Introduction
Deafness, also known as hearing loss, is a condition characterized by the partial or complete inability to hear. It can significantly impact an individual’s quality of life, communication abilities, and social interactions[1]. The aim of this guide is to provide healthcare professionals with a comprehensive overview of the diagnostic steps, possible interventions, and patient education strategies for managing deafness.
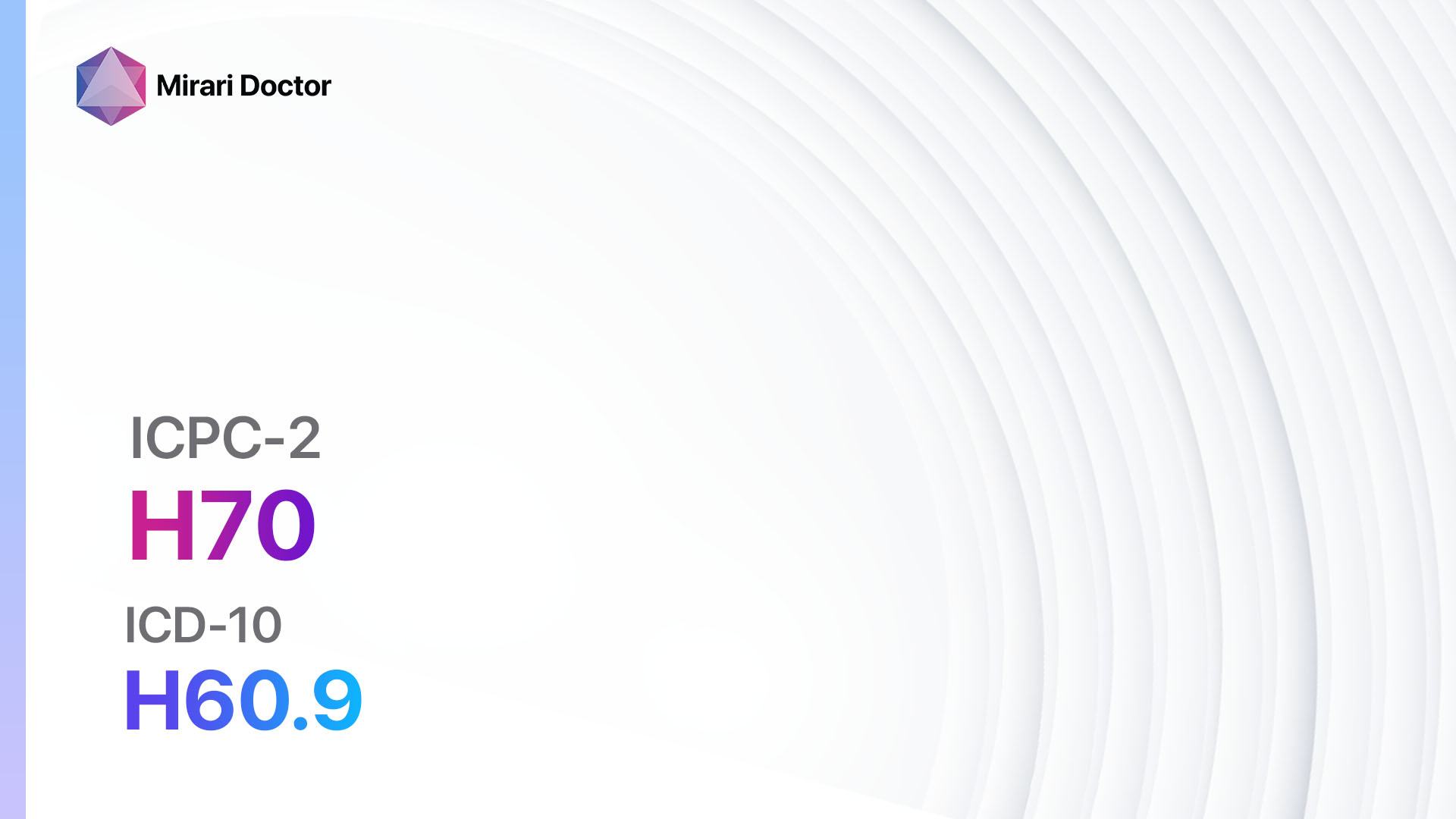
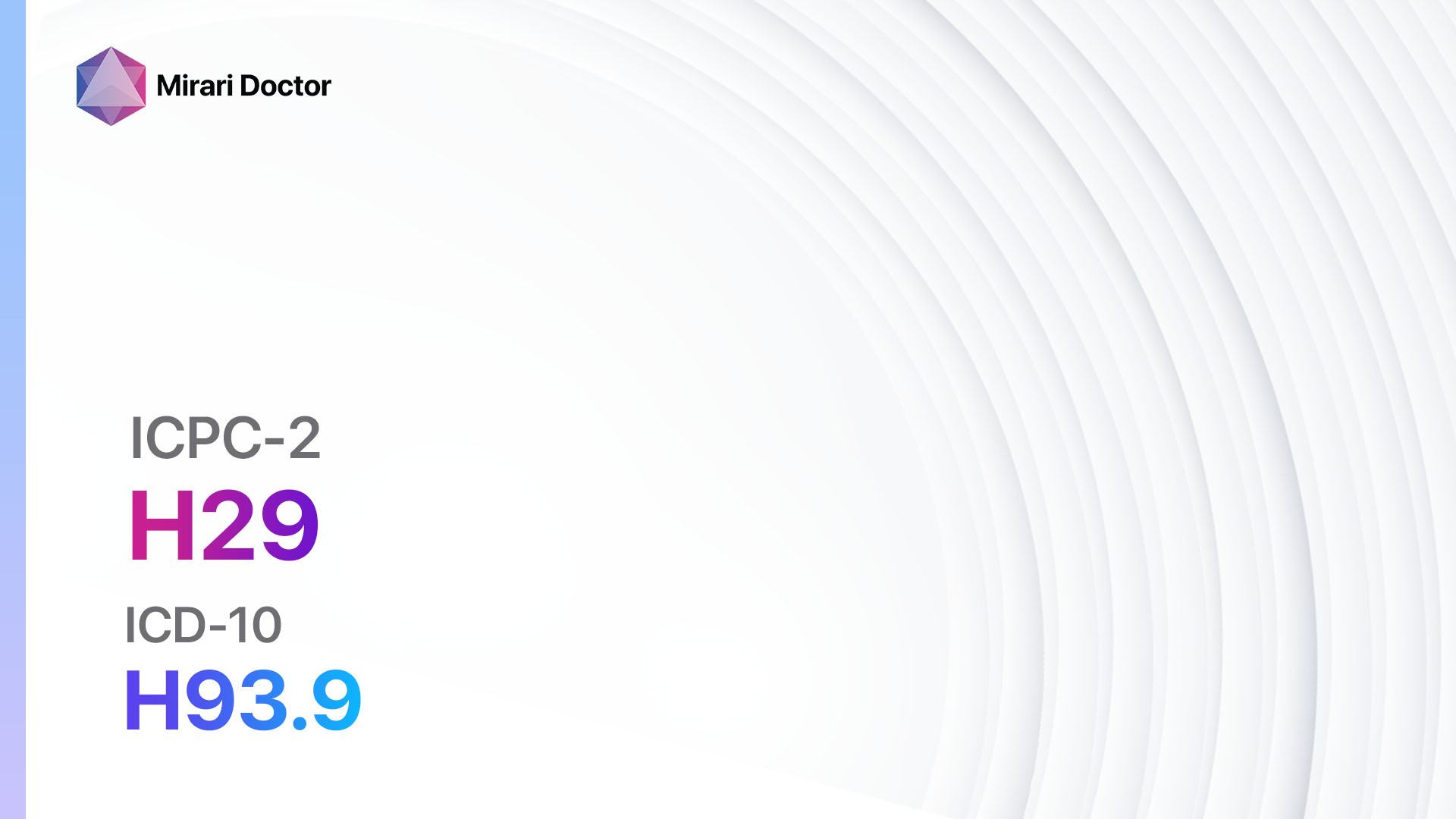
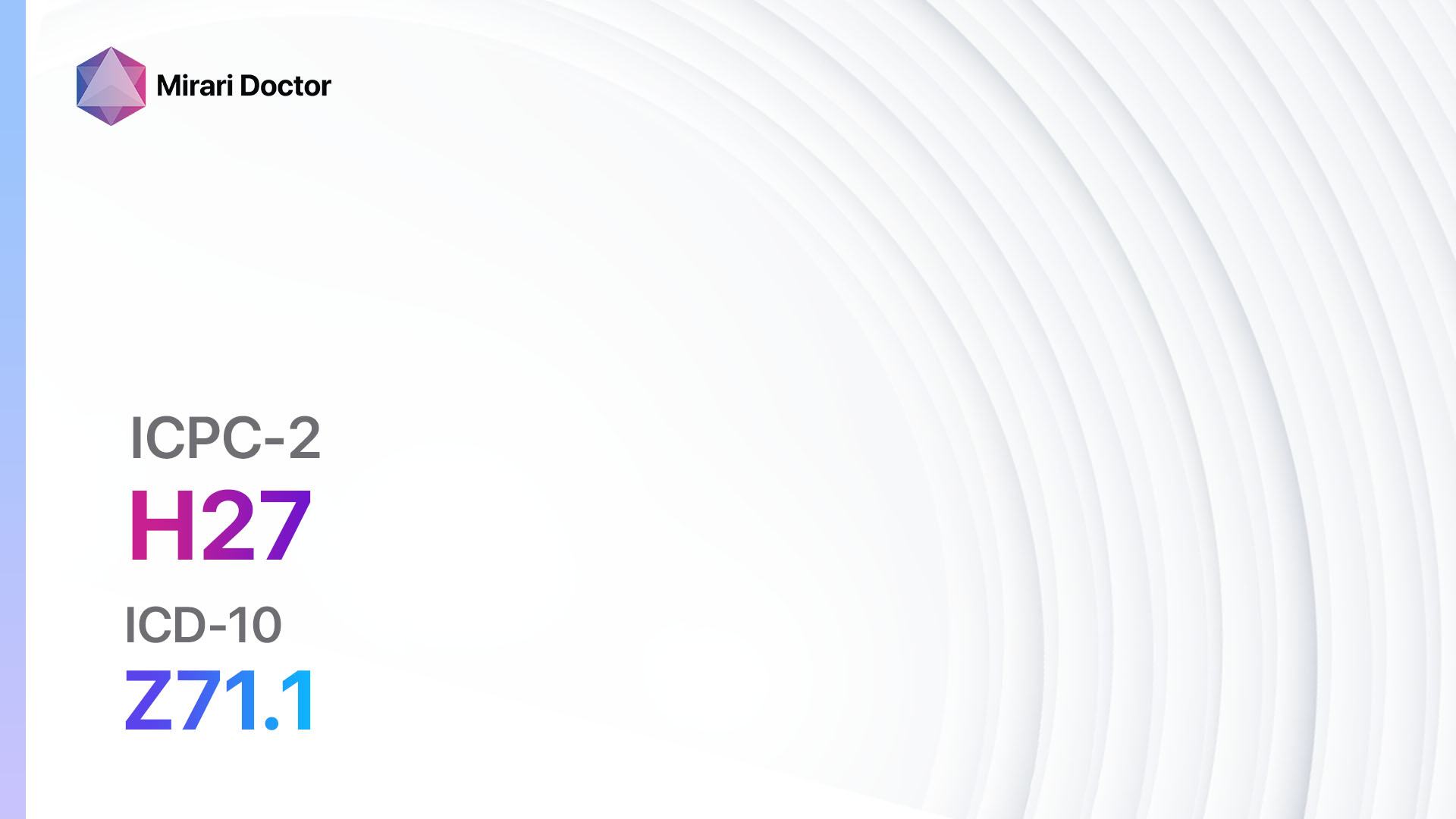
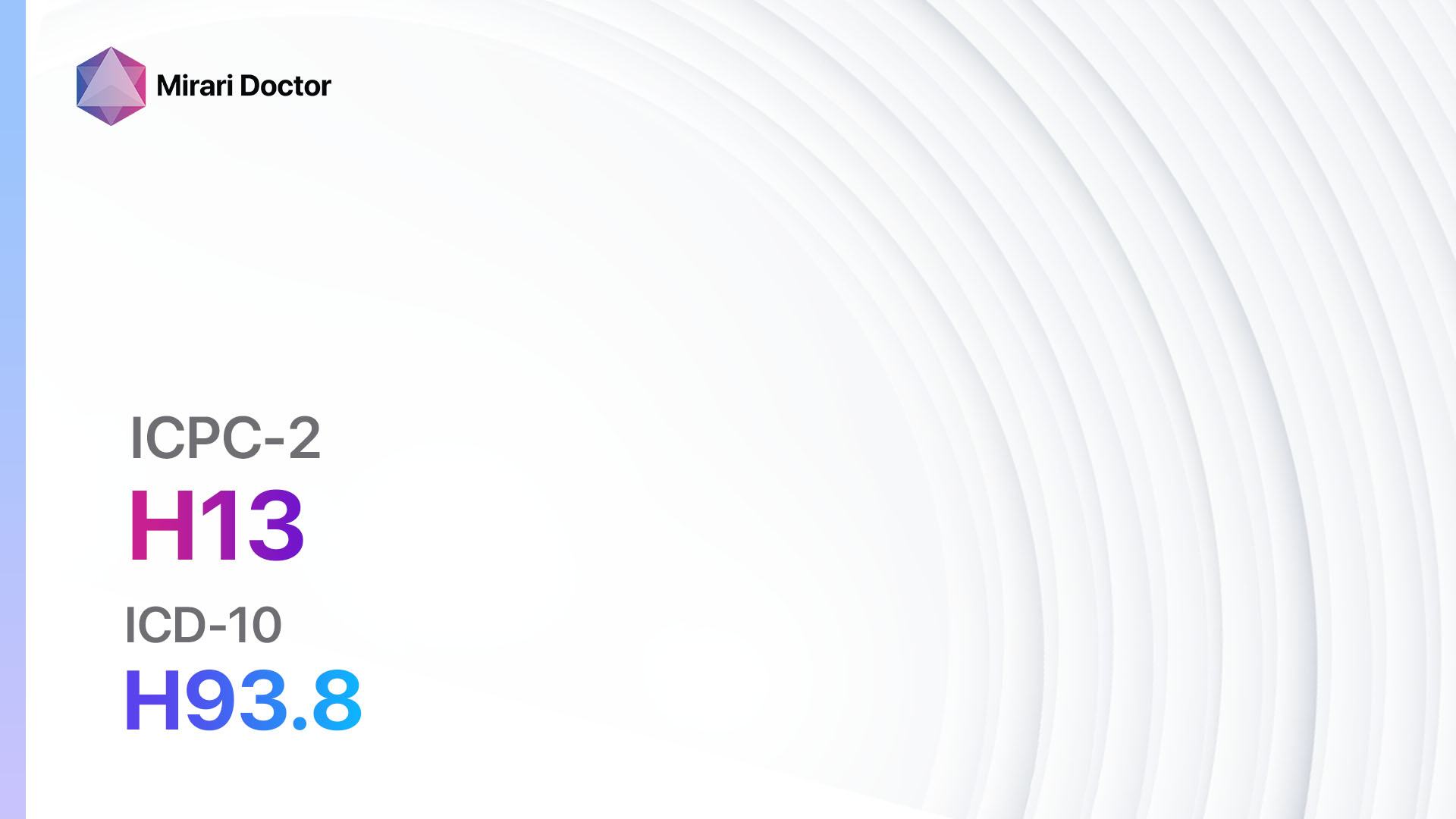
Codes
Symptoms
- Difficulty understanding speech or conversations[4]
- Inability to hear sounds or voices
- Ringing or buzzing sensation in the ears (tinnitus)[5]
- Sensation of pressure or fullness in the ears
- Difficulty hearing in noisy environments
- Withdrawal from social interactions due to communication difficulties
Causes
- Age-related hearing loss (presbycusis)[6]
- Exposure to loud noises[7]
- Genetics and family history[8]
- Ear infections or diseases
- Trauma or injury to the ear
- Certain medications that can cause hearing loss (ototoxic drugs)[9]
- Medical conditions such as diabetes, high blood pressure, or autoimmune disorders[10]
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the onset, duration, and progression of hearing loss.
- Identify any risk factors, such as exposure to loud noises, family history of hearing loss, or underlying medical conditions.
- Inquire about any previous ear infections, trauma, or use of ototoxic medications.
- Assess the impact of hearing loss on the patient’s daily life and communication abilities.
Physical Examination
- Inspect the external ear for any abnormalities, such as deformities or signs of infection.
- Evaluate the ear canal and eardrum using an otoscope to check for blockages, inflammation, or perforations.
- Perform a tuning fork test to assess the patient’s ability to hear different frequencies.
- Conduct a whisper test or speech audiometry to determine the patient’s hearing threshold.
Laboratory Tests
- Pure-tone audiometry: Measures the patient’s hearing sensitivity at different frequencies.
- Speech audiometry: Assesses the patient’s ability to understand speech at different volumes.
- Tympanometry: Measures the movement of the eardrum in response to changes in air pressure, helping to identify middle ear problems.
- Blood tests: May be ordered to check for underlying medical conditions that could contribute to hearing loss, such as diabetes or autoimmune disorders.
Diagnostic Imaging
- CT scan or MRI: Used to visualize the structures of the inner ear and identify any abnormalities or tumors that may be causing hearing loss.
- X-rays: Can help identify bony abnormalities or fractures in the skull or ear.
Other Tests
- Otoacoustic emissions (OAE) test: Measures the sounds emitted by the inner ear in response to a stimulus, helping to assess the function of the cochlea.
- Auditory brainstem response (ABR) test: Evaluates the electrical activity of the auditory nerve and brainstem in response to sound stimuli, useful in diagnosing nerve-related hearing loss.
- Genetic testing: May be recommended in cases where a genetic cause of hearing loss is suspected.
Follow-up and Patient Education
- Schedule regular follow-up appointments to monitor the progression of hearing loss and adjust interventions as needed.
- Provide patient education on strategies for managing hearing loss, such as using assistive devices, lip reading, and communication techniques.
- Discuss the importance of protecting the ears from loud noises and avoiding ototoxic medications.
- Refer patients to support groups or counseling services to address the emotional and psychological impact of hearing loss.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Deafness:
- Corticosteroids (e.g., Prednisone, Dexamethasone):
- Cost: Generic versions can range from $10 to $50 for a month’s supply.
- Contraindications: Active infections, systemic fungal infections.
- Side effects: Increased appetite, weight gain, mood changes.
- Severe side effects: Increased risk of infections, osteoporosis, adrenal suppression.
- Drug interactions: Nonsteroidal anti-inflammatory drugs (NSAIDs), anticoagulants.
- Warning: Prolonged use may require gradual tapering to avoid adrenal insufficiency.
- Antibiotics (e.g., Amoxicillin, Ciprofloxacin):
- Cost: Generic versions can range from $10 to $50 for a course of treatment.
- Contraindications: Allergy to antibiotics, history of tendon disorders.
- Side effects: Upset stomach, diarrhea, rash.
- Severe side effects: Severe allergic reactions, tendon rupture.
- Drug interactions: Antacids, blood thinners.
- Warning: Complete the full course of antibiotics as prescribed.
- Diuretics (e.g., Furosemide, Hydrochlorothiazide):
- Cost: Generic versions can range from $10 to $30 for a month’s supply.
- Contraindications: Allergy to diuretics, severe electrolyte imbalances.
- Side effects: Increased urination, electrolyte imbalances.
- Severe side effects: Dehydration, low blood pressure.
- Drug interactions: Nonsteroidal anti-inflammatory drugs (NSAIDs), lithium.
- Warning: Monitor electrolyte levels regularly.
- Antiviral medications (e.g., Acyclovir, Valacyclovir):
- Cost: Generic versions can range from $10 to $50 for a course of treatment.
- Contraindications: Allergy to antiviral medications, severe kidney disease.
- Side effects: Nausea, headache, dizziness.
- Severe side effects: Severe allergic reactions, kidney damage.
- Drug interactions: Probenecid, other antiviral medications.
- Warning: Start treatment as early as possible for viral-related hearing loss.
- Vasodilators (e.g., Betahistine, Cinnarizine):
- Cost: Generic versions can range from $10 to $30 for a month’s supply.
- Contraindications: Allergy to vasodilators, low blood pressure.
- Side effects: Upset stomach, dizziness, headache.
- Severe side effects: Severe allergic reactions, rapid heartbeat.
- Drug interactions: Antihypertensive medications, anticoagulants.
- Warning: Monitor blood pressure regularly.
Alternative Drugs:
- Ginkgo biloba: An herbal supplement that may improve blood flow to the inner ear. Cost: $10-$30 for a month’s supply.
- Vitamin B12: May help improve nerve function and reduce the risk of hearing loss. Cost: $5-$20 for a month’s supply.
- Magnesium: Some studies suggest that magnesium supplementation may have a protective effect on hearing. Cost: $5-$15 for a month’s supply.
- N-acetylcysteine: An antioxidant that may help reduce oxidative stress in the inner ear. Cost: $10-$30 for a month’s supply.
- Alpha-lipoic acid: May have antioxidant properties and protect against age-related hearing loss. Cost: $10-$30 for a month’s supply.
Surgical Procedures:
- Cochlear implant: A surgically implanted device that bypasses damaged parts of the inner ear and stimulates the auditory nerve. Cost: $50,000 to $100,000.
- Middle ear implant: A surgically implanted device that amplifies sound vibrations and transmits them to the middle ear. Cost: $20,000 to $40,000.
- Bone-anchored hearing aid (BAHA): A surgically implanted device that transmits sound vibrations through the skull bone to the inner ear. Cost: $10,000 to $20,000.
Alternative Interventions
- Acupuncture: May help improve blood flow and reduce tinnitus. Cost: $60-$120 per session.
- Chiropractic care: Some individuals report improvements in hearing and tinnitus with chiropractic adjustments. Cost: $50-$100 per session.
- Hyperbaric oxygen therapy: Involves breathing pure oxygen in a pressurized chamber to increase oxygen delivery to tissues. Cost: $200-$300 per session.
- Herbal supplements: Some herbs, such as ginkgo biloba and ginger, may have potential benefits for improving circulation and reducing tinnitus. Cost: Varies depending on the specific supplement.
- Sound therapy: Involves the use of white noise or other soothing sounds to mask tinnitus and improve relaxation. Cost: Varies depending on the specific sound therapy device or app.
Lifestyle Interventions
- Hearing aids: Amplify sounds and improve hearing for individuals with mild to moderate hearing loss. Cost: $1,000 to $6,000 per hearing aid.
- Assistive listening devices: Devices such as personal amplifiers or FM systems can help individuals hear better in specific situations, such as in noisy environments or during conversations. Cost: $100 to $500.
- Communication techniques: Educate patients on strategies such as lip reading, sign language, and visual cues to enhance communication.
- Avoidance of loud noises: Encourage patients to protect their ears from excessive noise exposure by using earplugs or earmuffs in noisy environments.
- Regular exercise and healthy lifestyle: Maintaining overall health and managing underlying medical conditions can help prevent further hearing loss.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – H86 Deafness (ICD-10:H91.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 45 minutes approx. $7.50 USD, Evening: 45 minutes approx. $7.50 USD |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
Total Morning: 90 minutes approx. $15 USD, Lunch: 90 minutes approx. $15 USD, Evening: 90 minutes approx. $15 USD, |
| Usual treatment for 7-60 days approx. $105 USD – $900 USD | Usual treatment for 6-8 weeks approx. $1,890 USD – $2,520 USD |
Usual treatment for 3-6 months approx. $4,050 USD – $8,100 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Deafness effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Deafness. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Olusanya, B. O., Davis, A. C., & Hoffman, H. J. (2019). Hearing loss: rising prevalence and impact. Bulletin of the World Health Organization, 97(10), 646–646A. https://doi.org/10.2471/BLT.19.224683
- World Organization of Family Doctors (WONCA). (n.d.). ICPC-2 – English. Retrieved June 19, 2024, from https://www.globalfamilydoctor.com/site/DefaultSite/filesystem/documents/Groups/WICC/International%20Classification%20of%20Primary%20Care%20Dec16.pdf
- World Health Organization. (2019). ICD-10 Version:2019. Retrieved June 19, 2024, from https://icd.who.int/browse10/2019/en#/H90-H95
- Cunningham, L. L., & Tucci, D. L. (2017). Hearing Loss in Adults. New England Journal of Medicine, 377(25), 2465–2473. https://doi.org/10.1056/nejmra1616601
- Baguley, D., McFerran, D., & Hall, D. (2013). Tinnitus. The Lancet, 382(9904), 1600–1607. https://doi.org/10.1016/s0140-6736(13)60142-7
- Gates, G. A., & Mills, J. H. (2005). Presbycusis. The Lancet, 366(9491), 1111–1120. https://doi.org/10.1016/s0140-6736(05)67423-5
- Basner, M., Babisch, W., Davis, A., Brink, M., Clark, C., Janssen, S., & Stansfeld, S. (2014). Auditory and non-auditory effects of noise on health. The Lancet, 383(9925), 1325–1332. https://doi.org/10.1016/s0140-6736(13)61613-x
- Shearer, A. E., Hildebrand, M. S., & Smith, R. J. H. (2017). Hereditary Hearing Loss and Deafness Overview. GeneReviews®. Retrieved June 19, 2024, from https://www.ncbi.nlm.nih.gov/books/NBK1434/
- Cianfrone, G., Pentangelo, D., Cianfrone, F., Mazzei, F., Turchetta, R., Orlando, M. P., & Altissimi, G. (2011). Pharmacological drugs inducing ototoxicity, vestibular symptoms and tinnitus: a reasoned and updated guide. European Review for Medical and Pharmacological Sciences, 15(6), 601–636.
- Bainbridge, K. E., Hoffman, H. J., & Cowie, C. C. (2008). Diabetes and Hearing Impairment in the United States: Audiometric Evidence from the National Health and Nutrition Examination Survey, 1999 to 2004. Annals of Internal Medicine, 149(1), 1. https://doi.org/10.7326/0003-4819-149-1-200807010-00231
Related articles
Made in USA