Introduction
Haematemesis, also known as vomiting blood, is a medical condition characterized by the presence of blood in vomit. It is a potentially serious symptom that may indicate an underlying medical condition[1]. The aim of this guide is to provide a comprehensive overview of the diagnostic steps, possible interventions, and patient education related to haematemesis.
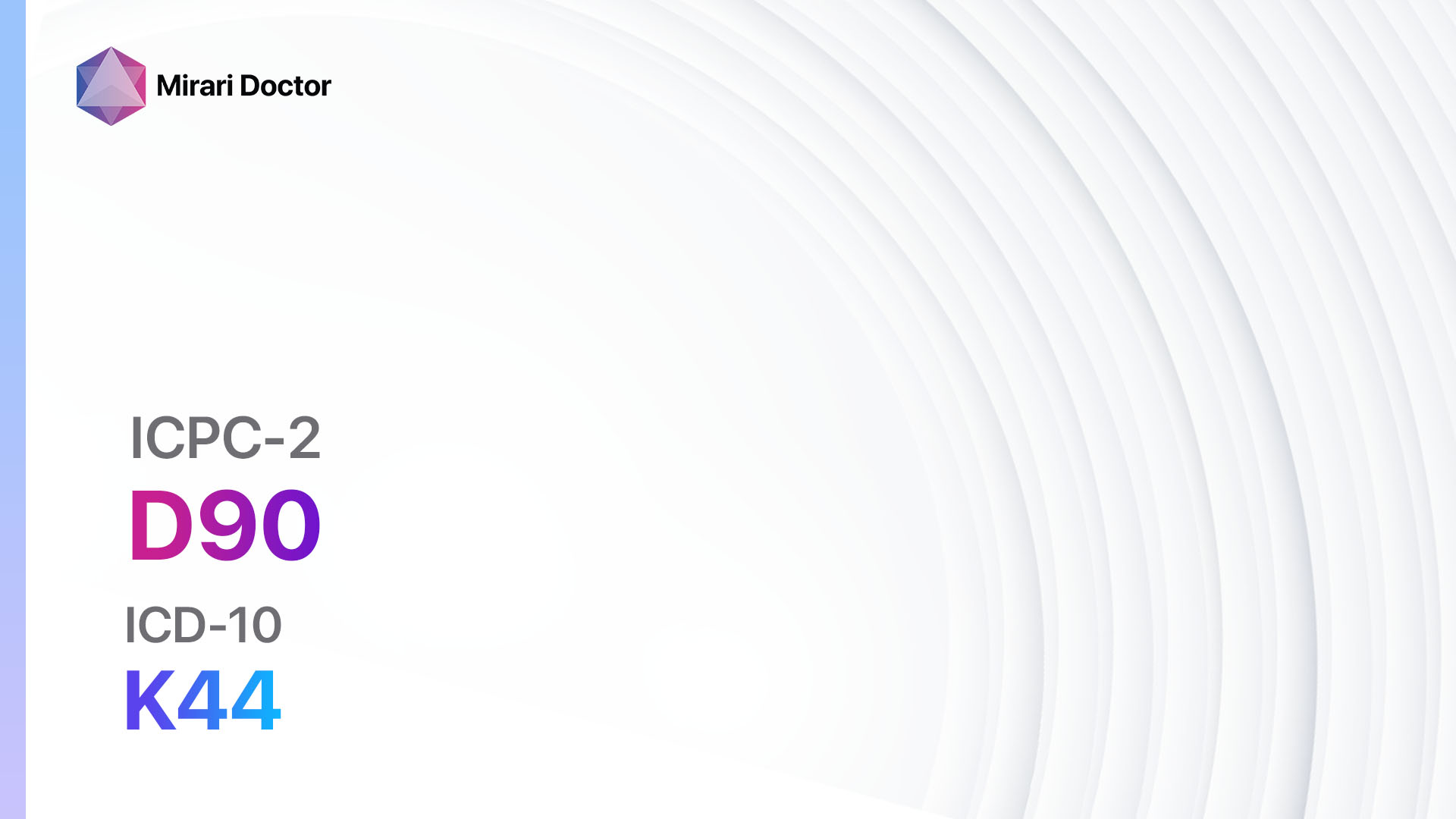
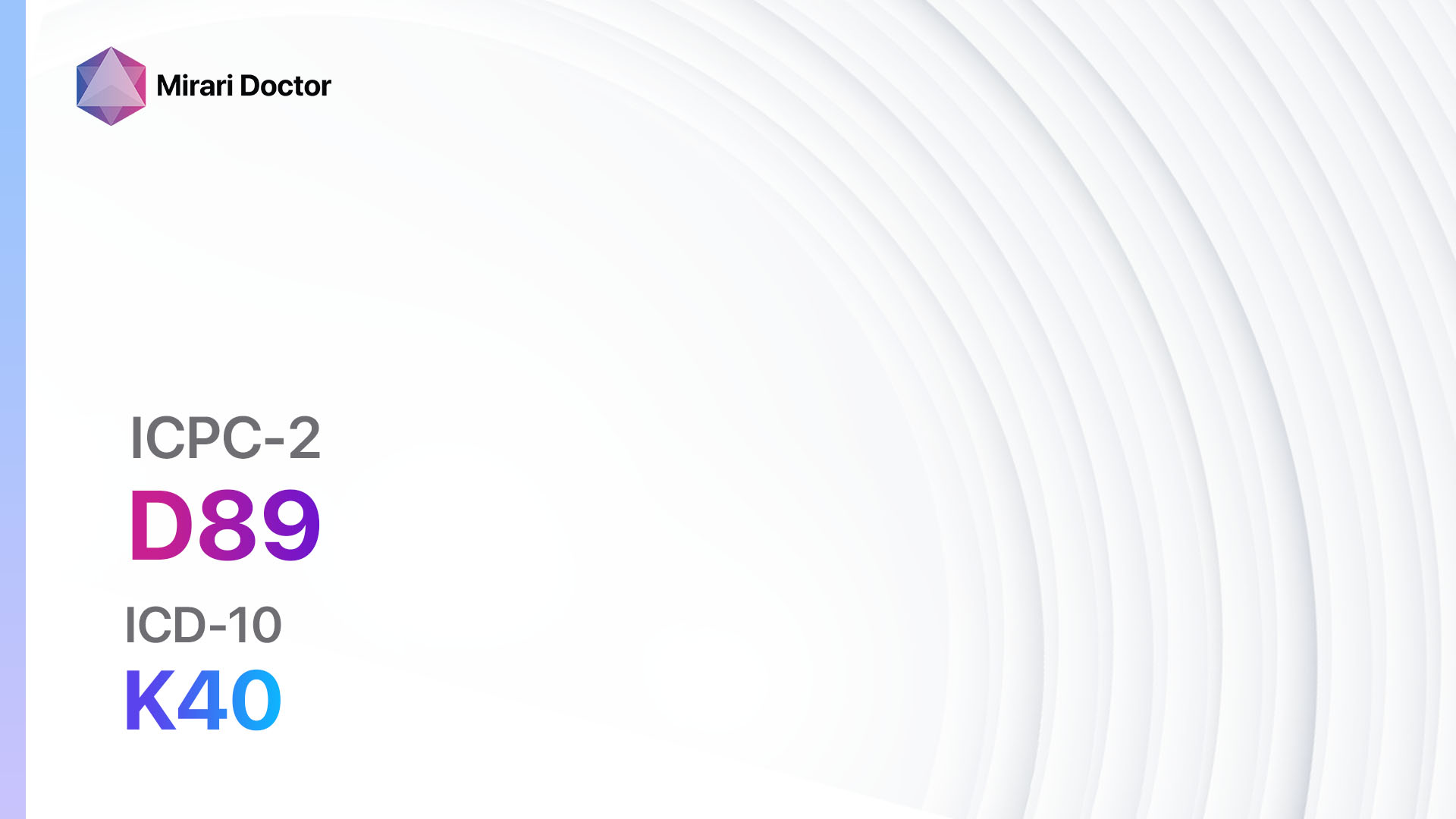
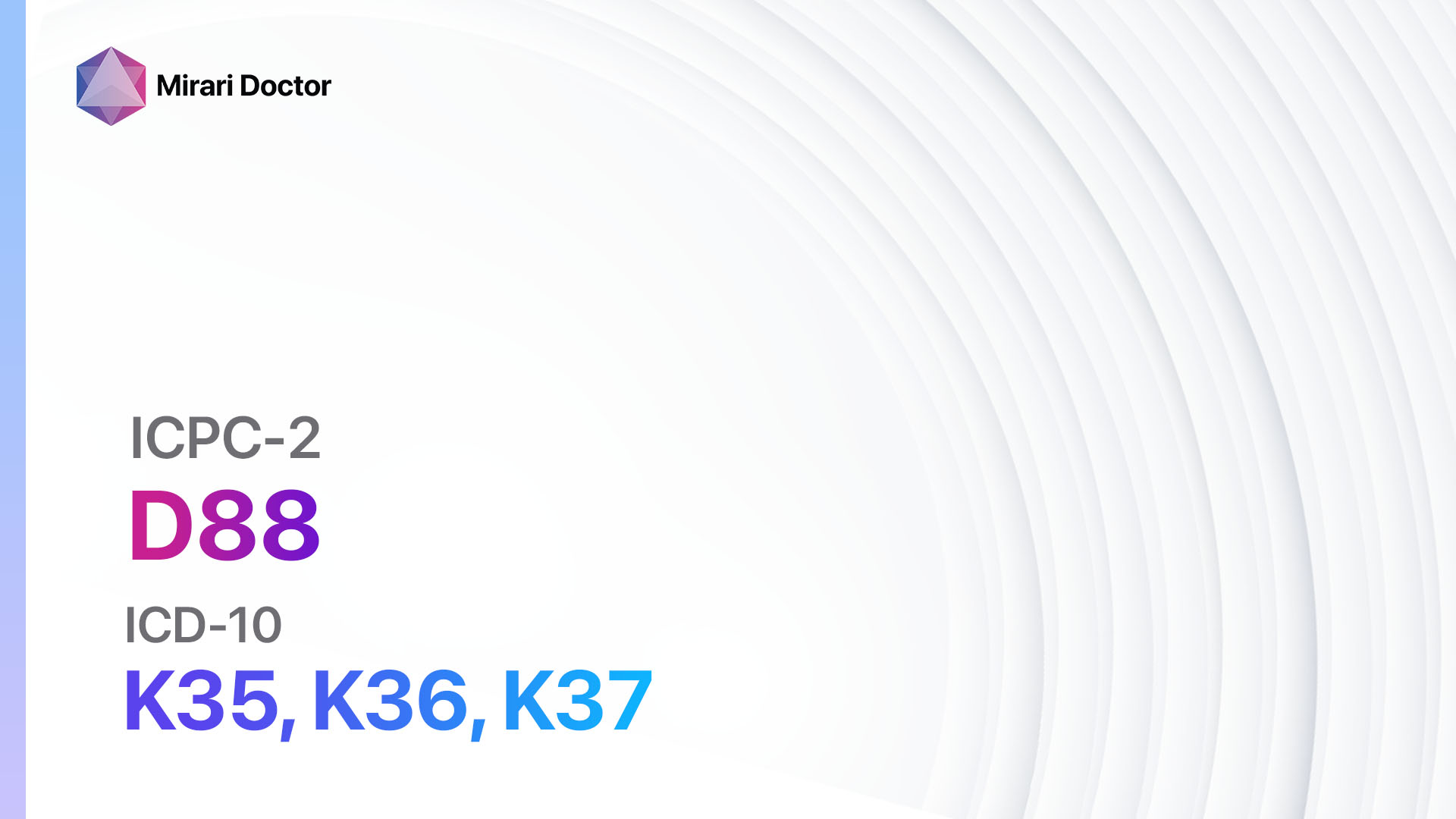
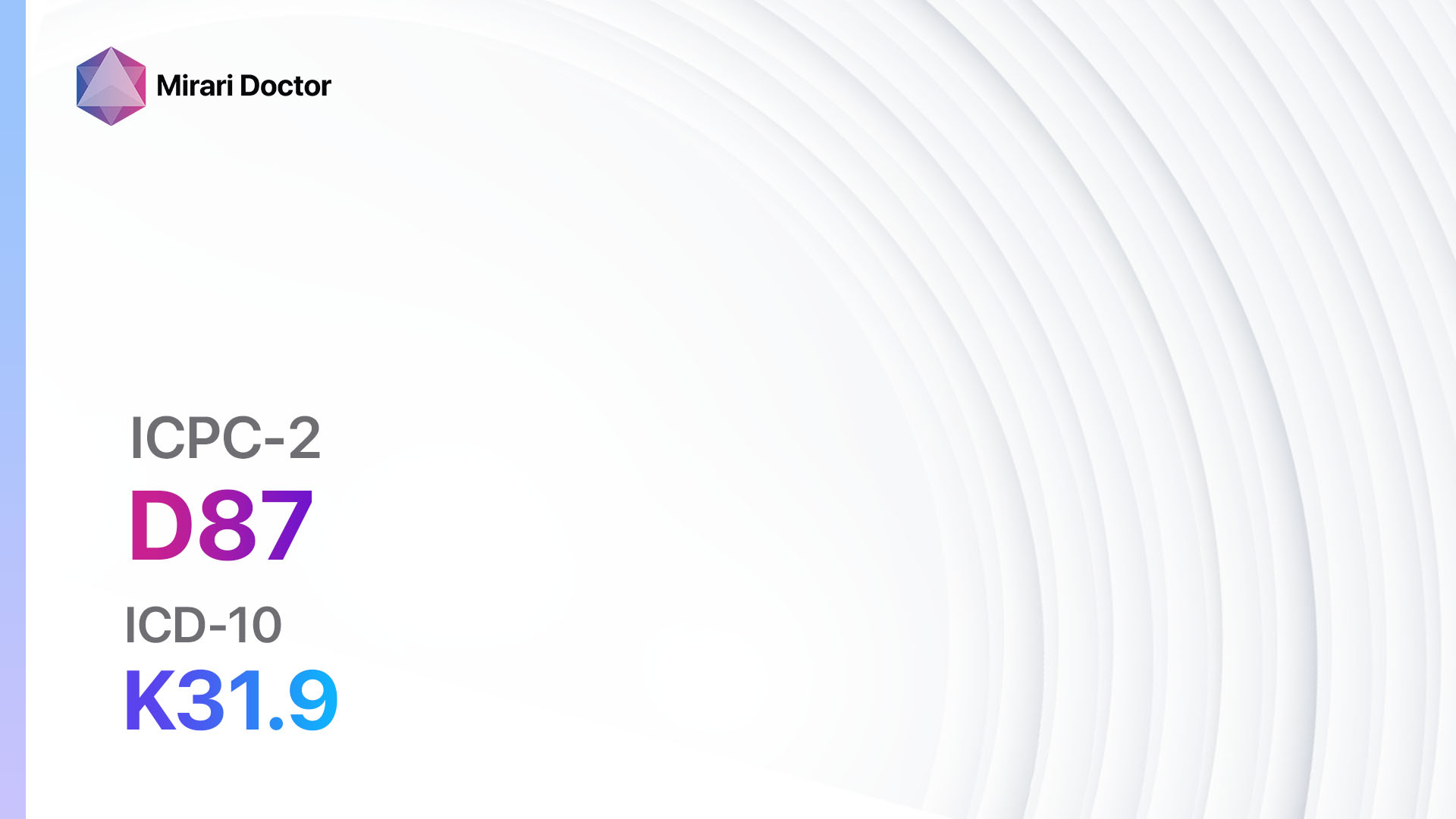
Codes
Symptoms
- Vomiting blood: The presence of blood in vomit, which may range from bright red to dark and coffee-ground-like in appearance[2].
- Nausea and vomiting: Feeling of nausea and recurrent episodes of vomiting[3].
- Abdominal pain: Discomfort or pain in the abdominal region[4].
- Weakness and fatigue: Feeling weak and tired[5].
- Pale skin: Skin appears pale due to decreased blood volume[6].
Causes
- Peptic ulcers: Open sores that develop on the lining of the stomach or upper part of the small intestine[7].
- Esophageal varices: Enlarged veins in the lower part of the esophagus, usually caused by liver cirrhosis[8].
- Mallory-Weiss tear: Tear in the lining of the esophagus or stomach, often caused by severe vomiting or retching[9].
- Gastritis: Inflammation of the stomach lining[10].
- Gastroesophageal reflux disease (GERD): Chronic acid reflux that causes irritation and inflammation of the esophagus.
- Esophagitis: Inflammation of the esophagus, often caused by acid reflux or infections.
- Gastric or duodenal ulcers: Open sores that develop on the lining of the stomach or upper part of the small intestine.
- Cancer: Tumors in the esophagus, stomach, or other parts of the gastrointestinal tract.
- Medications: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners, may increase the risk of haematemesis.
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the frequency and duration of haematemesis episodes.
- Inquire about any previous medical conditions, such as peptic ulcers, liver disease, or gastrointestinal disorders.
- Assess the patient’s medication history, including the use of NSAIDs or blood thinners.
- Ask about any recent trauma or injury to the abdominal region.
Physical Examination
- Perform a thorough physical examination, including vital signs, abdominal palpation, and assessment of the gastrointestinal system.
- Look for signs of anemia, such as pale skin or conjunctiva.
- Check for signs of liver disease, such as jaundice or enlarged liver.
- Assess for signs of gastrointestinal bleeding, such as melena (dark, tarry stools) or hematochezia (bright red blood in the stool).
Laboratory Tests
- Complete blood count (CBC): To assess for anemia and evaluate the blood cell counts.
- Liver function tests: To evaluate liver function and assess for liver disease.
- Coagulation profile: To assess the blood’s ability to clot and rule out bleeding disorders.
- Electrolyte levels: To evaluate the patient’s fluid and electrolyte balance.
- Blood type and crossmatch: To prepare for potential blood transfusion if needed.
Diagnostic Imaging
- Upper gastrointestinal endoscopy: A flexible tube with a camera is inserted through the mouth to visualize the esophagus, stomach, and upper part of the small intestine.
- Abdominal ultrasound: To assess the liver and other abdominal organs for abnormalities.
- CT scan or MRI: To obtain detailed images of the gastrointestinal tract and identify any tumors or structural abnormalities.
Other Tests
- Stool occult blood test: To check for the presence of blood in the stool.
- Helicobacter pylori testing: To determine if the bacteria H. pylori is present, which is associated with peptic ulcers.
- Esophageal manometry: To measure the pressure and movement of the esophagus.
- Capsule endoscopy: A small capsule with a camera is swallowed to visualize the entire gastrointestinal tract.
Follow-up and Patient Education
- Schedule a follow-up appointment to discuss the results of the diagnostic tests and determine the appropriate treatment plan.
- Educate the patient about the importance of adhering to prescribed medications and lifestyle modifications.
- Provide information on potential complications and when to seek immediate medical attention.
- Encourage the patient to maintain regular follow-up appointments for monitoring and further evaluation.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for haematemesis/vomiting blood:
- Proton pump inhibitors (e.g., Omeprazole, Pantoprazole):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Headache, diarrhea, abdominal pain.
- Severe side effects: Severe allergic reactions, liver problems.
- Drug interactions: Clopidogrel, methotrexate, digoxin.
- Warning: Long-term use may increase the risk of fractures and certain infections.
- H2 receptor blockers (e.g., Ranitidine, Famotidine):
- Cost: Generic versions can be $10-$30/month.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Headache, dizziness, constipation.
- Severe side effects: Rare, but may include blood disorders or liver problems.
- Drug interactions: Warfarin, phenytoin, theophylline.
- Warning: Rare cases of allergic reactions or anaphylaxis have been reported.
- Antacids (e.g., Aluminum hydroxide, Magnesium hydroxide):
- Cost: Over-the-counter options are available at a low cost.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Constipation or diarrhea, stomach cramps.
- Severe side effects: Rare, but may include kidney problems or electrolyte imbalances.
- Drug interactions: Tetracycline, quinolone antibiotics.
- Warning: Long-term use may lead to metabolic alkalosis or kidney stones.
- Antiemetics (e.g., Ondansetron, Metoclopramide):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to the medication, gastrointestinal obstruction.
- Side effects: Headache, dizziness, drowsiness.
- Severe side effects: Rare, but may include movement disorders or serotonin syndrome.
- Drug interactions: Serotonergic medications, dopamine antagonists.
- Warning: Use caution in patients with a history of seizures or cardiovascular disease.
- Vitamin K:
- Cost: Over-the-counter options are available at a low cost.
- Contraindications: Hypersensitivity to the medication.
- Side effects: Rare, but may include allergic reactions or injection site reactions.
- Severe side effects: Rare, but may include anaphylaxis or severe allergic reactions.
- Drug interactions: Anticoagulant medications.
- Warning: Use under the guidance of a healthcare professional.
Alternative Drugs:
- Tranexamic acid: An antifibrinolytic medication that helps prevent bleeding.
- Octreotide: A medication that reduces blood flow to the gastrointestinal tract.
- Esomeprazole: A proton pump inhibitor similar to omeprazole.
- Sucralfate: A medication that forms a protective coating over ulcers.
Surgical Procedures:
- Endoscopic therapy: Involves using an endoscope to treat bleeding ulcers or varices.
- Transjugular intrahepatic portosystemic shunt (TIPS): A shunt is placed to redirect blood flow in the liver and reduce pressure in the portal vein.
- Surgical repair: In cases of severe bleeding or structural abnormalities, surgery may be necessary to repair or remove the affected area.
Alternative Interventions
- Acupuncture: May help reduce nausea and improve overall well-being. Cost: $60-$120 per session.
- Herbal supplements: Certain herbs, such as ginger or chamomile, may help alleviate symptoms of nausea and promote digestion. Cost: Varies depending on the specific supplement.
- Hypnotherapy: Can help manage stress and anxiety, which may contribute to symptoms of haematemesis. Cost: $100-$200 per session.
- Mind-body techniques: Practices such as meditation or yoga may help reduce stress and improve overall well-being. Cost: Varies depending on the specific practice.
- Dietary modifications: Avoiding spicy or acidic foods, eating smaller meals, and avoiding alcohol and caffeine may help reduce symptoms. Cost: Varies depending on individual food choices.
Lifestyle Interventions
- Smoking cessation: Smoking can worsen symptoms and delay healing. Cost: Varies depending on the method used for smoking cessation.
- Alcohol moderation: Limiting or avoiding alcohol can help reduce the risk of gastrointestinal bleeding. Cost: Varies depending on individual alcohol consumption.
- Stress management: Engaging in stress-reducing activities, such as exercise, meditation, or therapy, may help improve symptoms. Cost: Varies depending on the specific activity or therapy.
- Healthy diet: Consuming a balanced diet rich in fruits, vegetables, and whole grains can promote overall gastrointestinal health. Cost: Varies depending on individual food choices.
- Regular exercise: Engaging in regular physical activity can help improve digestion and reduce stress. Cost: Varies depending on individual preferences and access to exercise facilities.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions. It is recommended to consult with a healthcare professional for personalized treatment options and cost estimates.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – D14 Haematemesis/vomiting blood (ICD-10:K92.0)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 6 (Liver/Kidney Therapy) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Haematemesis/vomiting blood effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Haematemesis/vomiting blood. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Biecker, E. (2015). Diagnosis and therapy of non-variceal upper gastrointestinal bleeding. World Journal of Gastrointestinal Pharmacology and Therapeutics, 6(4), 172-182.
- Cappell, M. S., & Friedel, D. (2008). Initial management of acute upper gastrointestinal bleeding: from initial evaluation up to gastrointestinal endoscopy. Medical Clinics of North America, 92(3), 491-509.
- Laine, L., & Jensen, D. M. (2012). Management of patients with ulcer bleeding. American Journal of Gastroenterology, 107(3), 345-360.
- Gralnek, I. M., Dumonceau, J. M., Kuipers, E. J., Lanas, A., Sanders, D. S., Kurien, M., … & Hassan, C. (2015). Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy, 47(10), a1-a46.
- Srygley, F. D., Gerardo, C. J., Tran, T., & Fisher, D. A. (2012). Does this patient have a severe upper gastrointestinal bleed?. Jama, 307(10), 1072-1079.
- Witting, M. D., Magder, L., Heins, A. E., Mattu, A., Granja, C. A., & Baumgarten, M. (2006). ED predictors of upper gastrointestinal tract bleeding in patients without hematemesis. The American journal of emergency medicine, 24(3), 280-285.
- Lau, J. Y., Sung, J., Hill, C., Henderson, C., Howden, C. W., & Metz, D. C. (2011). Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality. Digestion, 84(2), 102-113.
- Garcia-Tsao, G., & Bosch, J. (2010). Management of varices and variceal hemorrhage in cirrhosis. New England Journal of Medicine, 362(9), 823-832.
- Kortas, D. Y., Haas, L. S., Simpson, W. G., Nickl III, N. J., & Gates, L. K. (2001). Mallory-Weiss tear: predisposing factors and predictors of a complicated course. The American journal of gastroenterology, 96(10), 2863-2865.
- Toljamo, K. T., Niemelä, S. E., Karttunen, T. J., & Karvonen, A. L. (2012). Clinical significance and outcome of gastric mucosal erosions. Digestive diseases and sciences, 57(12), 2927-2936.
Related articles
Made in USA