Introduction
Abdominal distension refers to the swelling or enlargement of the abdomen, often accompanied by discomfort or pain. It can be caused by various factors, including gastrointestinal issues, fluid accumulation, or underlying medical conditions. This guide aims to provide an overview of the symptoms, causes, diagnostic steps, possible interventions, and lifestyle modifications for managing abdominal distension.[1][2]
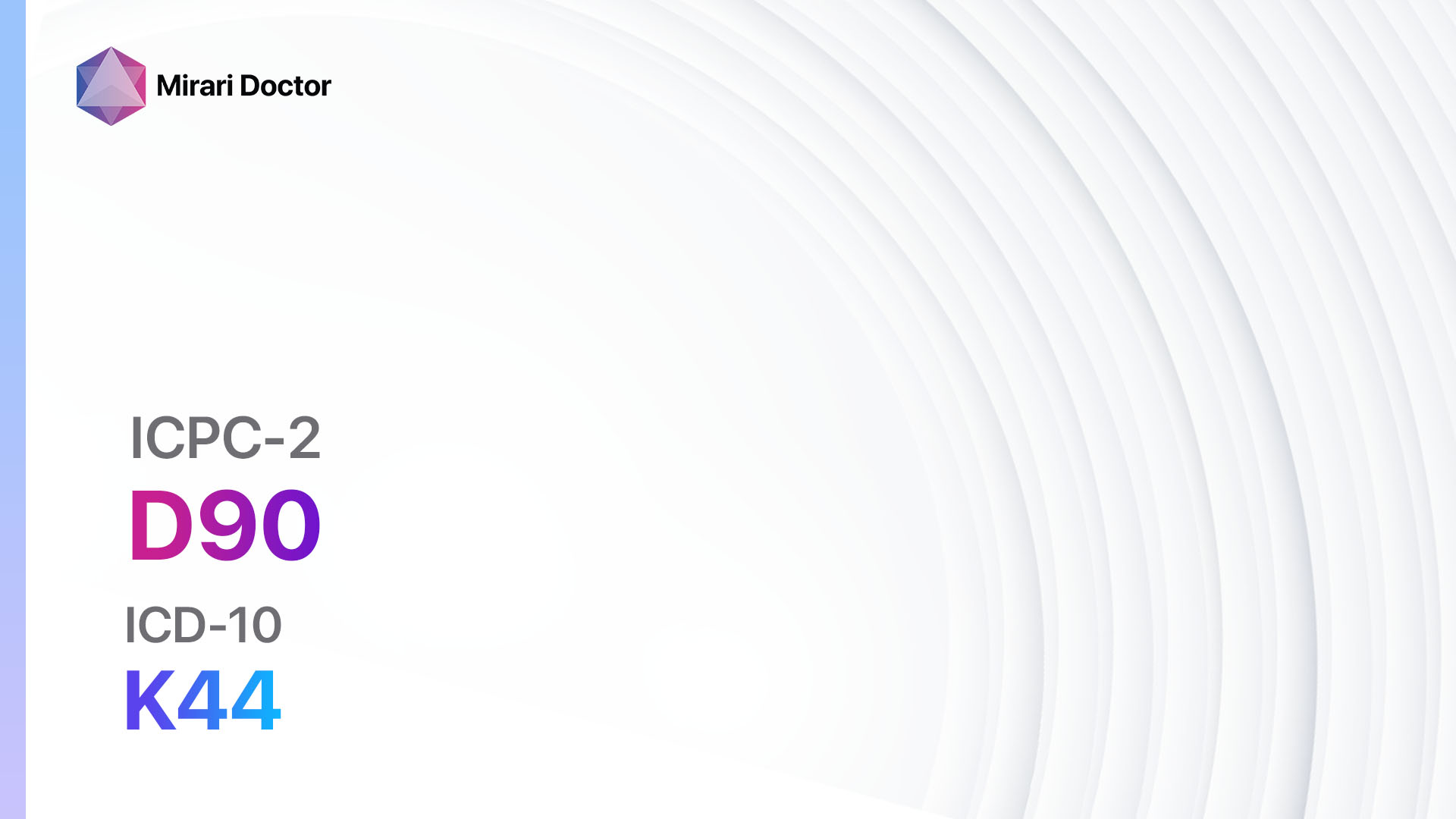
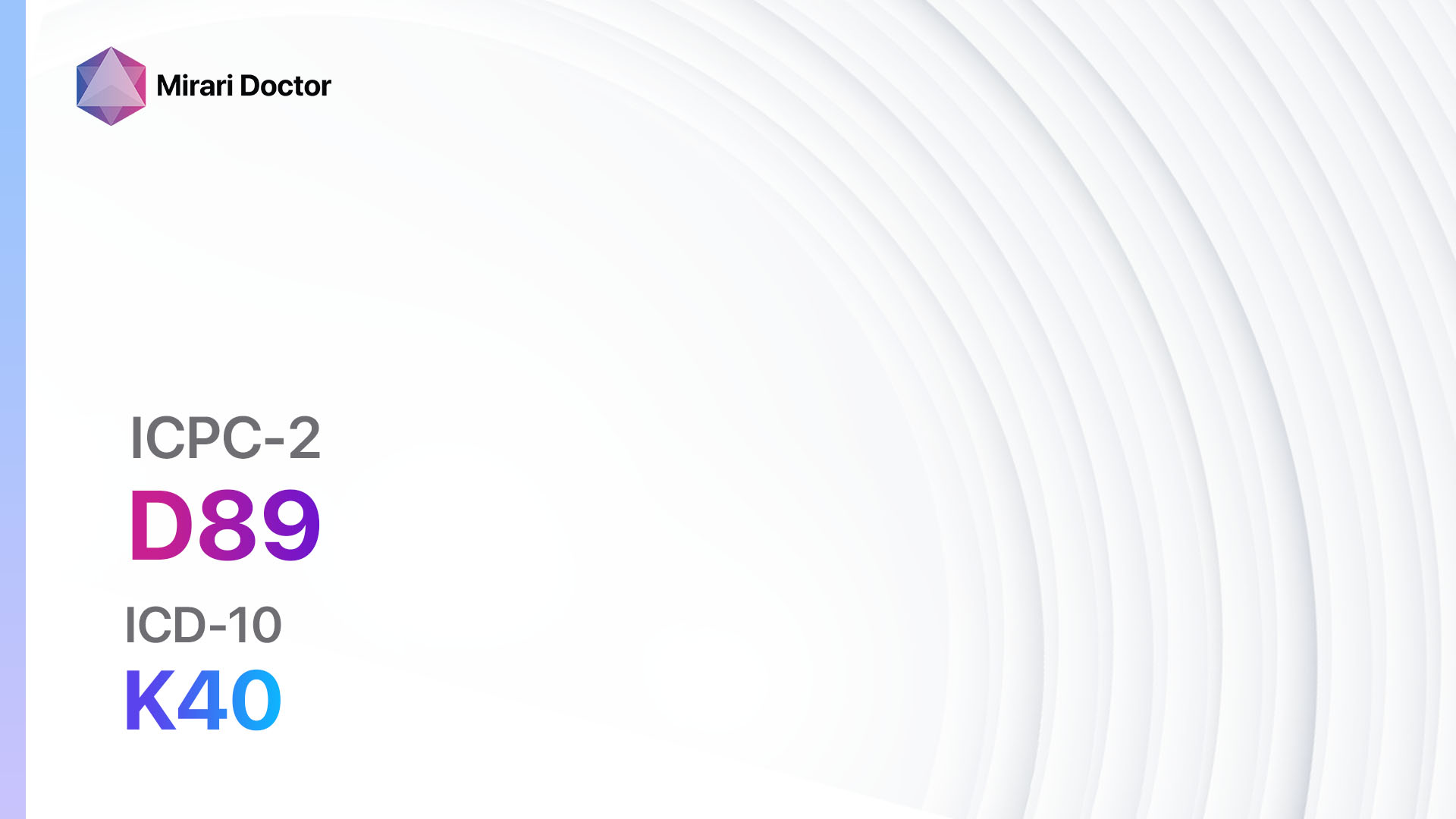
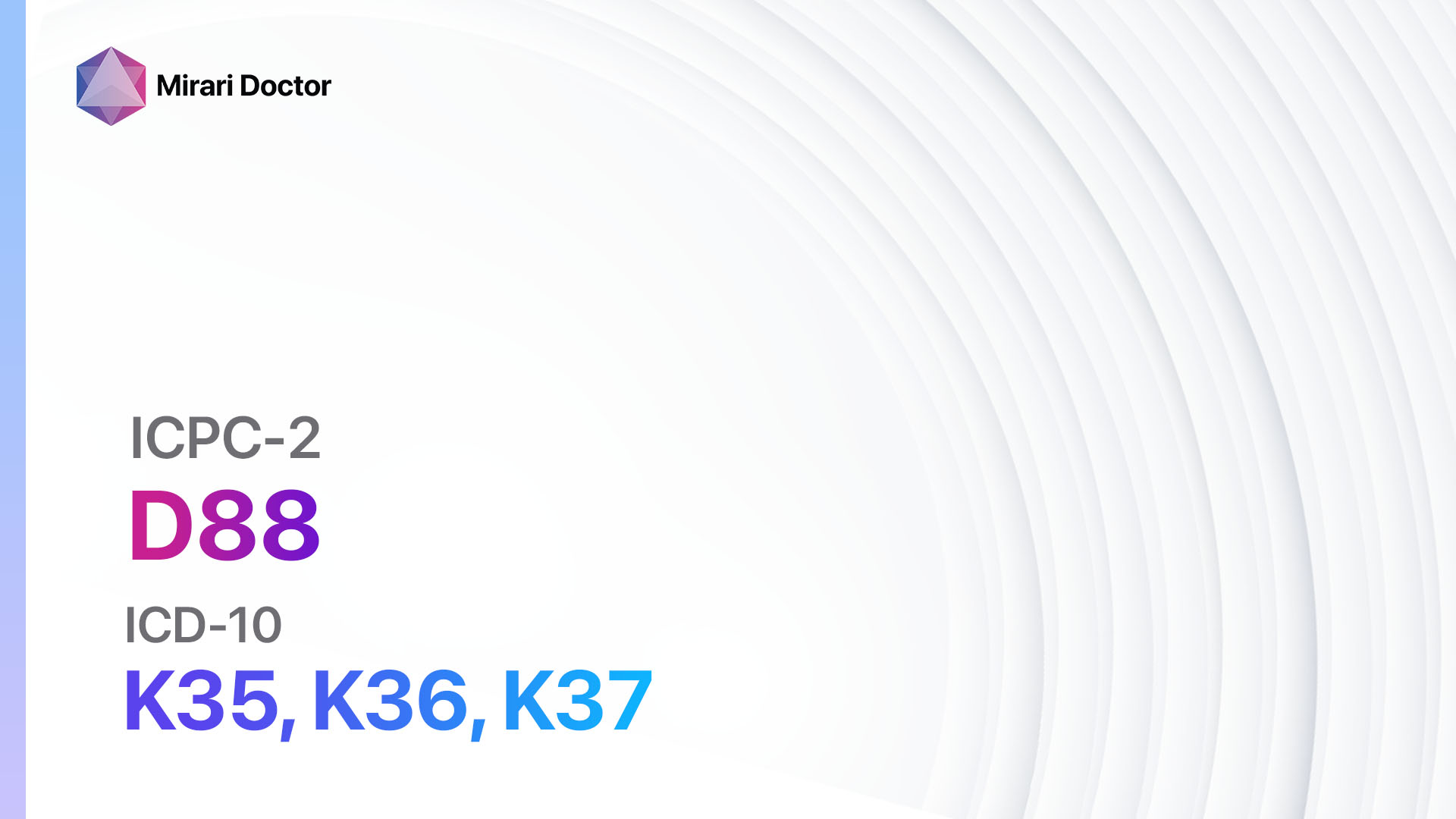
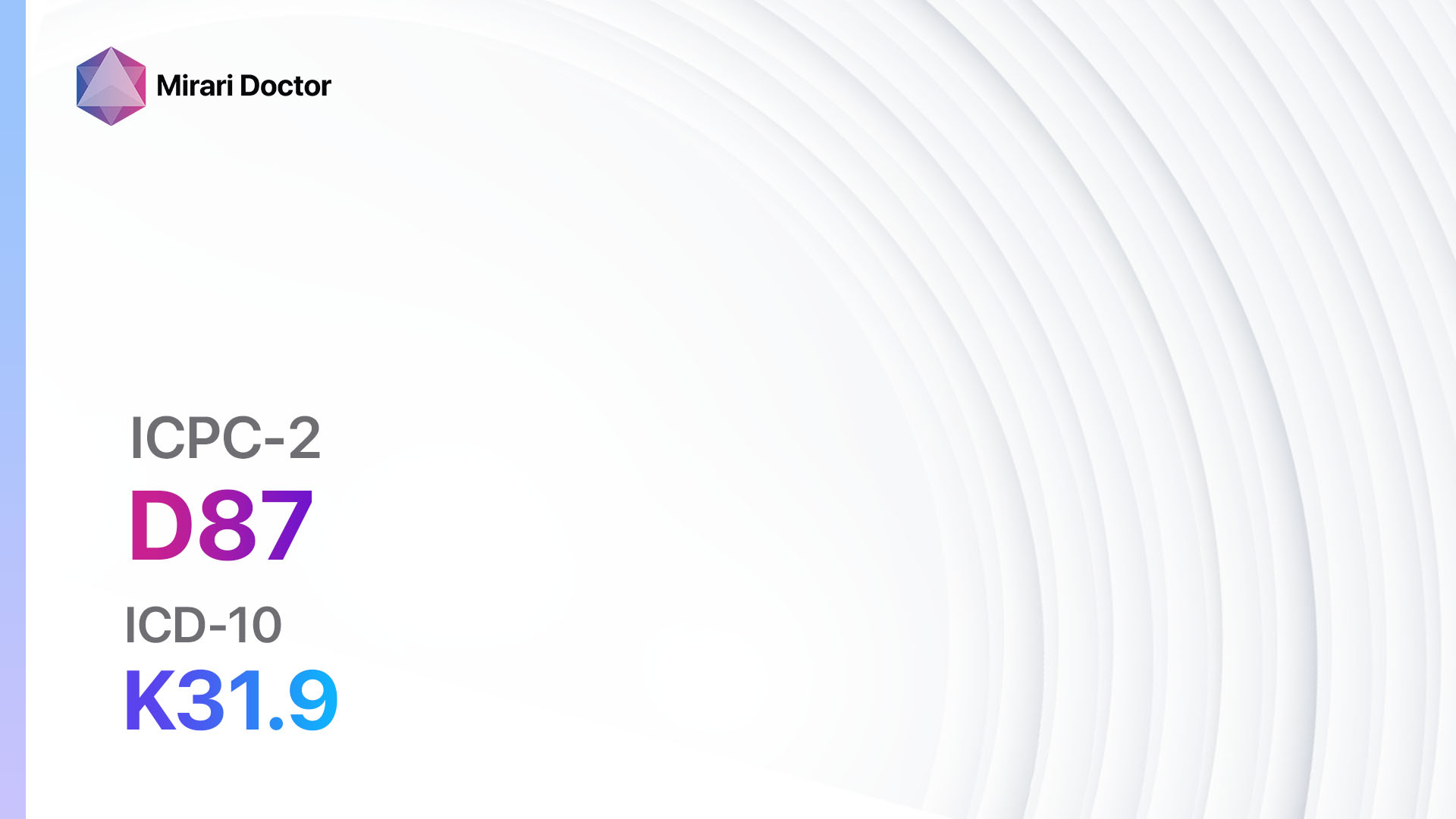
Codes
Symptoms
- Abdominal bloating: Feeling of fullness or tightness in the abdomen.[5]
- Increased abdominal girth: Noticeable increase in the size of the abdomen.[6]
- Abdominal discomfort or pain: Dull or sharp pain in the abdominal region.[7]
- Flatulence: Excessive gas production and release.[8]
- Constipation: Difficulty in passing stools or infrequent bowel movements.[9]
- Nausea and vomiting: Feeling of queasiness and the urge to vomit.[10]
Causes
- Gastrointestinal issues: Conditions such as irritable bowel syndrome (IBS), constipation, or intestinal obstruction can lead to abdominal distension.
- Fluid accumulation: Ascites, a condition characterized by the accumulation of fluid in the abdominal cavity, can cause distension.
- Overeating: Consuming large meals or eating too quickly can result in temporary abdominal distension.
- Food intolerances: Certain foods, such as lactose or gluten, can cause bloating and distension in individuals with intolerances.
- Medical conditions: Conditions like ovarian cysts, uterine fibroids, or tumors can contribute to abdominal distension.
Diagnostic Steps
Medical History
- Gather information about the patient’s symptoms, including the duration and severity of abdominal distension.
- Identify any risk factors, such as a history of gastrointestinal disorders or previous surgeries.
- Inquire about the presence of other symptoms, such as changes in bowel habits or weight loss.
Physical Examination
- Perform a thorough abdominal examination, assessing for distension, tenderness, or abnormal masses.
- Check for signs of fluid accumulation, such as shifting dullness or a fluid wave.
- Evaluate other vital signs, including blood pressure, heart rate, and respiratory rate.
Laboratory Tests
- Complete blood count (CBC): Assess for signs of infection or anemia.
- Liver function tests: Evaluate liver health and rule out liver disease as a cause of abdominal distension.
- Electrolyte panel: Check for imbalances that may contribute to fluid retention.
- Celiac disease panel: Screen for gluten intolerance or celiac disease.
- Stool tests: Rule out infections or malabsorption issues.
Diagnostic Imaging
- Abdominal X-ray: Assess for signs of bowel obstruction or abnormal gas patterns.
- Abdominal ultrasound: Visualize the abdominal organs, including the liver, gallbladder, and kidneys.
- CT scan: Provide detailed images of the abdominal structures, aiding in the diagnosis of tumors or other abnormalities.
- MRI: Offer a more detailed assessment of the abdominal organs, particularly useful for evaluating soft tissue structures.
Other Tests
- Endoscopy: Insert a flexible tube with a camera into the digestive tract to visualize the esophagus, stomach, and small intestine.
- Colonoscopy: Examine the colon and rectum for abnormalities or signs of inflammation.
- Pelvic ultrasound: Assess the reproductive organs in females, checking for conditions like ovarian cysts or uterine fibroids.
Follow-up and Patient Education
- Schedule follow-up appointments to monitor the effectiveness of interventions and address any concerns or new symptoms.
- Provide education on lifestyle modifications, including dietary changes and stress management techniques.
- Encourage patients to seek medical attention if symptoms worsen or new symptoms develop.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for Abdominal Distension:
- Simethicone (e.g., Gas-X, Mylicon):
- Cost: $5-$15 for a bottle of 60-100 tablets.
- Contraindications: Hypersensitivity to simethicone.
- Side effects: Rare, but may include diarrhea or skin rash.
- Severe side effects: None reported.
- Drug interactions: No significant drug interactions.
- Warning: Safe for use in infants, children, and adults.
- Laxatives (e.g., Polyethylene glycol, Senna):
- Cost: $5-$20 for a bottle of 30-100 tablets.
- Contraindications: Intestinal obstruction, fecal impaction, or hypersensitivity to the specific laxative.
- Side effects: Abdominal cramping, diarrhea, or electrolyte imbalances.
- Severe side effects: None reported with short-term use.
- Drug interactions: Some laxatives may interact with other medications, such as diuretics or anticoagulants.
- Warning: Prolonged or excessive use of laxatives can lead to dependence or electrolyte abnormalities.
- Prokinetic agents (e.g., Metoclopramide, Domperidone):
- Cost: $10-$30 for a bottle of 30-60 tablets.
- Contraindications: Gastrointestinal bleeding, mechanical obstruction, or hypersensitivity to the specific prokinetic agent.
- Side effects: Restlessness, drowsiness, or extrapyramidal symptoms (with metoclopramide).
- Severe side effects: Tardive dyskinesia (rare, with long-term use of metoclopramide).
- Drug interactions: Some prokinetic agents may interact with other medications, such as antipsychotics or opioids.
- Warning: Metoclopramide should not be used for more than 12 weeks due to the risk of tardive dyskinesia.
- Antispasmodics (e.g., Dicyclomine, Hyoscyamine):
- Cost: $10-$30 for a bottle of 30-60 tablets.
- Contraindications: Glaucoma, myasthenia gravis, or hypersensitivity to the specific antispasmodic.
- Side effects: Dry mouth, blurred vision, or constipation.
- Severe side effects: None reported.
- Drug interactions: Some antispasmodics may interact with other medications, such as anticholinergics or opioids.
- Warning: Use with caution in elderly patients due to the risk of cognitive impairment.
- Probiotics (e.g., Lactobacillus, Bifidobacterium):
- Cost: $10-$30 for a bottle of 30-60 capsules.
- Contraindications: Hypersensitivity to the specific probiotic strain.
- Side effects: Rare, but may include bloating or gas.
- Severe side effects: None reported.
- Drug interactions: No significant drug interactions.
- Warning: Probiotics may not be suitable for individuals with compromised immune systems.
Alternative Drugs:
- Peppermint oil: May help relax the muscles of the gastrointestinal tract. Cost: $10-$20 for a bottle of 60-90 capsules.
- Activated charcoal: Can help absorb excess gas in the digestive system. Cost: $10-$20 for a bottle of 60-100 capsules.
- Digestive enzymes: Aid in the breakdown of food, potentially reducing bloating. Cost: $10-$30 for a bottle of 30-60 capsules.
- Antibiotics: In cases of bacterial overgrowth, antibiotics may be prescribed. Cost varies depending on the specific antibiotic.
Surgical Procedures:
- Surgical intervention is typically not necessary for abdominal distension unless it is caused by an underlying condition that requires surgical management.
- In such cases, the cost of the procedure will vary depending on the specific condition and the healthcare facility. It is recommended to consult with a surgeon for a more accurate cost estimate.
Alternative Interventions
- Probiotics: May help restore the balance of gut bacteria and alleviate symptoms. Cost: $10-$30 for a bottle of 30-60 capsules.
- Herbal teas: Chamomile, peppermint, or ginger teas may provide relief from abdominal discomfort. Cost: $5-$10 for a box of 20-30 tea bags.
- Acupuncture: May help improve digestion and reduce abdominal distension. Cost: $60-$120 per session.
- Yoga and relaxation techniques: Can help reduce stress and promote healthy digestion. Cost: Varies depending on the location and instructor.
- Dietary modifications: Avoiding trigger foods, such as those high in FODMAPs, may help reduce bloating. Cost: Varies depending on individual food choices.
Lifestyle Interventions
- Eat smaller, more frequent meals to prevent overeating.
- Chew food thoroughly and eat slowly to aid digestion.
- Avoid carbonated beverages and chewing gum, as they can contribute to gas production.
- Stay hydrated by drinking an adequate amount of water throughout the day.
- Engage in regular physical activity to promote healthy digestion and reduce bloating.
- Manage stress through techniques such as meditation, deep breathing exercises, or yoga.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – D25 Abdominal distension (ICD-10:R14)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 2 (Prostate & Uterus) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 1 (Infection) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 3 (Kidney, Liver & Spleen) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Abdominal distension effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Abdominal distension. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Medindia.net. (n.d.). Abdominal Distension – Causes, Symptoms, Diagnosis, Treatment. Retrieved from https://www.medindia.net/health/conditions/abdominal-distension.htm
- Cleveland Clinic. (2021, September 30). Abdominal Distension (Distended Abdomen). Retrieved from https://my.clevelandclinic.org/health/symptoms/21819-abdominal-distension-distended-abdomen
- World Organization of Family Doctors (WONCA). (2015). International Classification of Primary Care (ICPC-2). Retrieved from https://www.globalfamilydoctor.com/site/DefaultSite/filesystem/documents/Groups/WICC/International%20Classification%20of%20Primary%20Care%20Dec16.pdf
- Centers for Medicare & Medicaid Services. (2018). ICD-10-CM Code R14 – Flatulence and related conditions. Retrieved from https://www.aapc.com/codes/icd-10-codes/R14
- Patient.info. (2023, September 28). Abdominal Distension and Bloating. Retrieved from https://patient.info/doctor/abdominal-distension-and-bloating
- Aakjær Andersen, C., et al. (2020). Diagnostic coding patterns in general practice between 2008 and 2015: a study from the Danish General Practice Database. BMJ Open, 10(9), e037664. Retrieved from https://bmjopen.bmj.com/content/bmjopen/10/9/e037664/DC4/embed/inline-supplementary-material-4.pdf?download=true
- Centers for Medicare & Medicaid Services. (2018). ICD-10-CM Code R14.0 – Abdominal distension (gaseous). Retrieved from https://www.aapc.com/codes/icd-10-codes/R14.0
- Wikipedia. (2023, May 23). Abdominal distension. Retrieved from https://en.wikipedia.org/wiki/Abdominal_distension
- Ministry of Health, Cyprus. (n.d.). ICPC-2 – English. Retrieved from https://www.gesy.org.cy/el-gr/annualreport/icpc-2-english1-10.pdf
- Unbound Medicine. (2018). R14.0 – Abdominal distension (gaseous). Retrieved from https://www.unboundmedicine.com/icd/view/ICD-10-CM/897955/all/R14_0___Abdominal_distension__gaseous_
Related articles
Made in USA