Introduction
Diabetes noninsulin dependent, also known as type 2 diabetes, is a chronic condition characterized by high blood sugar levels. It is a significant health concern worldwide, affecting millions of individuals[1]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnosis and management of diabetes noninsulin dependent.
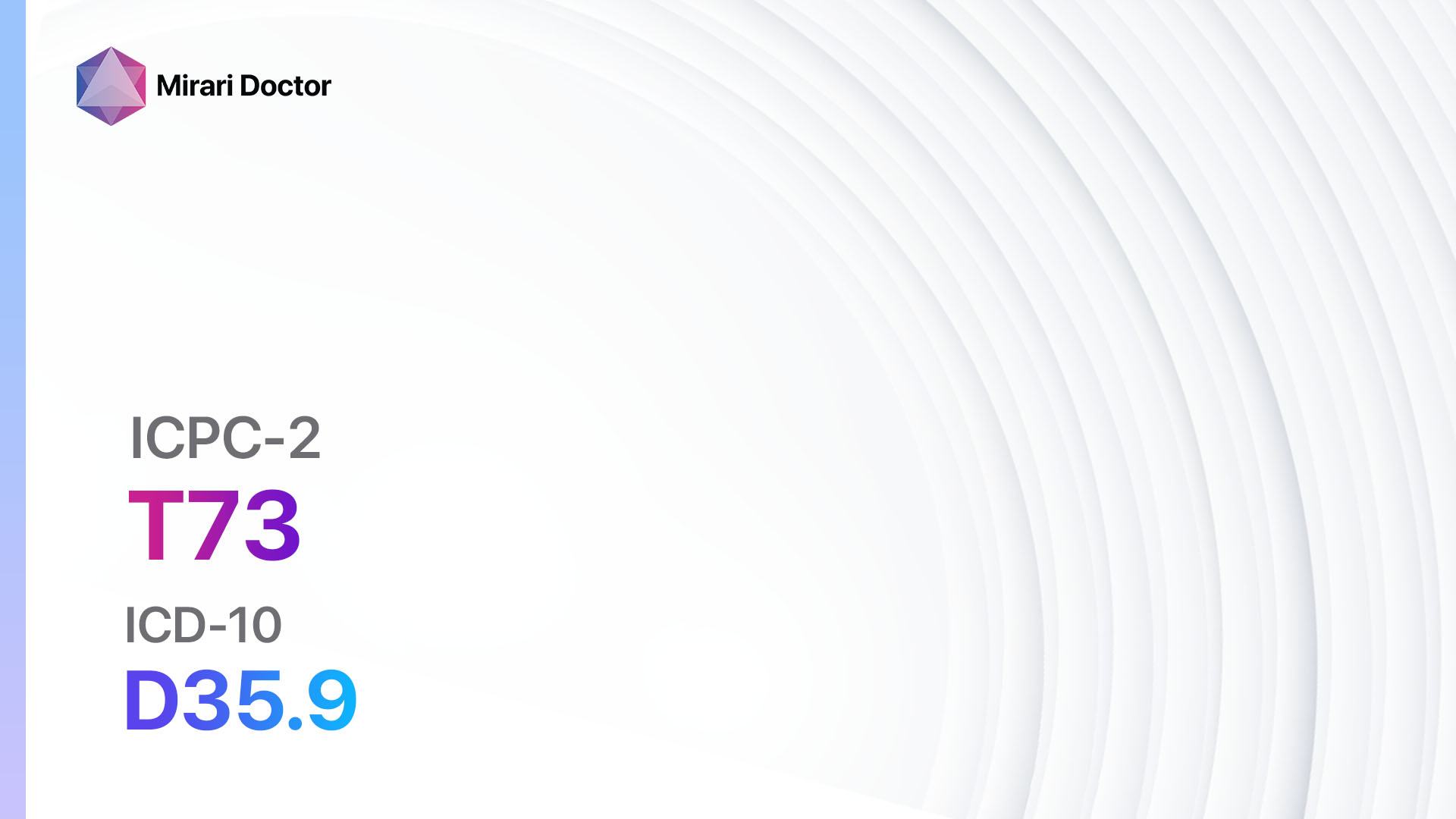
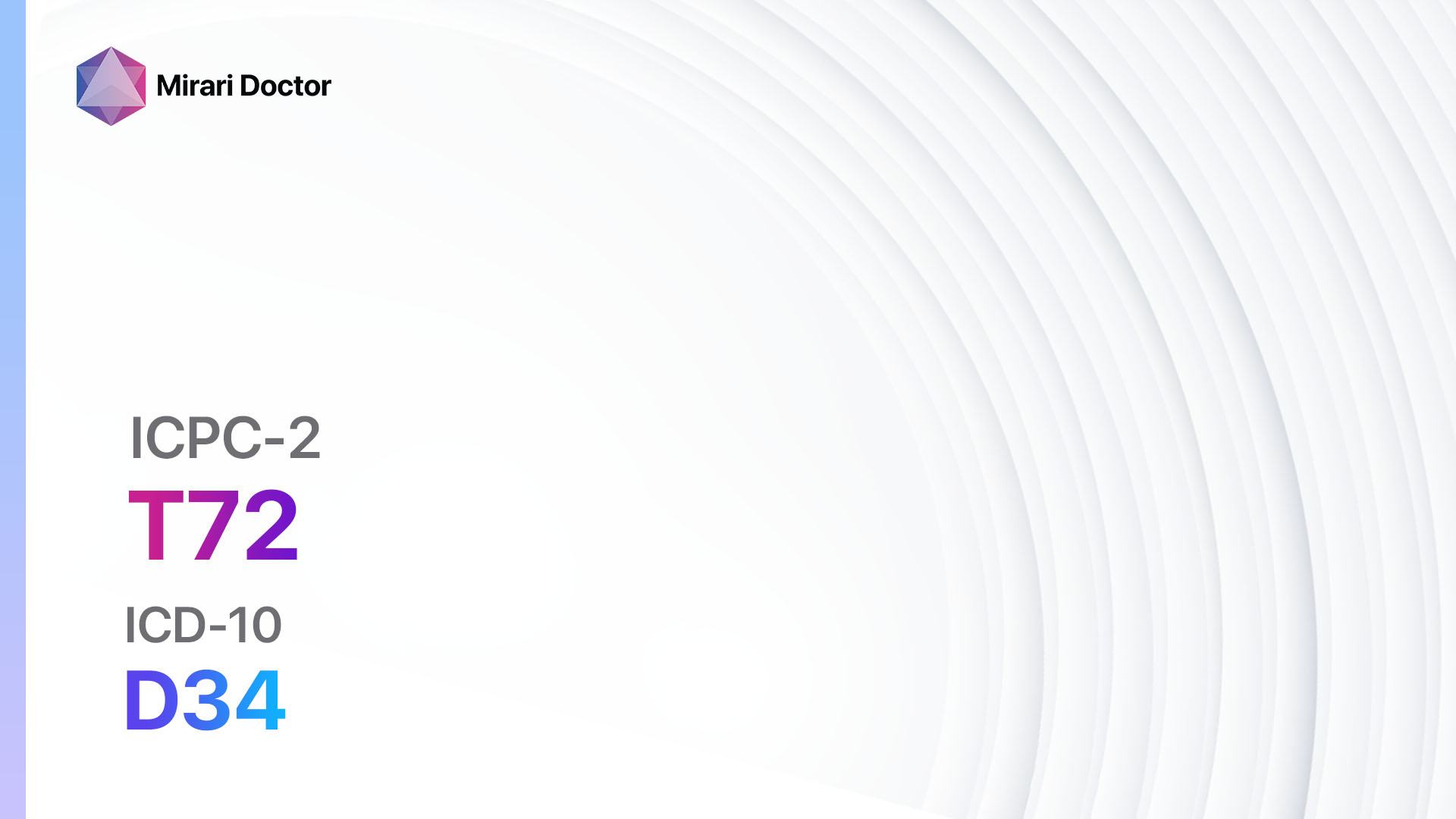
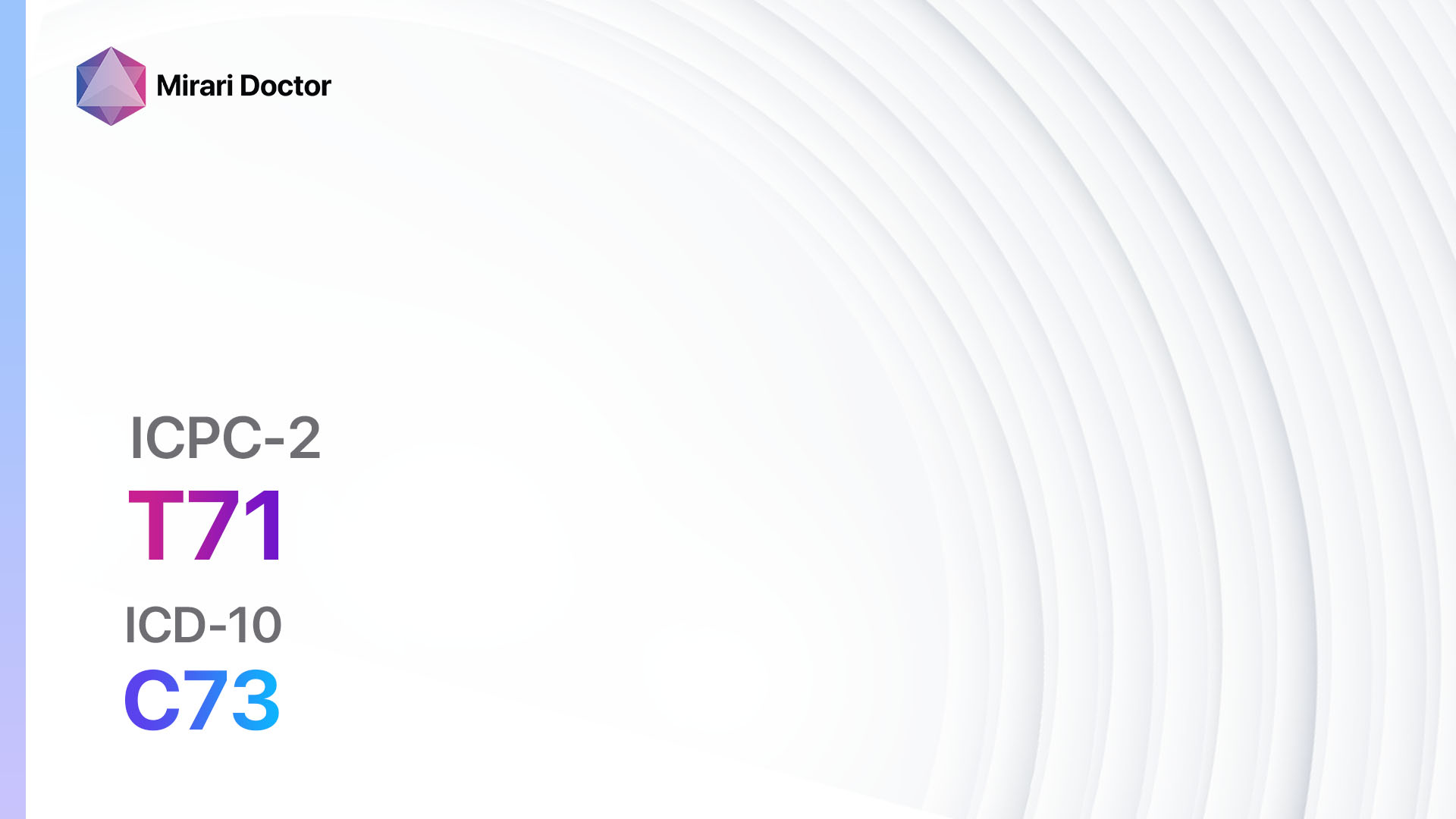
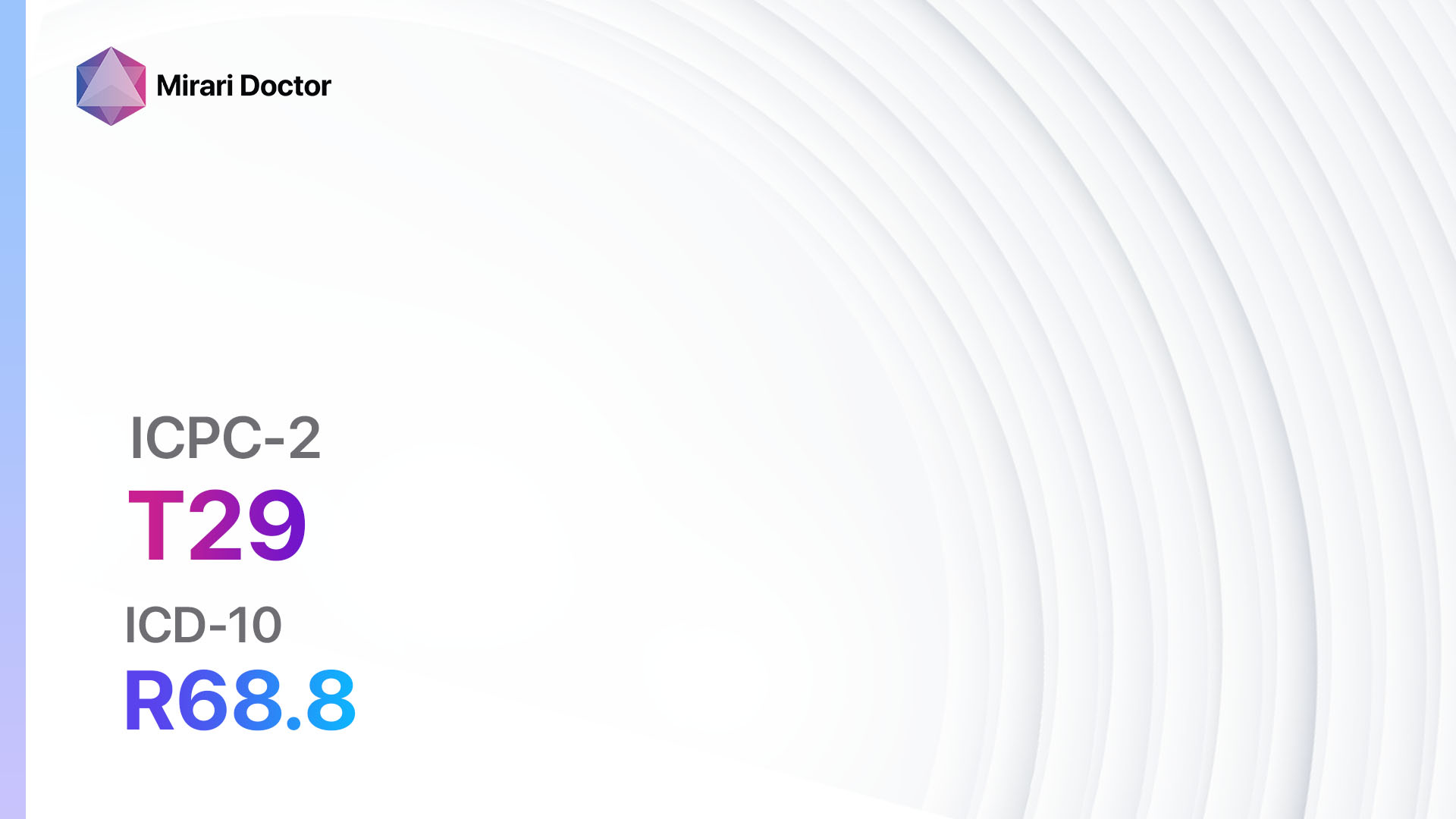
Codes
- ICPC-2 Code: T90 Diabetes non-insulin dependent
- ICD-10 Code: E11.9 Type 2 diabetes mellitus without complications
Symptoms
- Increased thirst: Patients may experience excessive thirst and have a constant need to drink fluids[2].
- Frequent urination: Increased urination, especially during the night, is a common symptom[2].
- Fatigue: Patients may feel tired and lack energy[2].
- Blurred vision: High blood sugar levels can cause changes in vision[2].
- Slow healing of wounds: Wounds may take longer to heal[2].
- Tingling or numbness in the hands or feet: This is known as peripheral neuropathy and is a common symptom of diabetes[3].
Causes
- Obesity: Being overweight or obese is a significant risk factor for developing type 2 diabetes[4].
- Sedentary lifestyle: Lack of physical activity increases the risk of developing diabetes[4].
- Poor diet: Consuming a diet high in processed foods, sugary drinks, and unhealthy fats can contribute to the development of diabetes[4].
- Genetics: Family history of diabetes can increase the risk of developing the condition[5].
- Age: The risk of developing type 2 diabetes increases with age[5].
Diagnostic Steps
Medical History
- Gather information about the patient’s risk factors, such as family history of diabetes, obesity, and sedentary lifestyle[6].
- Inquire about symptoms related to diabetes, such as increased thirst, frequent urination, and fatigue[6].
- Assess the patient’s medical history for conditions associated with diabetes, such as hypertension and cardiovascular disease[6].
Physical Examination
- Measure the patient’s blood pressure to assess for hypertension, a common comorbidity of diabetes[7].
- Examine the patient’s body mass index (BMI) to determine if they are overweight or obese[7].
- Check for signs of peripheral neuropathy, such as tingling or numbness in the hands or feet[7].
- Assess for signs of diabetic retinopathy, such as changes in vision[7].
Laboratory Tests
- Fasting plasma glucose test: A blood test to measure the patient’s blood sugar levels after fasting for at least 8 hours.
- A result of 126 mg/dL or higher on two separate occasions indicates diabetes[8].
- Oral glucose tolerance test: A blood test to measure the patient’s blood sugar levels 2 hours after consuming a sugary drink.
- A result of 200 mg/dL or higher indicates diabetes[8].
- Hemoglobin A1c test: A blood test that provides an average of the patient’s blood sugar levels over the past 2-3 months.
- A result of 6.5% or higher indicates diabetes[8].
Diagnostic Imaging
- None required for the diagnosis of diabetes noninsulin dependent.
Other Tests
- Lipid profile: A blood test to assess the patient’s cholesterol levels, which can help determine their cardiovascular risk.
- Kidney function tests: A blood test to assess the patient’s kidney function, as diabetes can lead to kidney damage.
- Electrocardiogram (ECG): A test to assess the patient’s heart function and detect any abnormalities[9].
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the patient’s blood sugar levels and adjust treatment if necessary.
- Provide education on diabetes management, including the importance of a healthy diet, regular exercise, and medication adherence.
- Encourage the patient to monitor their blood sugar levels at home and keep a record of their readings[10].
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Diabetes noninsulin dependent:
- Metformin:
- Cost: Generic versions can be as low as $4/month.
- Contraindications: Severe kidney disease, liver disease, and heart failure.
- Side effects: Nausea, diarrhea, and abdominal discomfort.
- Severe side effects: Lactic acidosis (rare but serious).
- Drug interactions: Alcohol, certain medications for heart disease.
- Warning: Regular kidney function tests required.
- Sulfonylureas (e.g., Glimepiride, Glipizide):
- Cost: Generic versions can be as low as $4/month.
- Contraindications: Severe kidney or liver disease, type 1 diabetes.
- Side effects: Hypoglycemia, weight gain.
- Severe side effects: Severe hypoglycemia (rare).
- Drug interactions: Alcohol, certain medications for heart disease.
- Warning: Regular blood sugar monitoring required.
- DPP-4 inhibitors (e.g., Sitagliptin, Saxagliptin):
- Cost: Brand-name versions can range from $200-$500/month. Generic versions may be available at a lower cost.
- Contraindications: Severe kidney disease.
- Side effects: Upper respiratory tract infection, headache.
- Severe side effects: Pancreatitis (rare).
- Drug interactions: None significant.
- Warning: Regular kidney function tests required.
- GLP-1 receptor agonists (e.g., Liraglutide, Dulaglutide):
- Cost: Brand-name versions can range from $500-$800/month.
- Contraindications: Personal or family history of medullary thyroid cancer or multiple endocrine neoplasia syndrome type 2.
- Side effects: Nausea, vomiting, diarrhea.
- Severe side effects: Pancreatitis (rare), thyroid cancer (rare).
- Drug interactions: None significant.
- Warning: Regular thyroid function tests required.
- SGLT2 inhibitors (e.g., Empagliflozin, Canagliflozin):
- Cost: Brand-name versions can range from $400-$600/month.
- Contraindications: Severe kidney disease, dialysis.
- Side effects: Genital yeast infections, urinary tract infections.
- Severe side effects: Diabetic ketoacidosis (rare), lower limb amputation (rare).
- Drug interactions: None significant.
- Warning: Regular kidney function tests required.
Alternative Drugs:
- Alpha-glucosidase inhibitors (e.g., Acarbose): Slows down the digestion of carbohydrates in the intestines.
- Thiazolidinediones (e.g., Pioglitazone): Improves insulin sensitivity in the body.
- Bile acid sequestrants (e.g., Colesevelam): Helps lower blood sugar levels by binding to bile acids in the intestines.
- Meglitinides (e.g., Repaglinide): Stimulates the release of insulin from the pancreas.
- Dopamine agonists (e.g., Bromocriptine): Helps lower blood sugar levels by acting on the brain.
Surgical Procedures:
- Bariatric surgery: A surgical procedure to promote weight loss in individuals with obesity and diabetes. Cost: $20,000 to $35,000.
- Pancreatic islet cell transplantation: A procedure to transplant insulin-producing cells into the pancreas. Cost: $150,000 to $200,000.
Alternative Interventions
- Acupuncture: May help improve blood sugar control and reduce insulin resistance. Cost: $60-$120 per session.
- Yoga: Can improve insulin sensitivity and promote weight loss. Cost: Varies depending on the location and instructor.
- Mindfulness-based stress reduction: Reduces stress levels, which can help improve blood sugar control. Cost: $300-$500 for an 8-week program.
- Herbal supplements: Some herbs, such as cinnamon and fenugreek, may have potential benefits for blood sugar control. Cost: Varies depending on the specific supplement.
- Low-carbohydrate diet: Restricting carbohydrate intake can help improve blood sugar control. Cost: Varies depending on food choices.
Lifestyle Interventions
- Regular exercise: Engaging in physical activity can improve insulin sensitivity and help with weight management. Cost: Varies depending on the type of exercise (e.g., gym membership, equipment).
- Healthy diet: Following a balanced diet that includes whole grains, lean proteins, fruits, and vegetables can help control blood sugar levels. Cost: Varies depending on food choices.
- Weight loss: Losing weight can improve insulin sensitivity and blood sugar control. Cost: Varies depending on the method chosen (e.g., diet programs, weight loss clinics).
- Smoking cessation: Quitting smoking can reduce the risk of complications associated with diabetes. Cost: Varies depending on the method chosen (e.g., nicotine replacement therapy, counseling).
- Stress management: Managing stress levels through techniques such as meditation or therapy can help improve blood sugar control. Cost: Varies depending on the method chosen (e.g., therapy sessions, meditation apps).
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – T90 Diabetes non-insulin dependent (ICD-10:E11.9)
| Mild | Moderate | Severe |
| Mode setting: 2 (Wound Healing) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 4 (Diabetes Therapy) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 4 (Diabetes Therapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 4 (Diabetes Therapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting:7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting:7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Diabetes noninsulin dependent effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Diabetes noninsulin dependent. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- World Health Organization. (2021). Diabetes. Retrieved from https://www.who.int/news-room/fact-sheets/detail/diabetes
- Mayo Clinic. (2021). Type 2 diabetes – Symptoms and causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
- American Diabetes Association. (2021). Peripheral Neuropathy. Retrieved from https://www.diabetes.org/diabetes/complications/neuropathy/peripheral-neuropathy
- Centers for Disease Control and Prevention. (2021). Diabetes Risk Factors. Retrieved from https://www.cdc.gov/diabetes/basics/risk-factors.html
- National Institute of Diabetes and Digestive and Kidney Diseases. (2021). Risk Factors for Type 2 Diabetes. Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/risk-factors-type-2-diabetes
- American Diabetes Association. (2021). Standards of Medical Care in Diabetes—2021. Diabetes Care, 44(Supplement 1), S1-S232.
- Diabetes Canada Clinical Practice Guidelines Expert Committee. (2018). Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes, 42(Suppl 1), S1-S325.
- American Diabetes Association. (2021). Diagnosis. Retrieved from https://www.diabetes.org/a1c/diagnosis
- National Institute for Health and Care Excellence. (2020). Type 2 diabetes in adults: management. NICE guideline [NG28].
- Powers, M. A., Bardsley, J., Cypress, M., Duker, P., Funnell, M. M., Fischl, A. H., … & Vivian, E. (2017). Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. The Diabetes Educator, 43(1), 40-53.
Related articles
Made in USA