
Physical Examination
- Perform a thorough abdominal examination to assess for tenderness, distension, or abnormal bowel sounds.
- Check vital signs, including temperature, heart rate, and blood pressure, to evaluate for signs of dehydration or systemic infection.
- Look for any signs of dehydration, such as dry mucous membranes, decreased skin turgor, or sunken eyes[7].
Laboratory Tests
- Stool culture: Collect a stool sample to identify the presence of bacteria, parasites, or viruses.
- Complete blood count (CBC): Evaluate for an elevated white blood cell count, which may indicate an infection.
- Electrolyte panel: Measure levels of electrolytes, such as sodium and potassium, to assess for dehydration.
- C-reactive protein (CRP): Measure CRP levels to determine the presence of inflammation.
- Stool antigen tests: Perform specific antigen tests to detect the presence of certain pathogens, such as rotavirus or norovirus[8].
Diagnostic Imaging
- Abdominal X-ray: May be used to rule out other causes of abdominal pain or to assess for complications such as bowel obstruction.
- Abdominal ultrasound: Can help visualize the gastrointestinal tract and identify any abnormalities or signs of inflammation.
- CT scan: May be necessary in severe cases or when complications are suspected, such as perforation or abscess formation[9].
Other Tests
- Rectal swab: Collect a rectal swab to test for the presence of certain pathogens, such as Clostridium difficile.
- Serology tests: Perform serology tests to detect antibodies against specific pathogens, such as Salmonella or Campylobacter.
- PCR testing: Use polymerase chain reaction (PCR) testing to identify specific viral or bacterial DNA in the stool[10].
Follow-up and Patient Education
- Advise the patient to maintain good hydration by drinking plenty of fluids, such as water, clear broths, or oral rehydration solutions.
- Instruct the patient to rest and avoid solid foods until symptoms improve.
- Provide information on proper hand hygiene and food safety practices to prevent the spread of gastroenteritis.
- Schedule a follow-up appointment to monitor the patient’s progress and ensure resolution of symptoms.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Gastroenteritis presumed infection:
- Oral rehydration solutions (e.g., Pedialyte):
- Cost: $5-$15 for a 1-liter bottle.
- Contraindications: None.
- Side effects: None.
- Severe side effects: None.
- Drug interactions: None.
- Warning: None.
- Antiemetics (e.g., Ondansetron, Metoclopramide):
- Cost: Generic versions can be $10-$50 for a 30-day supply.
- Contraindications: Hypersensitivity, intestinal obstruction.
- Side effects: Headache, dizziness, drowsiness.
- Severe side effects: Tardive dyskinesia, neuroleptic malignant syndrome.
- Drug interactions: Serotonin antagonists, dopamine antagonists.
- Warning: Use caution in patients with a history of seizures or cardiac arrhythmias.
- Antidiarrheal agents (e.g., Loperamide, Bismuth subsalicylate):
- Cost: Generic versions can be $5-$20 for a 30-day supply.
- Contraindications: Severe ulcerative colitis, pseudomembranous colitis.
- Side effects: Constipation, abdominal discomfort.
- Severe side effects: Paralytic ileus, toxic megacolon.
- Drug interactions: Opioids, anticholinergic agents.
- Warning: Use caution in patients with liver dysfunction or renal impairment.
- Probiotics (e.g., Lactobacillus, Bifidobacterium):
- Cost: Varies depending on the brand and formulation.
- Contraindications: None.
- Side effects: None.
- Severe side effects: None.
- Drug interactions: None.
- Warning: None.
- Antibiotics (e.g., Azithromycin, Ciprofloxacin):
- Cost: Generic versions can be $10-$50 for a 10-day supply.
- Contraindications: Hypersensitivity, myasthenia gravis.
- Side effects: Nausea, diarrhea, abdominal pain.
- Severe side effects: Tendon rupture, Clostridium difficile infection.
- Drug interactions: Antacids, warfarin.
- Warning: Use caution in patients with a history of QT prolongation or liver disease.
Alternative Drugs:
- Lactase supplements: Can help alleviate symptoms in individuals with lactose intolerance.
- Antiviral medications: May be prescribed for specific viral causes of gastroenteritis, such as norovirus or rotavirus.
- Antiparasitic medications: Used to treat parasitic infections, such as Giardia or Cryptosporidium.
Surgical Procedures:
In general, surgical intervention is not required for the treatment of gastroenteritis presumed infection. However, in rare cases where complications such as bowel obstruction or perforation occur, surgical consultation may be necessary.
Alternative Interventions
- Probiotics: Can help restore the balance of gut bacteria and alleviate symptoms. Cost: $10-$50 for a 30-day supply.
- Herbal remedies: Certain herbs, such as ginger or peppermint, may help reduce nausea and improve digestion. Cost: Varies depending on the specific herb and formulation.
- Acupuncture: May help alleviate symptoms and promote overall well-being. Cost: $60-$120 per session.
- Homeopathic remedies: Some individuals find relief from gastroenteritis symptoms with homeopathic treatments. Cost: Varies depending on the specific remedy and formulation.
- Hydrotherapy: The use of water-based therapies, such as hot or cold compresses, may provide symptomatic relief. Cost: Varies depending on the specific therapy and location.
Lifestyle Interventions
- Fluid and electrolyte replacement: Encourage the patient to drink plenty of fluids and consume electrolyte-rich foods to prevent dehydration.
- Dietary modifications: Advise the patient to avoid spicy, fatty, or greasy foods that may exacerbate symptoms. Instead, recommend bland, easily digestible foods such as rice, bananas, and toast.
- Rest and relaxation: Emphasize the importance of rest and relaxation to allow the body to recover and heal.
- Good hygiene practices: Educate the patient on proper handwashing techniques and food safety practices to prevent the spread of gastroenteritis.
- Stress reduction: Stress can worsen symptoms of gastroenteritis, so encourage the patient to engage in stress-reducing activities such as meditation or yoga.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – D73 Gastroenteritis presumed infection (ICD-10:A09.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 3 (Antiviral Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 3 (Antiviral Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes | Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes | Mode setting: 7 (Immunotherapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD | Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, | Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520USD – $3,360 USD | Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD |
 |
|
Use the Mirari Cold Plasma device to treat Gastroenteritis presumed infection effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Gastroenteritis presumed infection. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Elliott EJ. Acute gastroenteritis in children. BMJ. 2007;334(7583):35-40. doi:10.1136/bmj.39036.406169.80
- World Health Organization. International Classification of Diseases (ICD). Accessed June 8, 2024.//www.who.int/standards/classifications/classification-of-diseases
- Chow CM, Leung AK, Hon KL. Acute gastroenteritis: from guidelines to real life. Clin Exp Gastroenterol. 2010;3:97-112. Published 2010 Jul 15. doi:10.2147/ceg.s6554
- Bányai K, Estes MK, Martella V, Parashar UD. Viral gastroenteritis. Lancet. 2018;392(10142):175-186. doi:10.1016/S0140-6736(18)31128-0
- Ejemot-Nwadiaro RI, Ehiri JE, Arikpo D, Meremikwu MM, Critchley JA. Hand washing promotion for preventing diarrhoea. Cochrane Database Syst Rev. 2015;2015(9):CD004265. Published 2015 Sep 3. doi:10.1002/14651858.CD004265.pub3
- Shane AL, Mody RK, Crump JA, et al. 2017 Infectious Diseases Society of America Clinical Practice Guidelines for the Diagnosis and Management of Infectious Diarrhea. Clin Infect Dis. 2017;65(12):e45-e80. doi:10.1093/cid/cix669
- King CK, Glass R, Bresee JS, Duggan C; Centers for Disease Control and Prevention. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR Recomm Rep. 2003;52(RR-16):1-16.
- Binnicker MJ. Multiplex Molecular Panels for Diagnosis of Gastrointestinal Infection: Performance, Result Interpretation, and Cost-Effectiveness. J Clin Microbiol. 2015;53(12):3723-3728. doi:10.1128/JCM.02103-15
- O’Ryan GM, Ashkenazi-Hoffnung L, O’Ryan-Soriano MA, Ashkenazi S. Management of acute infectious diarrhea for children living in resource-limited settings. Expert Rev Anti Infect Ther. 2014;12(5):621-632. doi:10.1586/14787210.2014.901168
- Buss SN, Leber A, Chapin K, et al. Multicenter evaluation of the BioFire FilmArray gastrointestinal panel for etiologic diagnosis of infectious gastroenteritis. J Clin Microbiol. 2015;53(3):915-925. doi:10.1128/JCM.02674-14
Related articles
Made in USA