Introduction
Dehydration is a condition characterized by an inadequate amount of fluid in the body[1]. It occurs when the body loses more fluids than it takes in, leading to an imbalance in electrolytes and impairing normal bodily functions[2]. Dehydration can range from mild to severe and can have serious consequences if left untreated[3]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnostic steps, possible interventions, and patient education for dehydration.
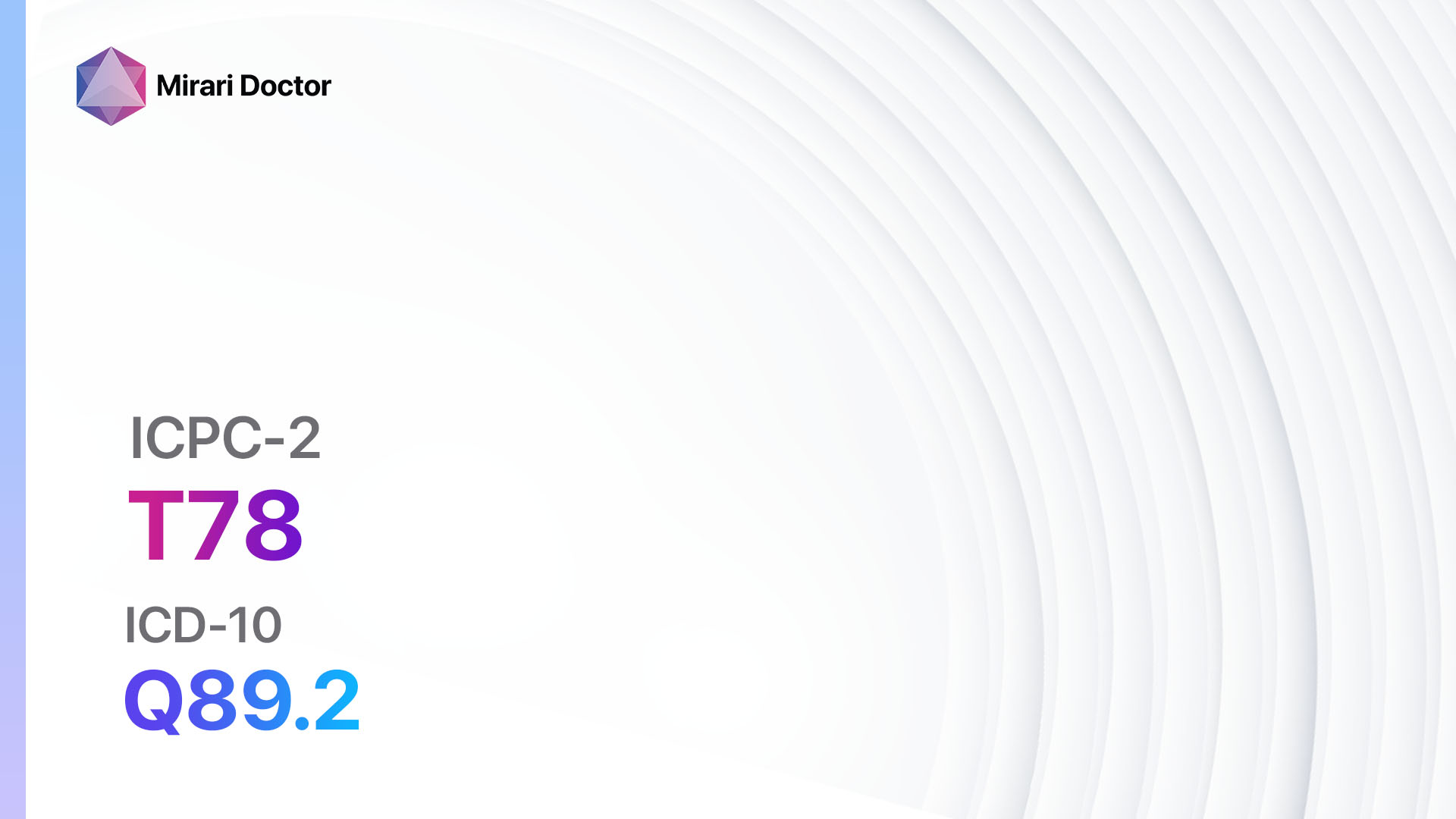
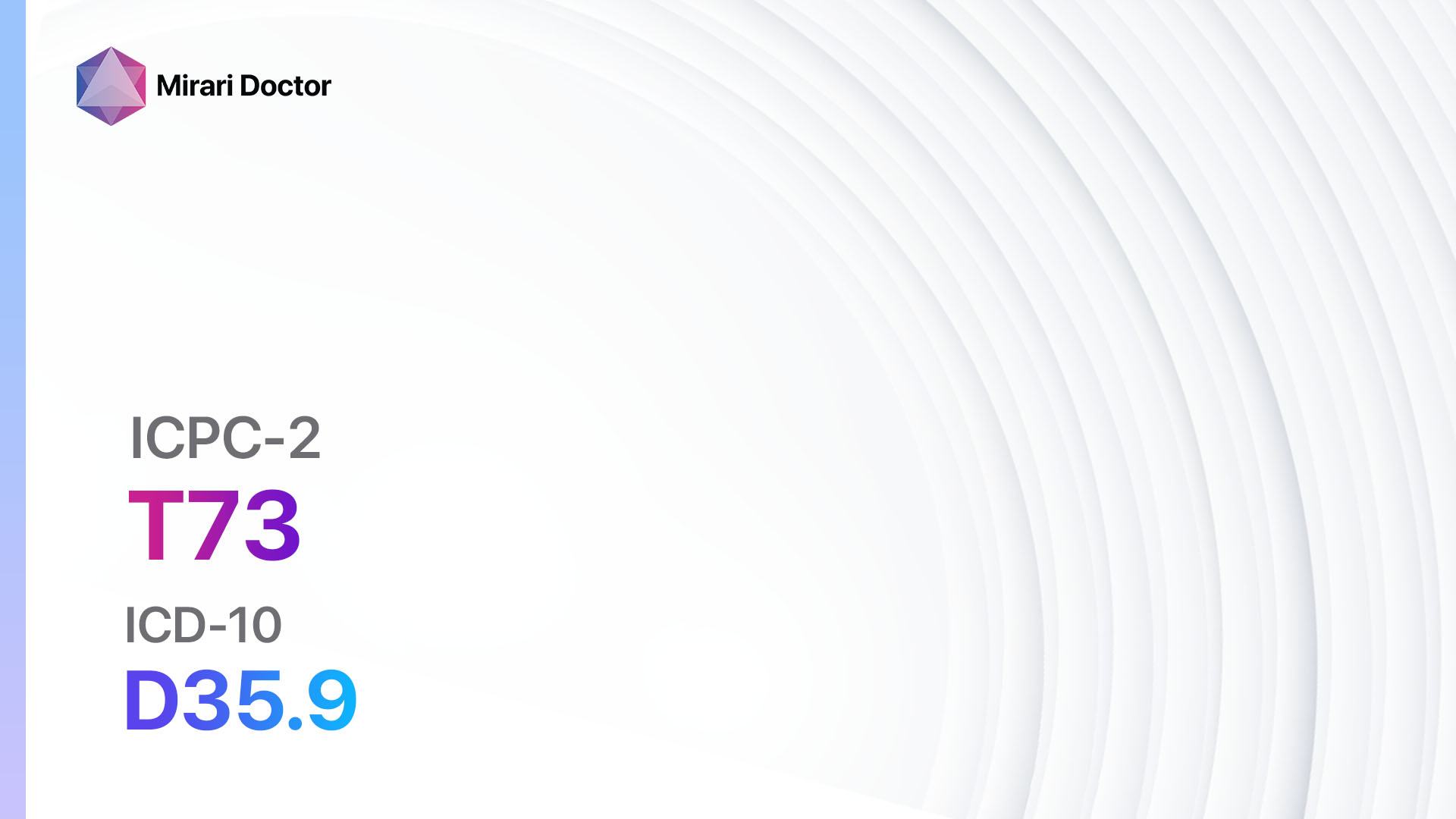
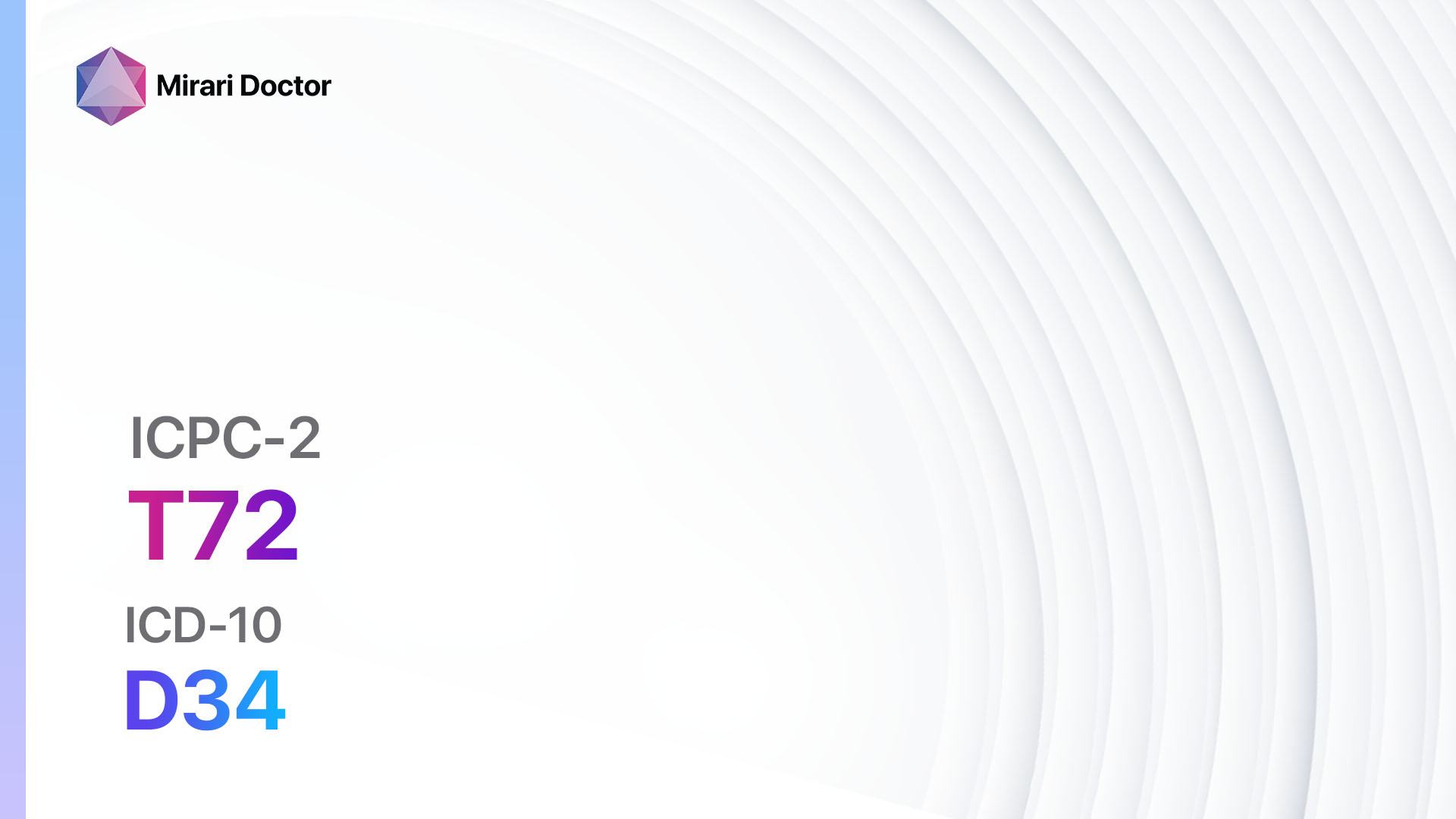
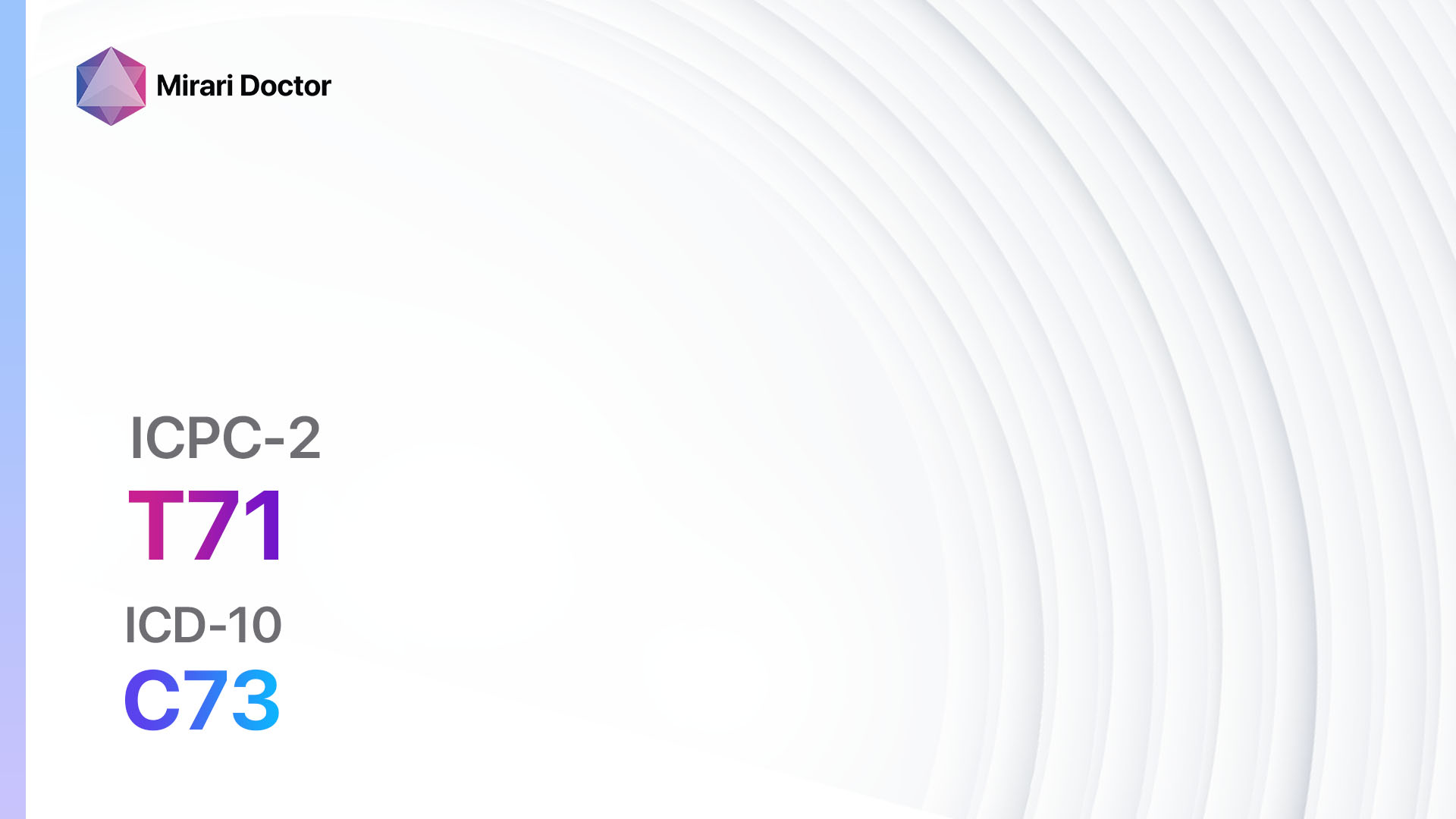
Codes
Symptoms
- Increased thirst
- Dry mouth and throat
- Fatigue or weakness
- Dizziness or lightheadedness
- Decreased urine output or dark-colored urine
- Dry skin
- Headache
- Muscle cramps
- Sunken eyes
- Rapid heartbeat[4]
Causes
- Inadequate fluid intake
- Excessive sweating
- Vomiting or diarrhea
- Fever
- Diabetes
- Kidney disease
- Medications that increase urine production (diuretics)
- Excessive alcohol consumption[5]
Diagnostic Steps
Medical History
- Gather information about the patient’s fluid intake habits, including the amount and frequency of water consumption.
- Inquire about any recent episodes of vomiting, diarrhea, or excessive sweating.
- Ask about any underlying medical conditions, such as diabetes or kidney disease.
- Determine if the patient is taking any medications that may contribute to dehydration[6].
Physical Examination
- Assess vital signs, including blood pressure, heart rate, and temperature.
- Check for signs of dehydration, such as dry mucous membranes, sunken eyes, and decreased skin turgor.
- Evaluate the patient’s mental status and level of consciousness.
- Examine the skin for signs of poor perfusion, such as coolness or pallor[7].
Laboratory Tests
- Complete blood count (CBC) to assess for changes in red blood cell count and electrolyte levels.
- Basic metabolic panel (BMP) to evaluate kidney function and electrolyte balance.
- Urinalysis to check for concentrated urine and signs of kidney dysfunction.
- Blood glucose level to rule out diabetes as a cause of dehydration[8].
Diagnostic Imaging
- In most cases, diagnostic imaging is not necessary for the diagnosis of dehydration. However, in severe cases or when an underlying condition is suspected, imaging modalities such as X-rays, ultrasound, CT scans, or MRIs may be used to assess organ function and identify potential causes of dehydration[9].
Other Tests
- In some cases, additional tests may be necessary based on the clinical presentation. These may include specialized laboratory tests to assess specific electrolyte imbalances or imaging studies to evaluate organ function[10].
Follow-up and Patient Education
- Provide the patient with information on the importance of adequate fluid intake and the signs and symptoms of dehydration.
- Advise the patient to seek medical attention if symptoms worsen or if they are unable to tolerate oral fluids.
- Schedule a follow-up appointment to monitor the patient’s hydration status and ensure appropriate treatment.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Dehydration:
- Oral rehydration solutions (e.g., Pedialyte):
- Cost: $5-$15 per bottle.
- Contraindications: None.
- Side effects: None.
- Severe side effects: None.
- Drug interactions: None.
- Warning: None.
- Intravenous (IV) fluids (e.g., Normal saline, Lactated Ringer’s solution):
- Cost: $50-$200 per bag.
- Contraindications: None.
- Side effects: None.
- Severe side effects: None.
- Drug interactions: None.
- Warning: Administration should be done under medical supervision.
- Antiemetics (e.g., Ondansetron, Metoclopramide):
- Cost: $10-$50 per prescription.
- Contraindications: Hypersensitivity.
- Side effects: Headache, constipation.
- Severe side effects: None.
- Drug interactions: None.
- Warning: Use with caution in patients with Parkinson’s disease.
- Antidiarrheal agents (e.g., Loperamide, Bismuth subsalicylate):
- Cost: $5-$20 per box.
- Contraindications: Severe abdominal pain, bloody stools.
- Side effects: Constipation, dizziness.
- Severe side effects: None.
- Drug interactions: None.
- Warning: Use with caution in patients with liver disease.
- Antipyretics (e.g., Acetaminophen, Ibuprofen):
- Cost: $5-$15 per bottle.
- Contraindications: Hypersensitivity, liver disease.
- Side effects: None.
- Severe side effects: None.
- Drug interactions: None.
- Warning: Follow recommended dosing guidelines.
Alternative Drugs:
- Probiotics: May help restore gut flora and improve digestion. Cost: $10-$30 per bottle.
- Electrolyte supplements: Can help replenish electrolytes lost through sweating or vomiting. Cost: $5-$20 per box.
- Anti-nausea herbal remedies: Ginger or peppermint supplements may help alleviate nausea. Cost: $5-$15 per bottle.
- Antidiarrheal herbal remedies: Chamomile or blackberry leaf tea may help reduce diarrhea. Cost: $5-$10 per box.
- Herbal diuretics: Dandelion or parsley supplements may help increase urine output. Cost: $5-$15 per bottle.
Surgical Procedures
- Surgical intervention is not typically required for the treatment of dehydration. However, in severe cases or when an underlying condition necessitates it, surgical procedures may be performed to address the underlying cause of dehydration.
Alternative Interventions
- Acupuncture: May help improve fluid balance and promote overall well-being. Cost: $60-$120 per session.
- Herbal remedies: Certain herbs, such as nettle leaf or corn silk, may have diuretic properties and help increase urine output. Cost: $5-$20 per bottle.
- Homeopathic remedies: Homeopathic preparations, such as Arnica or Bryonia, may help alleviate symptoms of dehydration. Cost: $5-$15 per bottle.
- Hydrotherapy: Soaking in a warm bath or using wet compresses may help rehydrate the body. Cost: None.
- Aromatherapy: Essential oils, such as lemon or peppermint, may help stimulate thirst and promote hydration. Cost: $5-$20 per bottle.
Lifestyle Interventions
- Increase fluid intake: Encourage the patient to drink water, herbal tea, or clear broths throughout the day.
- Avoid excessive alcohol and caffeine consumption, as they can contribute to dehydration.
- Eat hydrating foods, such as fruits and vegetables with high water content.
- Use a humidifier in dry environments to prevent excessive fluid loss through respiration.
- Dress appropriately for the weather and avoid prolonged exposure to extreme temperatures.
- Encourage regular exercise to promote circulation and maintain overall health.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – T11 Dehydration (ICD-10:E86)
| Mild | Moderate | Severe |
| Mode setting: 4 (Diabetes Therapy) Location: 4 (Heart, Bile & Pancreas) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 4 (Diabetes Therapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 4 (Diabetes Therapy) Location: 4 (Heart, Bile & Pancreas) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 6 (Throat, Lymphatic & Thyroid) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Dehydration effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Dehydration. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Shaheen, N. A., Alqahtani, A. A., Assiri, H., Alkhodair, R., & Hussein, M. A. (2018). Public knowledge of dehydration and fluid intake practices: variation by participants’ characteristics. BMC Public Health, 18(1), 1346.
- Popkin, B. M., D’Anci, K. E., & Rosenberg, I. H. (2010). Water, hydration, and health. Nutrition Reviews, 68(8), 439-458.
- Hooper, L., Abdelhamid, A., Attreed, N. J., Campbell, W. W., Channell, A. M., Chassagne, P., … & Hunter, P. (2015). Clinical symptoms, signs and tests for identification of impending and current water‐loss dehydration in older people. Cochrane Database of Systematic Reviews, (4).
- Kenefick, R. W., & Sawka, M. N. (2007). Hydration at the work site. Journal of the American College of Nutrition, 26(sup5), 597S-603S.
- Maughan, R. J. (2003). Impact of mild dehydration on wellness and on exercise performance. European Journal of Clinical Nutrition, 57(2), S19-S23.
- Thomas, D. R., Cote, T. R., Lawhorne, L., Levenson, S. A., Rubenstein, L. Z., Smith, D. A., … & Dehydration Council. (2008). Understanding clinical dehydration and its treatment. Journal of the American Medical Directors Association, 9(5), 292-301.
- Fortes, M. B., Owen, J. A., Raymond-Barker, P., Bishop, C., Elghenzai, S., Oliver, S. J., & Walsh, N. P. (2015). Is this elderly patient dehydrated? Diagnostic accuracy of hydration assessment using physical signs, urine, and saliva markers. Journal of the American Medical Directors Association, 16(3), 221-228.
- Cheuvront, S. N., Kenefick, R. W., Charkoudian, N., & Sawka, M. N. (2013). Physiologic basis for understanding quantitative dehydration assessment. The American Journal of Clinical Nutrition, 97(3), 455-462.
- Becker, G. J., & Garigali, G. (2016). Ultrasound and imaging techniques to diagnose and evaluate cholecystitis. Vinmec International Hospital.
- Sterns, R. H. (2015). Disorders of plasma sodium—causes, consequences, and correction. New England Journal of Medicine, 372(1), 55-65.
Related articles
Made in USA